Purpose
To observe the efficacy of deep anterior lamellar keratoplasty (DALK) for treatment of acute hydrops in keratoconus after anterior chamber paracentesis combined with thermokeratoplasty.
Design
Retrospective, noncomparative clinical case series.
Methods
Twenty-one patients (21 eyes) suffering acute hydrops associated with keratoconus were treated first by anterior chamber paracentesis combined with thermokeratoplasty. At 1 week after the edema was absorbed, and Descemet membrane ruptures and stromal clefts were cured, all patients received modified DALK. Descemet membrane re-ruptures during surgery were recorded, if any. Graft transparency, visual acuity, recipient folds or opacity, and immune rejection were monitored for 6 months to 1 year.
Results
All the corneal edema alleviated rapidly, and the intrastromal clefts narrowed within 1 week after combined anterior chamber paracentesis and thermokeratoplasty. DALK was performed successfully in all patients within 2 weeks after the first surgical procedure, with no Descemet membrane rebreaking or corneal perforation. The recipients were completely clear in 7 eyes, and mild fusiform scars appeared at the central recipient in 14 eyes. All the opacity of Descemet membrane ruptures became slight or even disappeared after 6 months. The mean best-corrected visual acuity was improved to 20/30 at 1 year after DALK. No immune rejection occurred.
Conclusions
Anterior chamber paracentesis combined with thermokeratoplasty can accelerate the absorption of corneal edema in patients with acute corneal hydrops (within 1 week) and Descemet membrane rupture healing without obvious opacity (within 2 weeks). During this window phase, DALK could be performed safely, and good visual acuity may be obtained.
Acute corneal hydrops occurs in approximately 3% of keratoconic eyes. Caused by leaking of aqueous through a tear in the Descemet membrane, it can lead to a sudden visual decrease and pain. In the natural course of the disease, an episode of acute corneal hydrops may take approximately 3–6 months for complete disappearance. Patients usually have low vision for a long period of time, during which serious complications such as corneal perforation may occur. Surgical intervention is required when corneal edema is not absorbed to avoid complications and achieve early visual rehabilitation. Intracameral injection of air or gas, such as perflouropropane (C3F8), is most common. However, the vision will still be influenced by the obvious scar in the central cornea. To remove the scar and improve the vision, penetrating keratoplasty may be needed.
With the development of microsurgery equipment and techniques, deep anterior lamellar keratoplasty (DALK), which avoids immune rejection that penetrating keratoplasty often encounters, has become generally accepted as the best choice for keratoconus in the advanced stage with large curvature. However, in patients with combined acute hydrops, regular DALK cannot be performed because Descemet membrane ruptures and intrastromal clefts may cause corneal perforation. Moreover, after the edema is naturally absorbed, the cornea will heal with obvious scarring and will not be suitable for DALK.
In this study, we tried to provide an opportunity for DALK for patients with corneal hydrops by anterior chamber paracentesis combined with thermokeratoplasty. The clinical efficacy was evaluated.
Methods
This retrospective case series study was approved by the Institutional Review Board of Shandong Eye Institute and followed the tenets of the Declaration of Helsinki. Twenty-one patients (21 eyes) with acute corneal hydrops in keratoconus who were treated by DALK within 2 weeks after onset at our institution from June 1, 2009 to July 31, 2012 were included. Thirteen patients were men and 8 patients were women. The mean age was 22 years (range, 13–36 years). All patients complained of spontaneous and sudden onset of pain, redness, reduced visual acuity, and epiphora in eyes within 3 days. Testing for visual acuity and intraocular pressure (IOP), slit-lamp examination, measurement of corneal curvature, corneal topography, and anterior segment optical coherence tomography (OCT) were performed to confirm the diagnosis of keratoconus with acute corneal hydrops.
