Larynx
The larynx is the primary organ for voice production which provides protection from aspiration and contributes to the clearing of secretions.
26-1 Injection Laryngoplasty
Indications
1. Vocal fold paralysis/immobility resulting in aspiration or dysphonia.
2. Glottic insufficiency resulting in aspiration or dysphonia.
Relative Contraindication
Medical contraindication to anesthesia
Preoperative Evaluation
1. If the etiology of the vocal fold immobility is unclear (i.e., no known history of cardiac surgery, tumor resection, extracorporeal membranous oxygenation [ECMO], etc.), then obtain magnetic resonance imaging (MRI) of the brain, neck, and chest.
2. Medical clearance for anesthesia
3. Modified barium swallow or a functional endoscopic evaluation of swallowing (FEES) to evaluate swallowing and confirm aspiration
4. Laryngoscopy/stroboscopy to evaluate vocal fold motion
5. Discussion that the injection is a temporary measure and that there are short-term injections and longer-term injections, lasting 2–3 months and 1–2 years, respectively.
Operative Technique
1. Informed parental consent is obtained, and the off-label use of injection material in children is discussed.
2. General anesthesia is administered; spontaneous ventilation is recommended with no indwelling endotracheal tube. Topical lidocaine, 2%, is sprayed. After the initial evaluation, a deeper plane of anesthesia may be needed to avoid laryngospasm. Insufflation can be performed via an endotracheal tube placed into the hypopharynx.
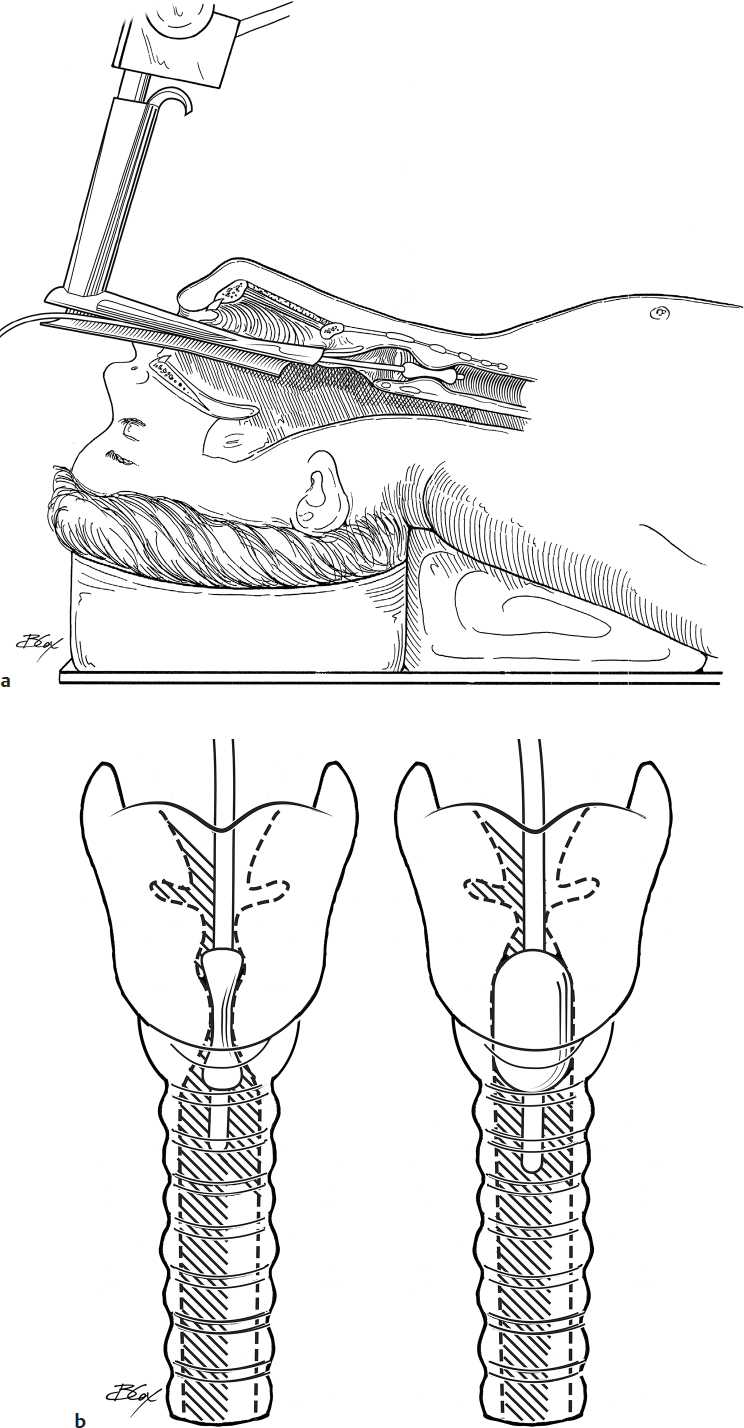
3. A suspension laryngoscope is inserted and placed either in the vallecula or in the glottic introitus, depending on the ability to properly expose the larynx.
4. A microscope is brought into view (a telescope rod can be used as well) to visualize the vocal folds. Palpate the vocal folds to assess for other lesions that may contribute to dysphonia. Palpate the interarytenoid area to rule out arytenoid fixation as an etiologic factor in the immobility that is seen.
5. A sterile-packaged injection material is utilized. Depending on the goals, short-term and long-term injection materials are available. The technique is the same regardless of the type of injection used. Fat and Gelfoam (Pfizer) injections are also possible (the preparation of those is not described here).
6. A needle is used transorally to place the injection. A long transoral needle (provided with some injection materials), a bruning syringe (pressurized syringe), or a 25-gauge butterfly needle that is grasped with a cupped forceps (make sure to cut the flanges so that it can fit through the laryngoscope) can be used.
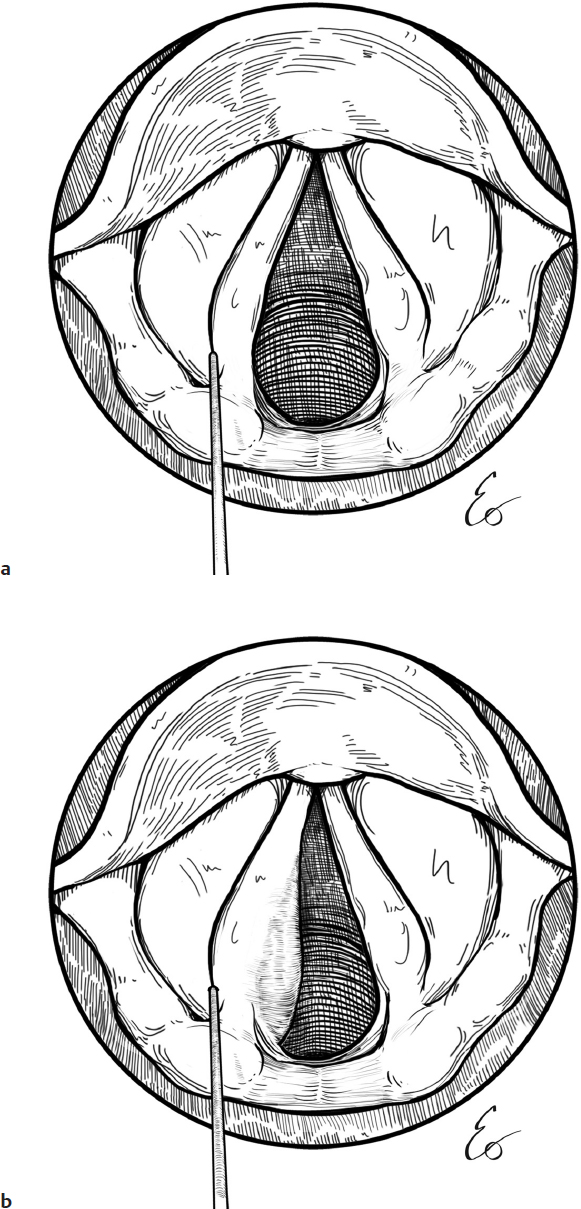
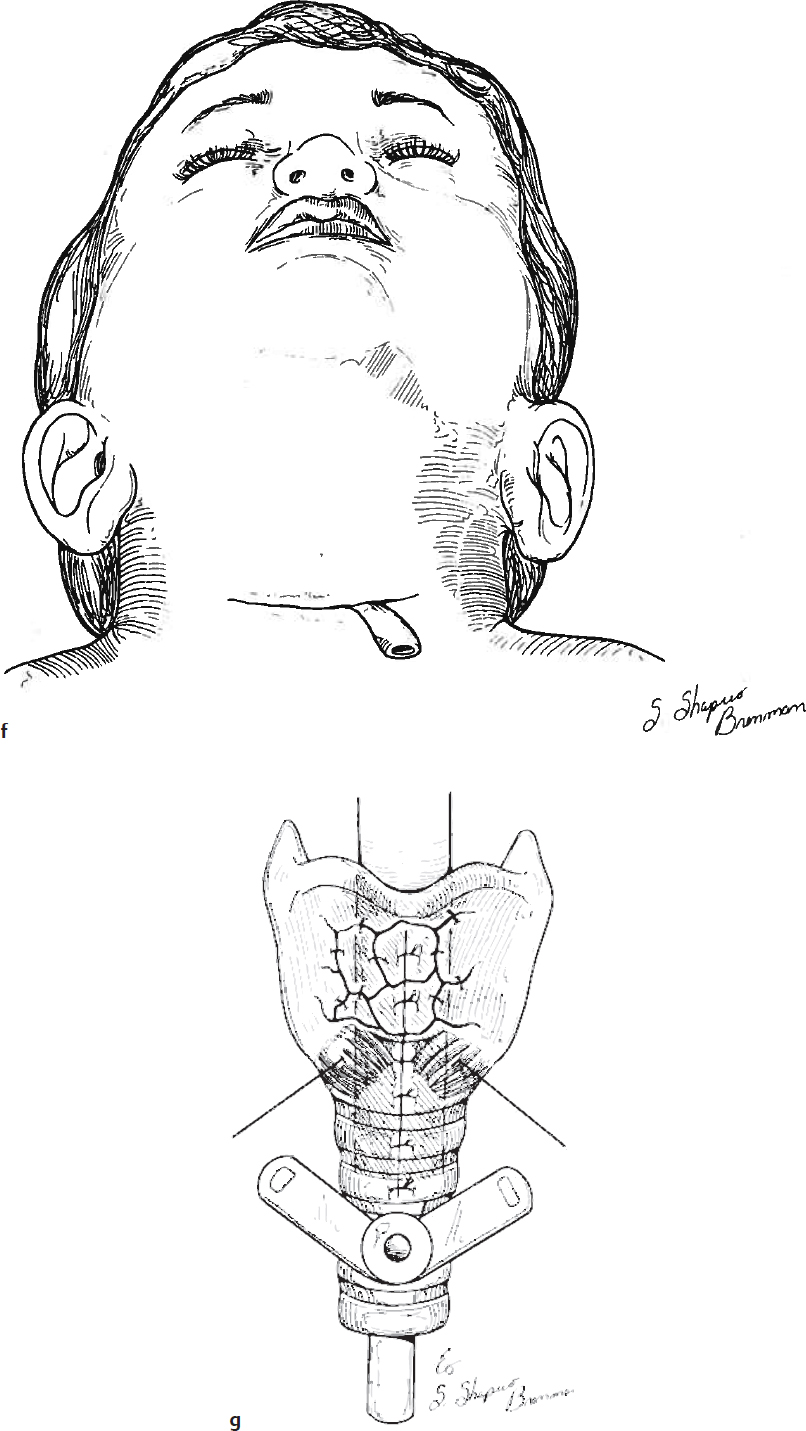
7. Inject anterior and lateral to the affected vocal process of the arytenoid (Fig. 26.1a).
8. Make sure not to place the needle too deep so the material does not extrude intraluminally. Visualize the medial/inferior surface of the vocal fold to ensure no extrusion of the needle or material. You will see the plumping of the vocal fold with gentle continuous pressure of the plunger (Fig. 26.1b).
Discharge Instructions
1. No significant limitations are needed.
2. No dietary restrictions are needed.
3. Remind the family that the voice will likely be more strained for the first 2 weeks after the procedure.
4. In very young children, mild stridor may be heard, although this is not commonly an issue.
Complications
1. Anesthesia
2. Lack of response of voice/swallowing to the injection
3. Fibrosis/foreign body reactions reported with some injection materials
26-2 Recurrent Laryngeal Nerve Reinnervation
Indications
1. Persistent vocal fold paralysis after injury to the recurrent laryngeal nerve
2. Intact donor nerve
Relative Contraindications
1. Inability to identify a recurrent laryngeal nerve stump
2. Extensive neck scarring
3. High vagal injury (unknown at this time)
Preoperative Evaluation
If the etiology of the vocal fold immobility is unclear (i.e., no known history of cardiac surgery, tumor resection, ECMO, etc.), then obtain an MRI of the brain, neck, and chest.
Operative Technique
1. A laryngeal electromyography (EMG) is obtained intraoperatively to confirm the asymmetric function of the thyroarytenoid muscle (TA), supporting the clinical opinion of a persistently paralyzed vocal fold.
2. The procedure is often performed in conjunction with a temporary vocal fold injection using rapidly resorbing filler material to allow for some improvement in the quality of the voice while the reinnervation takes effect (refer to Fig. 26.1a,b)
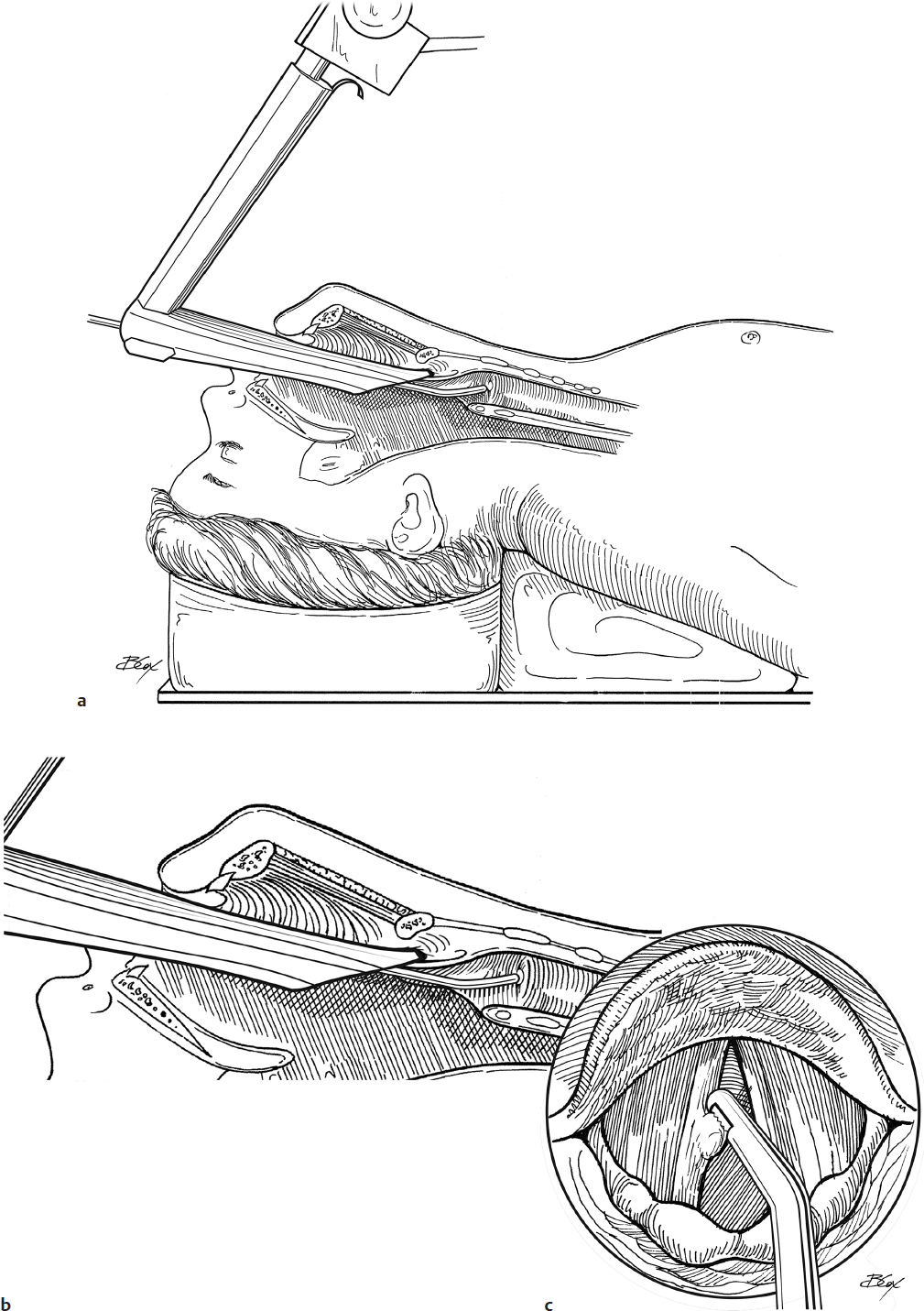
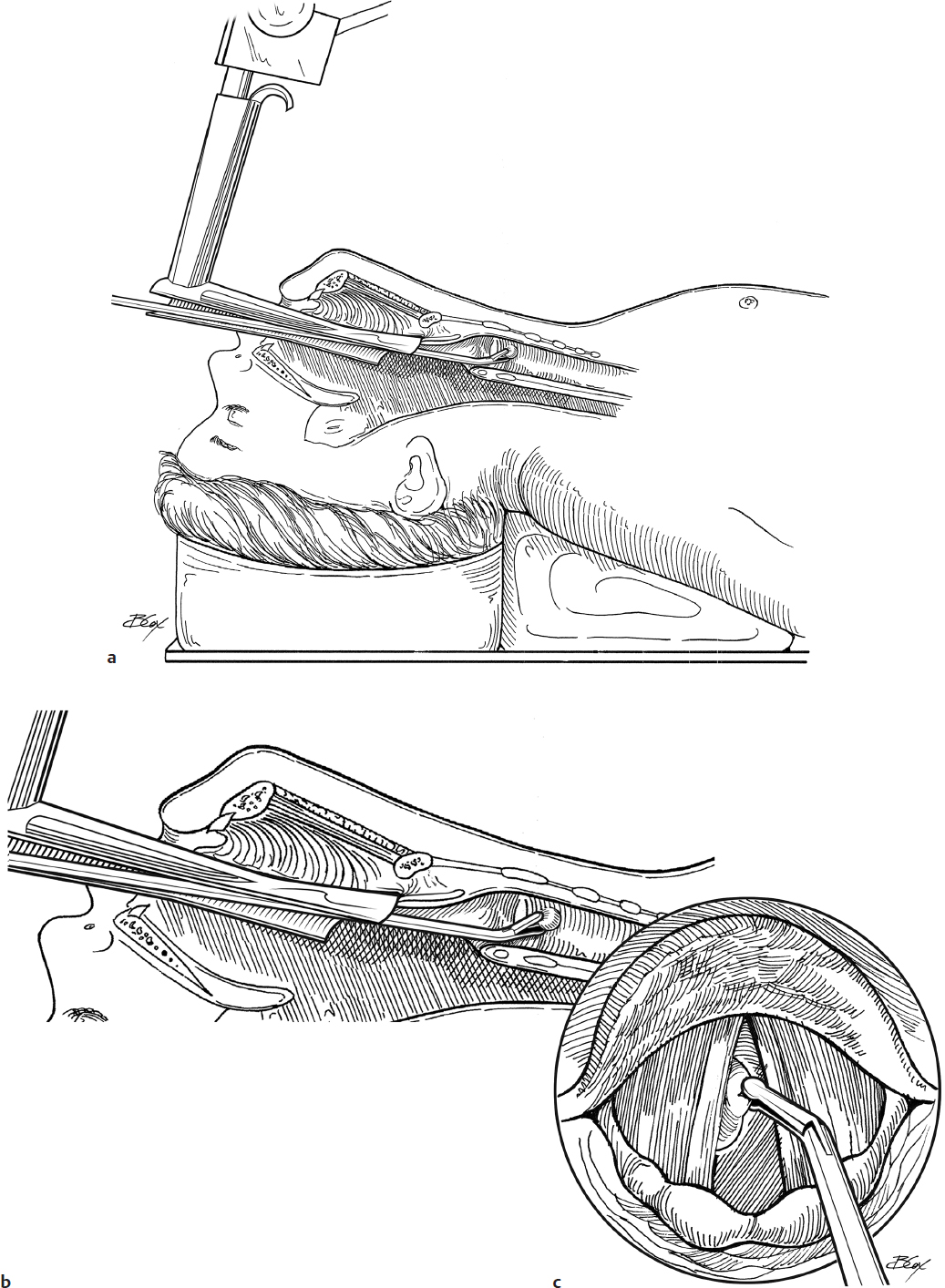
3. A small shoulder role is placed. The neck is prepared and draped in standard surgical fashion.
4. No paralysis is administered.
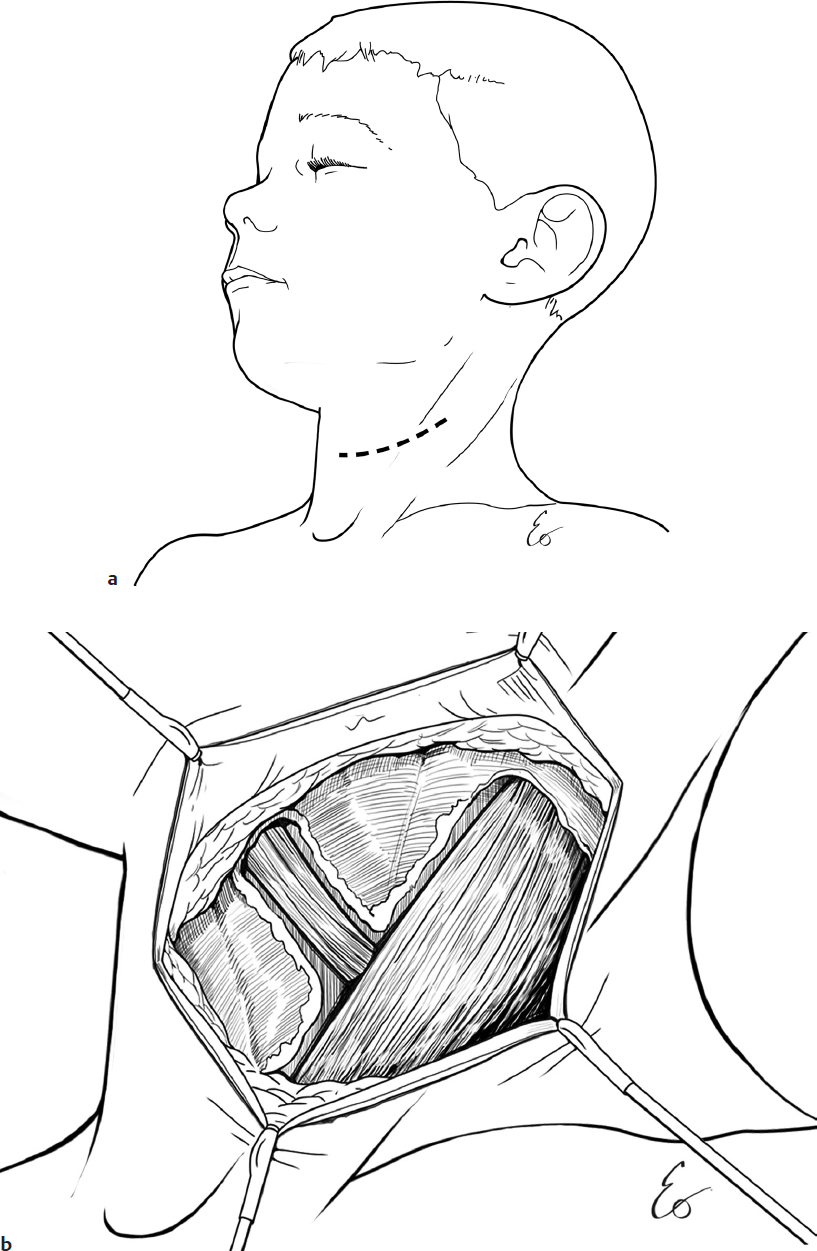
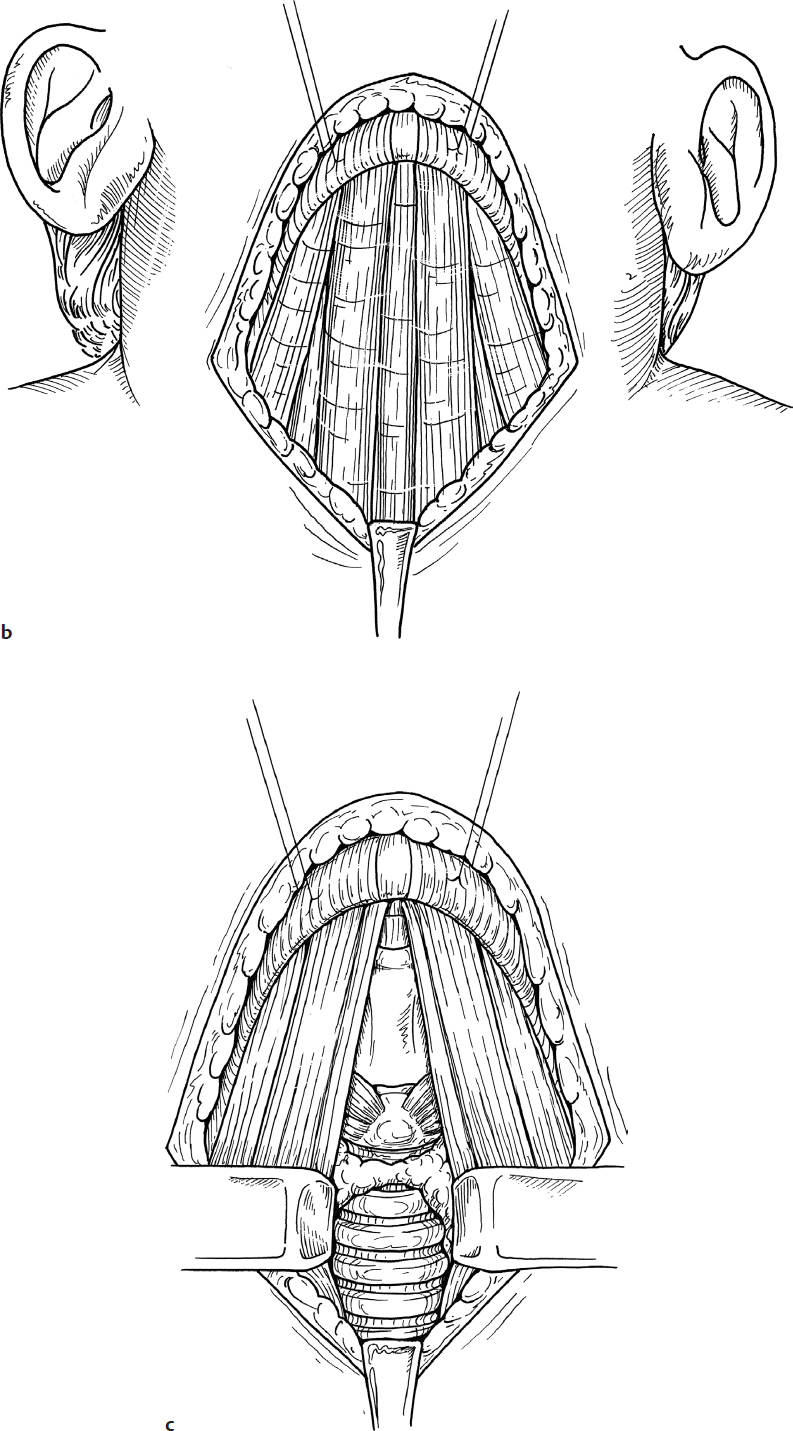
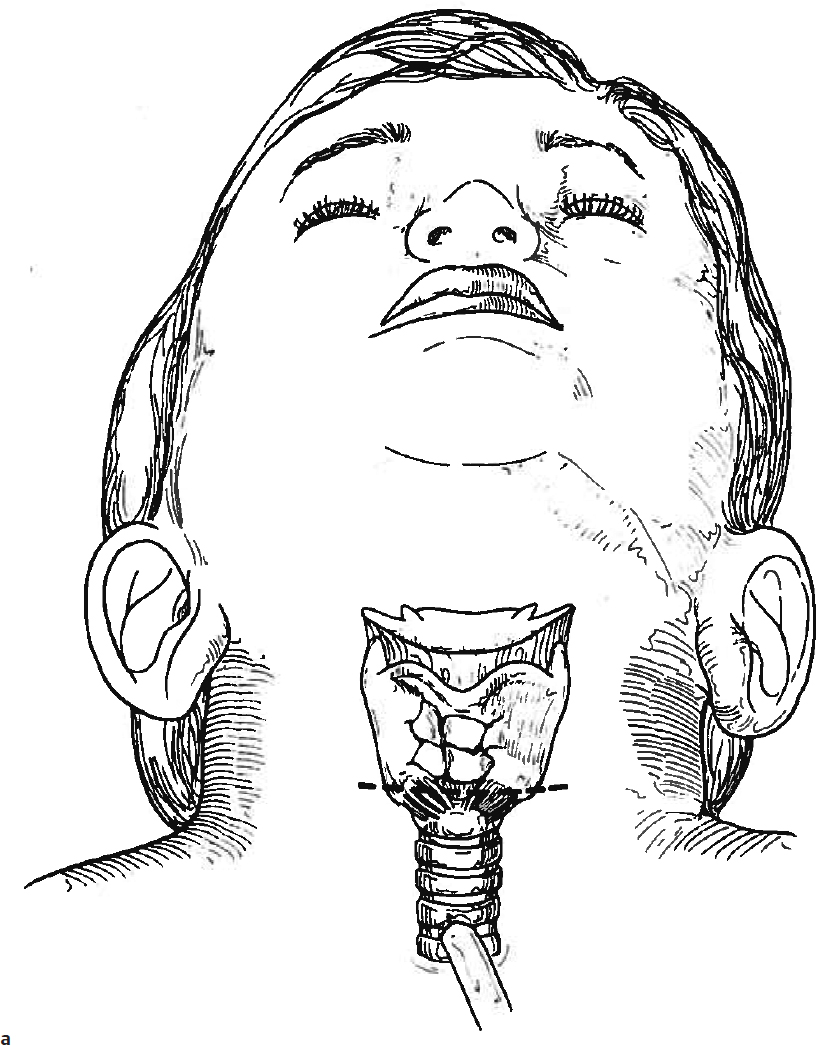
5. A curvilinear incision is fashioned such that the midpoint of the incision would lie over the portion of the sternocleidomastoid (SCM) muscle where the omohyoid muscle crosses the carotid sheath. The incision does not need to cross over the midline of the neck (Fig. 26.2a).
6. A no. 15 blade is used to incise the skin, and subplatysmal flaps are elevated superiorly and inferiorly and secured to the drapes.
7. The anterior border of the SCM muscle is identified and skeletonized (Fig. 26.2b).
8. The omohyoid muscle is identified as it crosses over the inferior extent of the SCM and partially skeletonized in order to allow it to be retracted inferiorly (Fig. 26.2b).
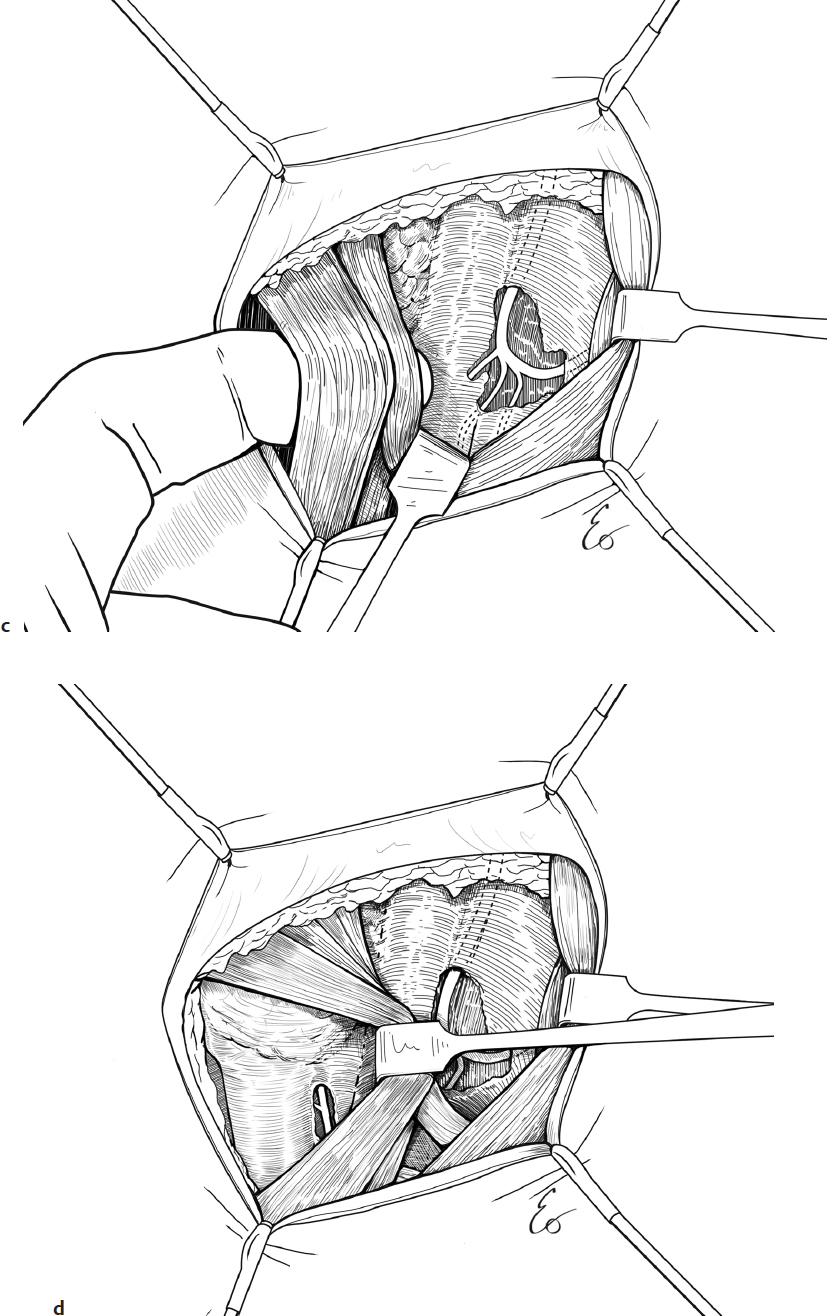
9. The ansa cervicalis nerve is identified overlying the internal jugular vein (IJV), and its inferior loop is localized. The branches emanating from the inferior loop (i.e., the omohyoid, sternohyoid, and sternothyroid branches) are identified and preserved (Fig. 26.2c).
10. If in doubt, a hand-held nerve stimulator can be used to stimulate the branches of the ansa cervicalis. Look for strap muscle twitches.
11. Next, attention is shifted to identifying the recurrent laryngeal nerve (RLN) as it courses in the tracheoesophageal groove.
12. Elevate the strap muscles from the thyroid gland and retract the muscles laterally (Fig. 26.2c,d).
13. Identify the inferior pole of the ipsilateral thyroid gland and dissect inferiorly/distally to it to localize the RLN (Fig. 26.2d).
14. If dissection does not allow for easy identification of the nerve, find the superior thyroid pole, and after ligating the vessels at its superior extent, reflect the superior pole inferiorly and medially to identify the RLN near the cricothyroid joint (CTJ). Be careful to avoid damage to the parathyroid glands.
15. Approximately 1–2 cm of RLN is needed for tension-free rotation and anastomosis.
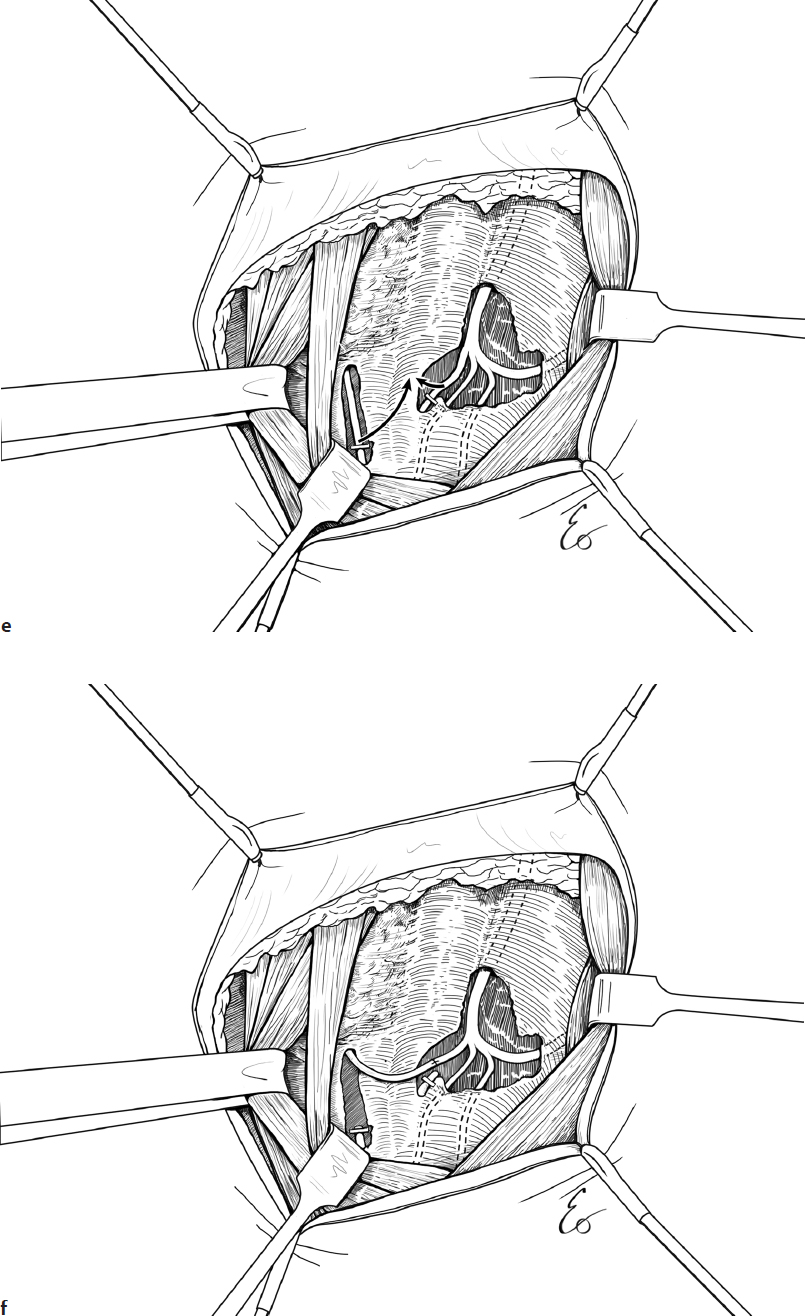
16. Next, the anastomosis will take place. Create a tunnel between the two compartments by elevating the strap muscles. Use a ¼-inch Penrose drain to retract the strap musculature medially and secure it to the drapes (Fig. 26.2e,f).
17. Determine which of the ansa cervicalis branches has the best size match to the caliber of the RLN, and transect that branch at a distal portion of it, allowing for tension-free rotation and anastomosis with the RLN (Fig. 26.2e,f).
18. Transect the RLN distally, again, allowing for tension-free arc rotation toward the lateral neck (Fig. 26.2e,f).
19. Use a sterile-draped microscope to perform the neurorrhaphy.
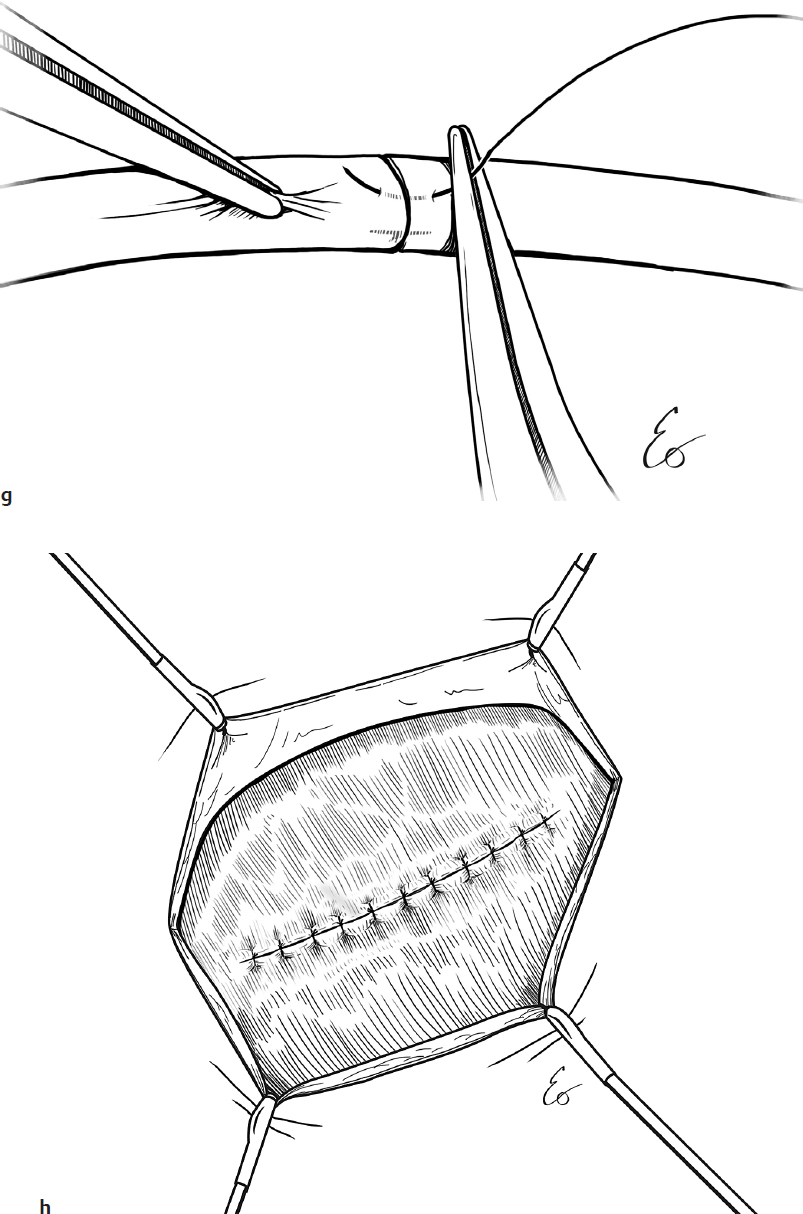
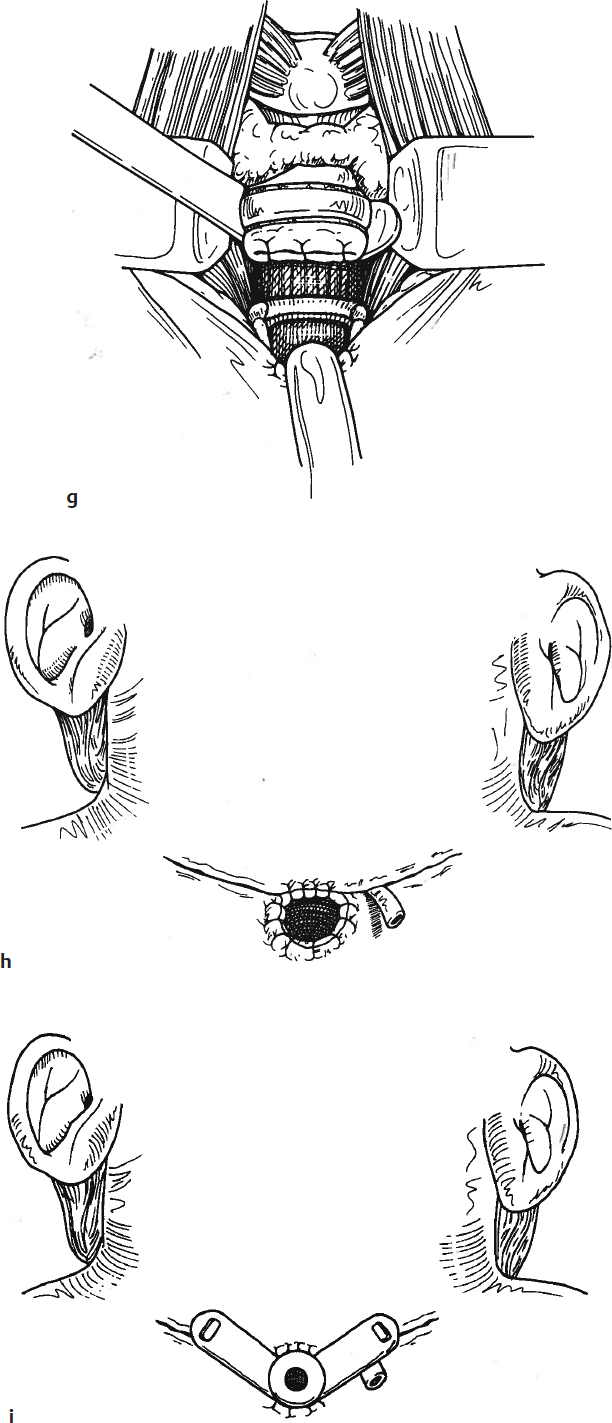
20. A BV100-4 9-0 monofilament nylon suture is used to approximate the epineurium at two points approximately 180 degrees apart. Microinstruments are utilized (Fig. 26.2g).
21. Lay the anastomosed nerves in a natural position under the strap muscles and remove the Penrose drain.
22. Optional: Place a Penrose drain superficial to the strap muscle tunnel. (No drain needed in most cases.)
23. Reapproximate the strap muscles and SCM with 4-0 Vicryl suture (Ethicon) in an interrupted fashion (Fig. 26.2h).
24. Reapproximate the platysma muscle with a 4-0 Vicryl suture in an interrupted fashion.
25. Skin closure is performed with 5-0 Monocryl suture (Ethicon), subcuticular closure.
26. Discharge home on day of surgery unless a drain was needed.
Discharge Instructions
1. No significant limitations are needed.
2. No dietary restrictions are needed.
3. Remind the family that the voice will likely begin to worsen about 2 months postop once the injection material resorbs, and then will hopefully gain more power at least 3 months postoperatively when the reinnervation begins to take effect.
Complications
1. Wound infection
2. Lack of improvement of the voice
3. Airway obstruction
26-3 Laryngotracheal Separation
Introduction
Laryngotracheal separation is a rarely performed procedure that serves as a definitive management option for severe, intractable aspiration secondary to laryngeal incompetence.
Indications
Laryngotracheal separation is indicated for severe, life-threatening aspiration and for progressive pulmonary complications. Given that the procedure results in the complete loss of voice, it should only be considered when alternative medical and surgical options have been exhausted.
Preoperative Evaluation
Office evaluation of patients with aspiration should include a head and neck history and physical examination, focusing on vocal quality, airway complaints, and feeding issues. A multidisciplinary evaluation is paramount and should include assessments from pulmonology, gastroenterology, speech therapy, respiratory therapy, social work, and occasionally neurology. Flexible fiberoptic laryngoscopy should be performed, assessing laryngeal structure and function. Aspiration should be confirmed by modified barium swallow and/or a functional endoscopic evaluation of swallowing. Reflux management, aggressive swallow therapy, and alternate feeding strategies are indicated prior to surgical consideration.
Operative Technique
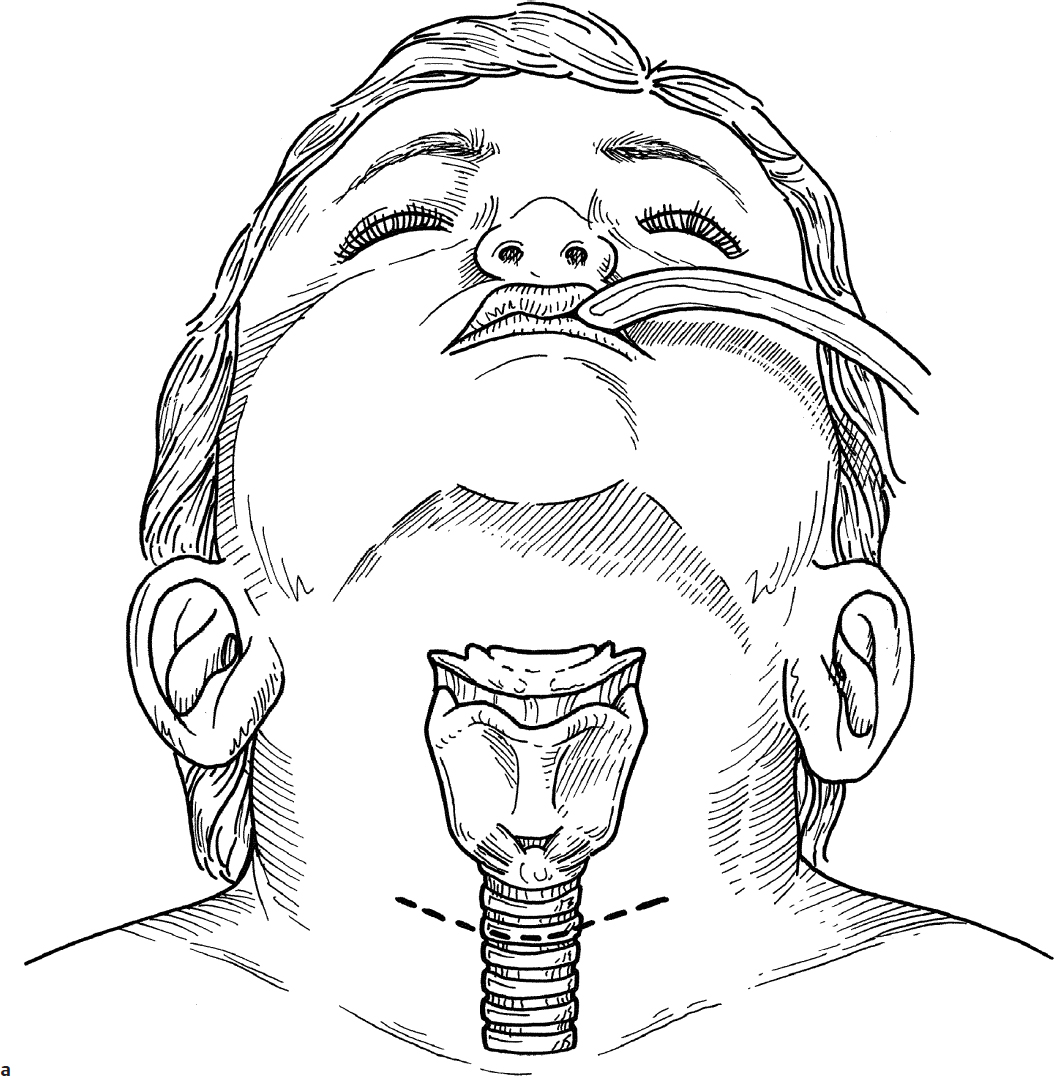
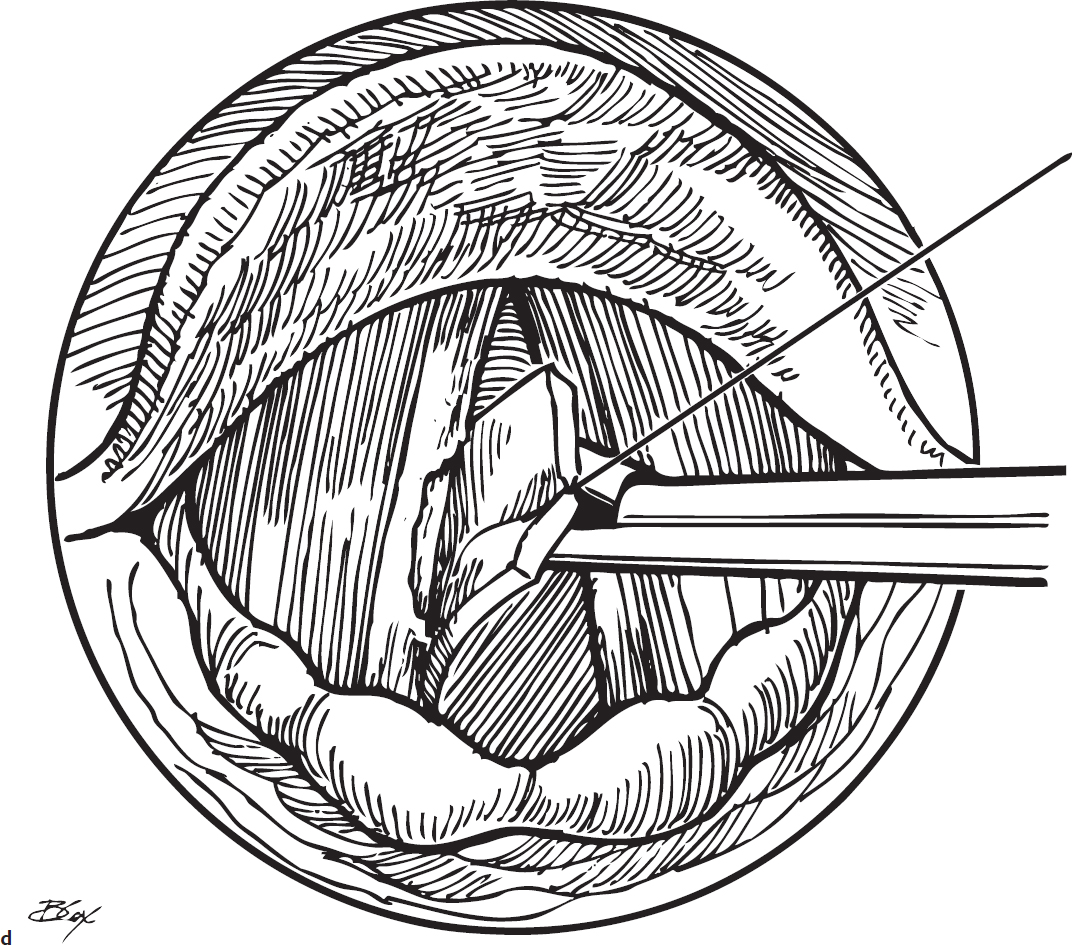
1. Laryngeal diversion is performed using general anesthesia with an endotracheal tube in place.
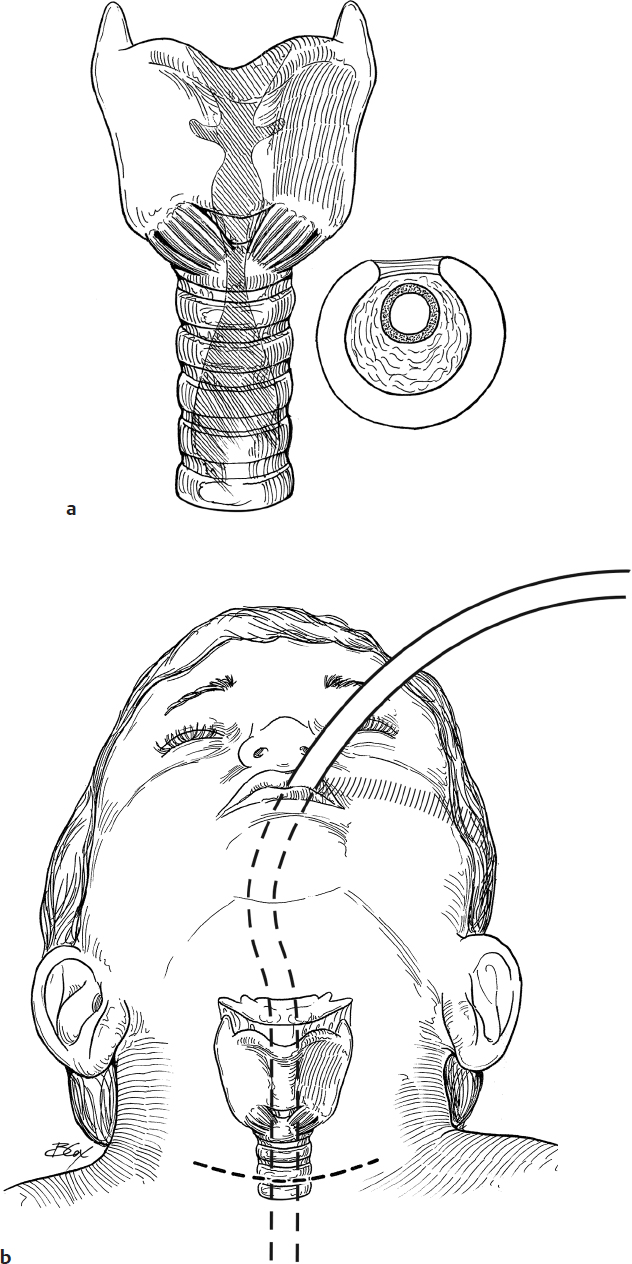
2. The patient is positioned on a shoulder roll with the neck extended as for tracheotomy (see Section 25-1).
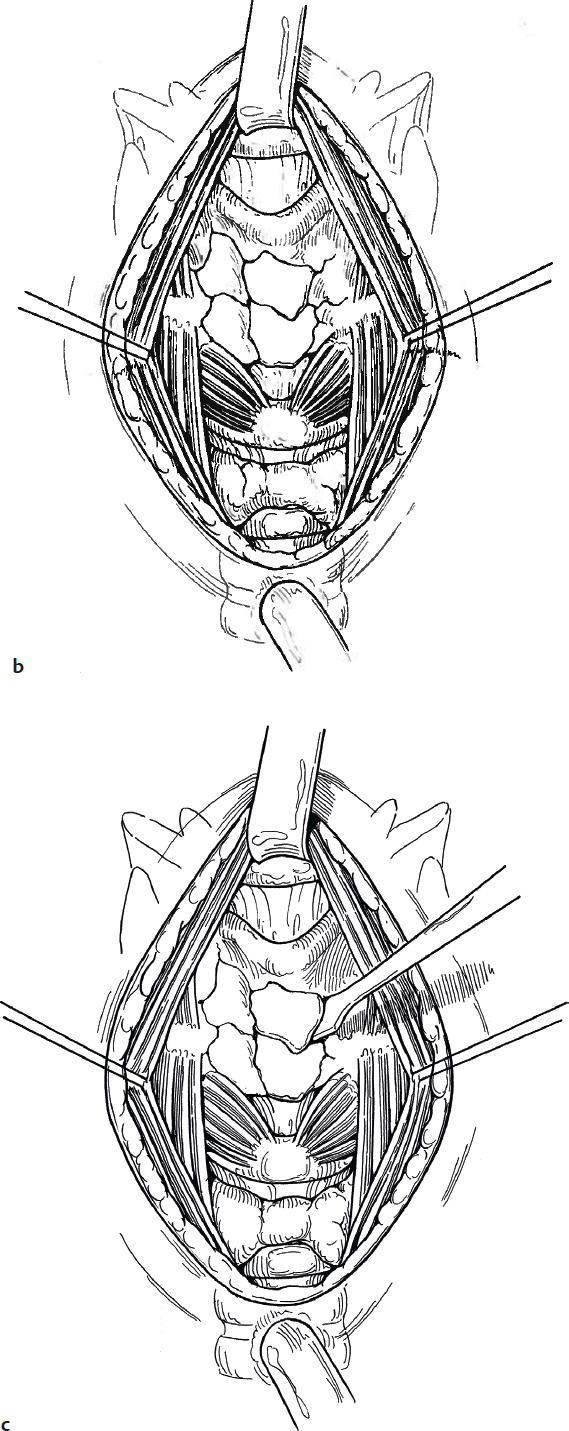
3. A horizontal skin incision is made halfway between the cricoid and the sternal notch (Fig. 26.3a). One percent lidocaine with 1:100,000 epinephrine is injected subcutaneously at the site of the incision to aid in hemostasis.
4. Subcutaneous fat and tissue are reflected with a clamp, exposing the deep cervical fascia overlying the strap muscles, and ribbon retractors are placed to expose the field as well as stabilize the trachea in the midline (Fig. 26.3b); 3-0 silk sutures may be used to stabilize the superior flap.
5. Vertical dissection with a scissors and clamp in the midline is carried out until the trachea is exposed. After the trachea is exposed, the strap muscles are separated in the midline to expose the cricoid and thyroid cartilage (Fig. 26.3c).
6. The trachea is transected between the fourth and fifth rings horizontally, sloping the incision superiorly (Fig. 26.3d).
7. The oral endotracheal tube is removed, and a reinforced endotracheal tube with a microcuff is placed into the stoma to facilitate ventilation during the completion of the operation.
8. The trachea is mobilized inferiorly from the tracheoesophageal septum (Fig. 26.3e).
9. The anterior edge of the trachea is sutured to the inferior edge of the skin incision with 4-0 Prolene suture (Ethicon) (Fig. 26.3f).
10. The upper stump of the trachea is mobilized from the tracheoesophageal septum and then closed with 3-0 Prolene suture, creating a blind pouch (Fig. 26.3g).
11. A Penrose drain is placed in the wound.
12. The subcutaneous tissues are closed with 4-0 interrupted Vicryl, and the skin is closed with 4-0 running subcuticular Vicryl. The central portion of the upper skin flap is sutured to the posterior tracheostoma with 4-0 interrupted Prolene (Fig. 26.3h).
13. The endotracheal tube is removed from the newly created stoma, and an appropriate-sized tracheostomy tube is secured in place (Fig. 26.3i).
Complications
1. Tracheocutaneous fistula
2. Recurrent aspiration through a persistent fistula
3. Wound infection
4. Hematoma
5. Seroma
26-4 Excision of Laryngeal Papillomas, Polyps, and Granulomas
Introduction
Laryngeal papillomas are rare, benign tumors that occur rarely in children and are the result of mucosal infection with the human papillomavirus (HPV). Laryngeal polyps and granulomas are inflammatory lesions that arise in the larynx secondary to trauma (usually intubation) and/or reflux.
Indications
Laryngeal papillomas are frequently recurring lesions that require excision when they cause dysphonia and/or airway obstruction. Laryngeal polyps and granulomas rarely require excision. Surgery may be considered for symptomatic lesions that fail to respond to voice therapy, reflux management, and vocal hygiene measures.
Preoperative Evaluation
Office evaluation of patients with these benign laryngeal lesions should include a head and neck history and physical examination, focusing on vocal quality and airway complaints. Flexible fiberoptic laryngoscopy should be performed, assessing laryngeal structure and function. Reflux management and/or voice therapy are often indicated and may be complementary to surgery.
Operative Technique
1. After induction of general anesthesia, spontaneous ventilation is maintained using appropriate anesthetic technique. Alternatively, the procedure may be performed using apneic technique with intermittent endotracheal intubation.
2. An appropriately sized Lindholm laryngoscope is inserted into the vallecula and suspended, exposing the larynx (Fig. 26.4a,b).
3. Visualizing through the operative microscope, the lesion is excised using a laryngeal microdebrider skimmer blade, taking care to preserve the underlying normal tissue. Alternatively, a CO2 laser may be used (standard laser precautions need to be applied) (Fig. 26.4c).
4. Occasionally, a biopsy is indicated in order to assess for laryngeal dysplasia. A cup forceps is used to obtain the specimen.
5. Hemostasis, if necessary, is obtained by the application of oxymetazoline-soaked pledgets (Fig. 26.4d).
6. If tracheobronchial disease is suspected, a rigid telescope may be used to assess the distal airway. Tracheobronchial papillomas may be removed using a longer microdebrider blade under telescopic guidance.
Complications
1. Laryngeal scar
2. Recurrence of the lesion
3. Voice dysfunction
4. Airway obstruction
5. Injury to the oral cavity, oropharynx, or airway
6. Pneumonia
7. Pneumothorax
8. Laser-induced burns or fire
26-5 Excision of Subglottic Cysts
Introduction
Subglottic cysts are uncommon lesions usually presenting in children who have had a prior history of intubation. Commonly, subglottic cysts present with coexisting subglottic stenosis. Subglottic cysts may be single or multiple.
Indications
Subglottic cysts require excision or marsupialization when they cause airway obstruction.
Preoperative Evaluation
Office evaluation of patients with subglottic cysts should include a head and neck history and physical examination, focusing on airway complaints. Patients typically present with a variable degree of biphasic stridor, which may be exacerbated when the patient develops an upper respiratory tract infection or when crying. Flexible fiberoptic laryngoscopy should be performed, assessing laryngeal structure and function. Reflux management is often indicated and may be complimentary to surgery.
Operative Technique
1. After induction of general anesthesia, spontaneous ventilation is maintained using appropriate anesthetic technique. Alternatively, the procedure may be performed using apneic technique with intermittent endotracheal intubation.
2. An appropriately sized Benjamin laryngoscope is inserted into the vallecula and suspended, exposing the larynx (Fig. 26.5a).
3. Visualizing through the operative microscope or 0-degree telescope, the cyst is unroofed using a cup forceps (Fig. 26.5b,c). The lesion may be further excised using a laryngeal microdebrider skimmer blade, taking care to preserve the underlying normal tissue. Alternatively, a CO2 laser may be used to marsupialize the lesion (standard laser precautions need to be applied).
4. If the patient has coexisting subglottic stenosis, dilatation using an appropriate sized balloon may be performed.
5. Hemostasis, if necessary, is obtained by the application of oxymetazoline-soaked pledgets.
6. If tracheobronchial disease is suspected, a rigid telescope may be used to assess the distal airway.
Complications
1. Laryngeal scar
2. Recurrence of the lesion
3. Voice dysfunction
4. Airway obstruction
5. Injury to the oral cavity, oropharynx, or airway
6. Pneumonia
7. Pneumothorax
8. Laser-induced burns or fire
26-6 Balloon Laryngoplasty
Introduction
Subglottic stenosis is an uncommon complication, occurring in children who have had a prior history of intubation. Balloon dilatation is an endoscopic technique used to apply radial force in an effort to expand the narrowed airway.
Indications
Balloon laryngoplasty is indicated for patients with acquired subglottic stenosis presenting with signs and symptoms of airway obstruction. The technique may also be used to address restenosis in patients who have undergone laryngotracheal reconstruction. Balloon laryngoplasty is often performed with adjunctive procedures, including division of scar tissue, topical application of mitomycin C, or removal of granulation tissue or cysts.
Preoperative Evaluation
Office evaluation of patients with subglottic stenosis should include a head and neck history and physical examination, focusing on airway complaints. Patients typically present with a variable degree of biphasic stridor, which may be exacerbated when the patient develops an upper respiratory tract infection or when crying. Flexible fiberoptic laryngoscopy should be performed, assessing laryngeal structure and function. Reflux management is often indicated and may be complimentary to surgery.
Operative Technique
1. After induction of general anesthesia, spontaneous ventilation is maintained using appropriate anesthetic technique. Alternatively, the procedure may be performed using apneic technique with intermittent endotracheal intubation.
2. An appropriately sized Benjamin laryngoscope is inserted into the vallecula and suspended, exposing the larynx.
3. The larynx is visualized using the 0-degree telescope, and the degree of stenosis is assessed.
4. An appropriately sized balloon (5–14 mm) is selected and inserted into the stenotic segment and centered. The balloon is inflated using a syringe with a pressure gauge, with care taken to stay below the burst pressure of the balloon (indicated on the packaging). With certain balloons, oxygen may be delivered through a separate port for the duration of balloon inflation (Fig. 26.6a,b).
5. The balloon is deflated once the saturation drops below 92%, and the airway is reassessed with repeat dilatation, if necessary.
6. The distal airway is then evaluated using the telescope.
7. The decision to intubate or leave the patient extubated postoperatively should be individualized to the patient’s needs.
Complications
1. Laryngeal scar
2. Recurrence of the stenosis
3. Voice dysfunction
4. Airway obstruction
5. Rupture of airway
6. Pneumonia
7. Pneumothorax
26-7 Repair of Laryngeal Fracture
Introduction
Laryngeal fractures in children usually occur from a direct blow to the neck resulting from a “clothesline injury” or a motor vehicle accident. Patients may arrive at the emergency department intubated, tracheotomized, without a secure airway, and with significant endolaryngeal mucosal injuries.
Indications
Displaced laryngeal fractures require treatment (i.e., reduction) to avoid laryngeal stenosis and airway obstruction.
Preoperative Evaluation
Standard cervical and chest radiographs are obtained to rule out associated injuries. Computed tomography (CT) scan of the larynx helps delineate the fractures. Flexible laryngoscopy should be performed in the awake, unintubated patient. Direct laryngoscopy and bronchoscopy define the configuration of the lumen and identify other laryngeal pathology, including vocal fold injuries, hematoma, and arytenoid dislocation.
Operative Technique
1. Reduction of a laryngeal fracture is performed under general anesthesia administered either through an endotracheal tube or an oral RAE tube placed in a tracheostoma.
2. One percent lidocaine with 1:100,000 epinephrine is injected subcutaneously at the site of the incision to aid in hemostasis.
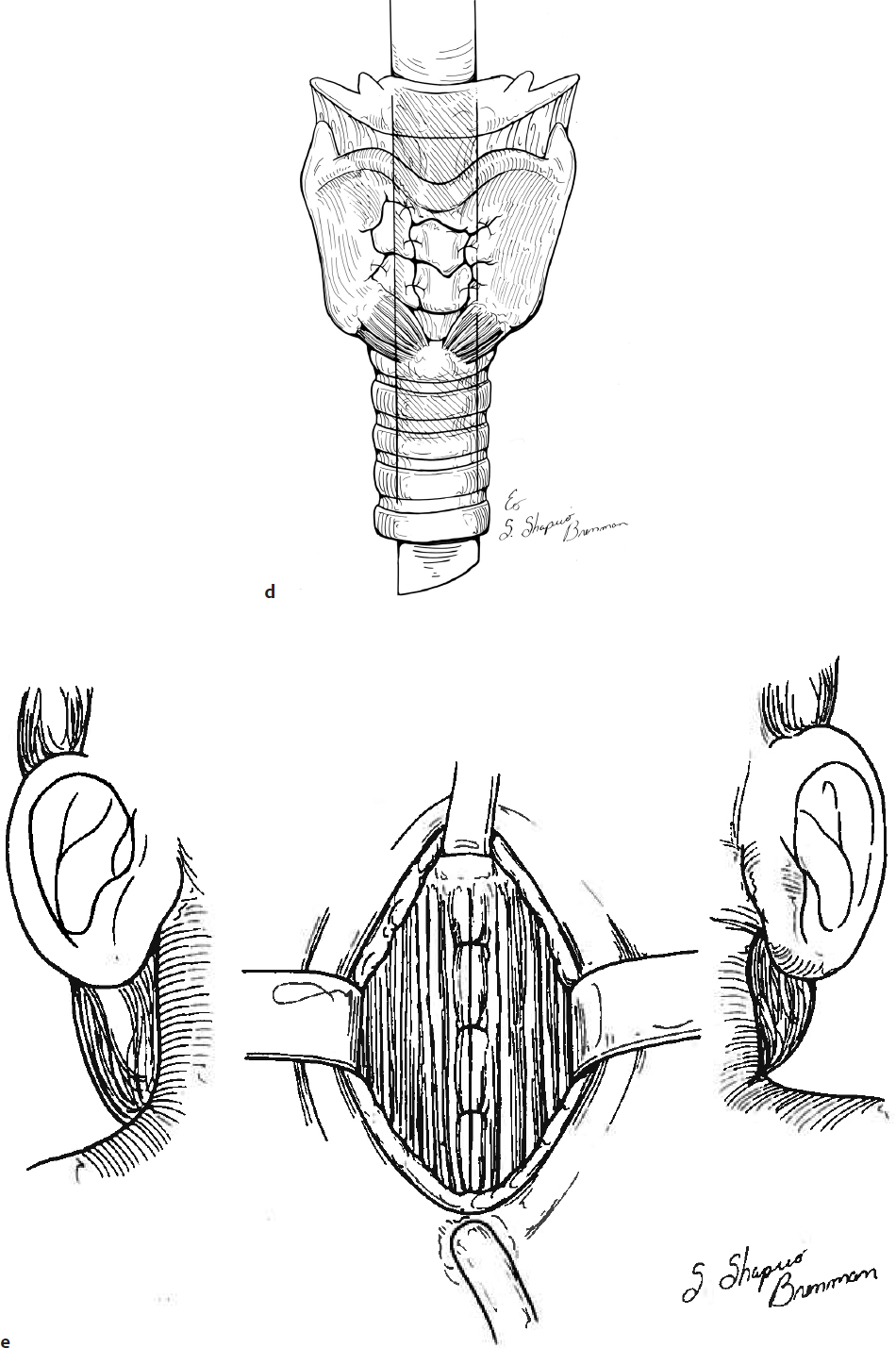
3. A transverse incision is made at the level of the cricothyroid membrane down to the strap muscles (Fig. 26.7a).
4. A superior skin flap is elevated to the level of the hyoid bone. An inferior skin flap is elevated, exposing the strap muscles over the upper trachea (Fig. 26.7b).
5. The midline fascia is divided and the strap muscles are retracted laterally with 4-0 silk suture clamped with a hemostat; the thyroid lamina, cricoid cartilage, and trachea are thereby exposed (Fig. 26.7c).
6. Depressed thyroid cartilage fragments are aligned with a Cottle elevator (Fig. 26.7c).
7. If significant mucosal injury or vocal fold injuries were noted on endoscopy, a complete laryngofissure should be performed to expose these areas. Wounds should be reap-proximated using absorbable polydioxanone (PDS) or Vicryl suture (4-0 or smaller).
8. The cartilage fragments are sutured in place with 4-0 PDS suture (Fig. 26.7d).
9. If the thyroid lamina is ossified, small holes are drilled to hold the sutures.
10. The strap muscles are reapproximated in the midline with 4-0 Vicryl suture (Fig. 26.7e).
11. A Penrose drain is placed in the wound, and the subcutaneous tissue is closed with 4-0 Vicryl suture (Fig. 26.7f).
12. The skin is closed with 4-0 Vicryl suture.
13. Patients who do not have a tracheostomy tube in place should remain intubated with an endotracheal tube for 7–10 days. If a tracheotomy is in place, the oral RAE tube is removed and replaced with a tracheostomy tube, and an age-appropriate size Rutter stent or superior limb of a cut T-tube that has been oversewn to prevent aspiration is placed in the larynx (Fig. 26.7g).
14. Intravenous broad-spectrum antibiotics are continued until the drains and stents are removed after 7 days. The stent is removed by direct laryngoscopy and bronchoscopy.
15. If the cricoid cartilage is fractured, displaced, and comminuted, a decision to perform a cricotracheal resection (CTR) may be indicated (see Section 25-4).
16. If present, the tracheostomy tube may be removed when the upper airway lumen is sufficient to permit normal respiration.
Complications
1. Laryngeal stenosis
2. Dysphagia
3. Dysphonia
4. Aspiration
26-8 Laryngotracheoplasty with Thyroid Ala Graft
Introduction
Laryngotracheoplasty with thyroid alar cartilage graft (LTP-TAC) is a modification of the cricoid split procedure and is employed for patients with subglottic stenosis. In LTP-TAC, the expanded laryngotracheal framework is maintained with the interposition of a portion of the patient’s thyroid ala. The theoretical advantage of this procedure over the cricoid split without a cartilage graft is that it maintains the expansion and prevents inadvertent displacement of the endotracheal tube through the split segment.
Indications
The LTP-TAC procedure is indicated for patients with subglottic stenosis who meet the criteria for cricoid split (Fig. 26.8a). The patient should theoretically be extubatable with the expanded airway, avoiding the need for tracheostomy. In some centers, LTP-TAC is occasionally employed as an alternate to standard LTP (costal cartilage graft) in patients who have mild subglottic stenosis but are tracheostomy tube–dependent. It is also offered in patients who do not require intubation but have sufficient airway compromise to require surgical intervention for subglottic stenosis.
Preoperative Evaluation
In many cases, patients require intubation in the intensive care setting. Evaluation of these patients should include an assessment for candidacy (failed extubation attempts, adequate cardiopulmonary status, and controlled reflux). Microlaryngoscopy and bronchoscopy should be performed in order to assess the status of the airway.
Office evaluation of patients with known subglottic stenosis should include a head and neck history and physical examination, focusing on vocal quality, swallowing, and airway complaints. A multidisciplinary evaluation is paramount and should include assessments from pulmonology, gastroenterology, speech therapy, respiratory therapy, and social work. Flexible fiberoptic laryngoscopy should be performed, assessing laryngeal structure and function. Reflux management and/or voice therapy are often indicated and may be complementary to surgery.
Operative Technique
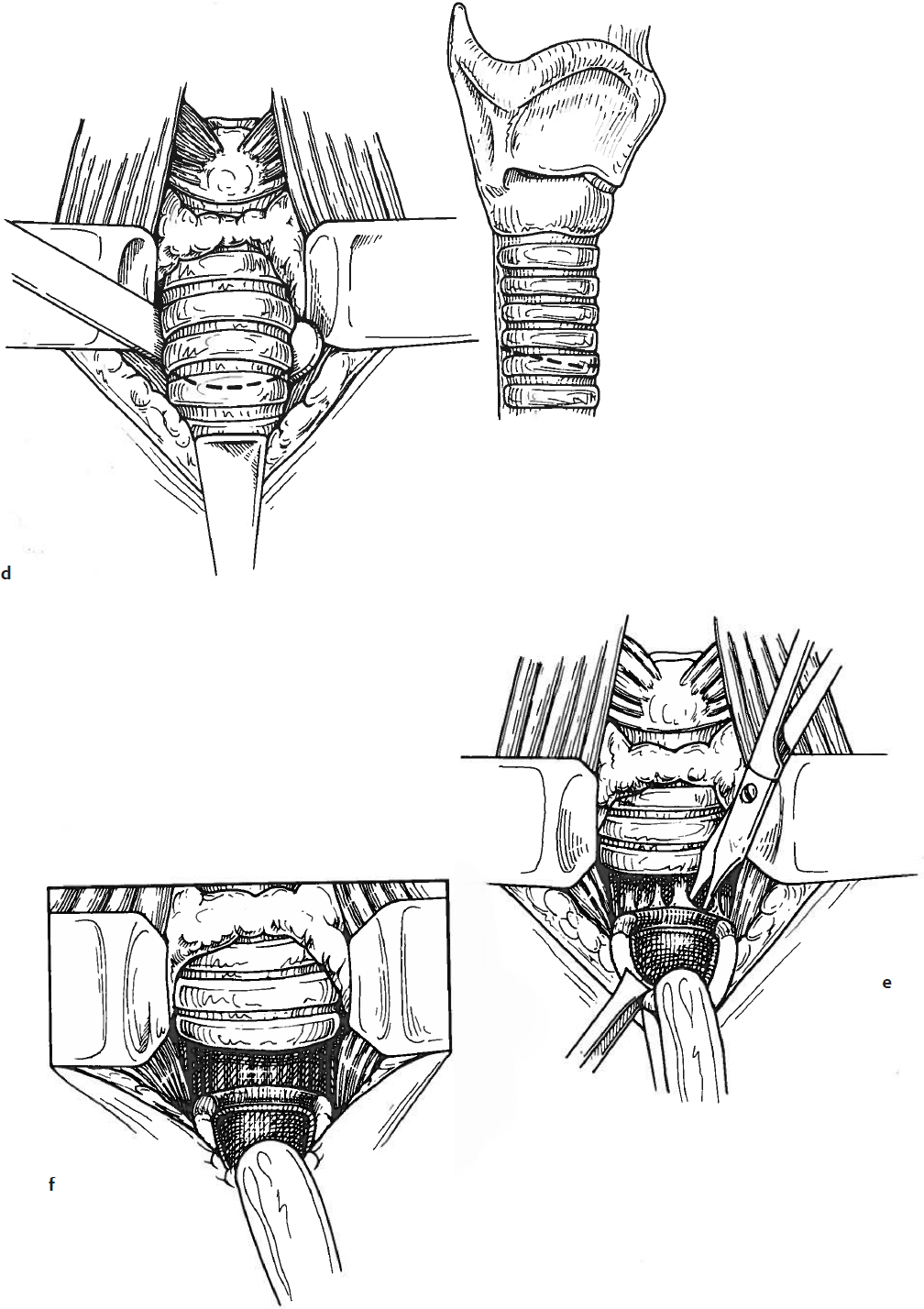
1. After induction of general anesthesia, the patient is positioned on a shoulder roll and a horizontal incision site is marked at the level of the cricoid cartilage (Fig. 26.8b).
2. Lidocaine (1%) with epinephrine (1:100,000) is injected into the subcutaneous tissue in order to facilitate hemostasis during the procedure.
3. The patient is then prepped and draped in order to maintain sterility during the procedure.
4. The incision is made using a no. 15 blade and carried through the platysma.
5. Superior and inferior subplatysmal flaps are then elevated using the Metzenbaum scissors and/or monopolar cautery to the level of the hyoid superiorly and to the third or fourth tracheal ring inferiorly. The flaps are secured using 3-0 silk sutures.
6. The strap muscles are divided in the midline using the Metzenbaum scissors and/or monopolar cautery, exposing the entire laryngeal framework, the thyroid gland, and the upper tracheal rings. The strap muscles may be secured using 3-0 silk sutures (Fig. 26.8c).
7. The thyroid gland is divided in the midline using the monopolar cautery.
8. A midline laryngotracheofissure is then performed using a fresh no. 15 blade and is to the midpoint of the thyroid ala superiorly and the upper two tracheal rings inferiorly (Fig. 26.8d).
9. The edges of the fissure are distracted using silk or Prolene sutures.
10. An appropriately sized nasotracheal tube is then inserted and placed with the tip beyond the fissure.
11. The upper edge of one of the thyroid ala is exposed using the tenotomy scissors and a small retractor. A 3–4 mm tear drop–shaped piece of the thyroid ala is then incised using a Beaver blade. The incised segment is carefully elevated off of the deep perichondrium using a single hook, Freer elevator, and/or scissors (Fig. 26.8e).
12. The graft is sutured into the laryngofissure using six to eight interrupted 4-0 or 5-0 PDS sutures (Fig. 26.8f).
13. A Valsalva maneuver is performed in order to assess for a leak, and Tisseel (Baxter) is occasionally applied to the suture line.
14. The strap muscles and platysmal layers are closed over a 0.25-inch Penrose drain using interrupted 4-0 Vicryl sutures.
15. The skin is closed using a running subcuticular 5-0 Monocryl suture.
16. The nasotracheal tube is secured to the columella using a 3-0 Prolene suture buttressed with a cut piece of a catheter to prevent suture erosion through the columella (Fig. 26.8g).
17. The drain is removed after 3 days and the patient extubated 4–7 days following the procedure. A pre-extubation endoscopy may be performed prior to extubation with exchange of the tube to an orotracheal route.
Complications
1. Recurrent subglottic stenosis
2. Voice dysfunction
3. Aspiration
4. Subcutaneous emphysema
5. Pneumonia
6. Pneumothorax
7. Endotracheal tube complications