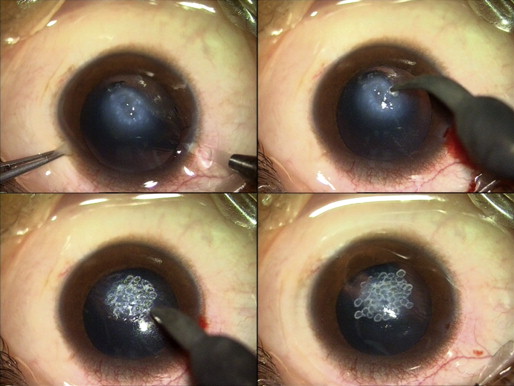
The patients were treated by anterior chamber paracentesis combined with thermokeratoplasty immediately. The surgical procedure was as follows. After peribulbar anesthesia, a puncture was made at the 2 o’clock or 10 o’clock position of the limbus, and 0.2 mL of aqueous humor was drained to lower the IOP and keep the anterior chamber shallow. The edematous cornea was cauterized using a cautery to make the central cornea contract and flatten the prominent cone. The treatment area was slightly larger than the corneal edema. A corneal bandage lens was worn ( Figure 1 ).
Postoperatively, antiglaucoma medication (0.5% timolol maleate eye drops) was used every 12 hours, and low doses of glucocorticoids (0.1% fluorometholone eye drops) were given 4 times a day at first and then tapered off. Slit-lamp microscopy was employed daily, and the IOP was measured weekly. The specific attributes of acute hydrops, such as the size and state of Descemet membrane ruptures and stromal clefts, and changes in corneal thickness were detected in detail by anterior segment OCT weekly.
One week after the complete absorption of the edema and healing of Descemet membrane ruptures, modified DALK was performed. Briefly, four-fifths thickness of the corneal lamellae were cut using a Hessburg-Barron vacuum trephine (7.75 mm in diameter). The incisal edge of the cornea was drawn using toothed forceps, and the lamellae were cut using a knife along the stromal fibers. After the recipient was prepared, a full-thickness corneal graft, 8.0 mm in diameter and with no endothelium, was sutured to the recipient using a “gradual pressure” technique.
Intraoperative Descemet membrane ruptures and recipient opacity were recorded, if any. Transparency of the graft, visual acuity, recipient folds or scarring, and immune rejection were monitored during the follow-up of 6 months to 1 year.
Results
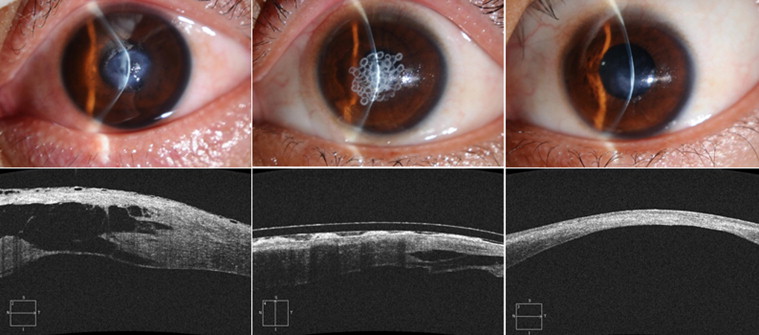
The visual acuity of the 21 patients was counting fingers before the surgical treatment. All patients exhibited anterior corneal protrusion and severe corneal edema, 4–6 mm in diameter, in the central cornea, and the curvature could not be detected. Anterior segment OCT images showed obvious thickening of the central cornea and intrastromal clefts. Descemet membrane ruptures were found in most patients, and detachment of Descemet membrane from the stroma occurred in 6 patients.
After anterior chamber paracentesis combined with thermokeratoplasty, the corneal edema in all patients absorbed significantly, and the intrastromal clefts narrowed and even disappeared at about 5 days. Medication was continued for another week, until the corneal edema almost subsided, and the corneal stroma became thinner, but no obvious scar appeared. At 2 weeks, anterior segment OCT images showed further recovery of Descemet membrane, disappearance of rupture, and a slightly high density of corneal stroma compared with normal ( Figure 2 ).
All 21 patients were successfully treated by DALK about 2 weeks after anterior chamber paracentesis combined with thermokeratoplasty. During the surgery, slight clefts still existed in the central cornea, where Descemet membrane was exposed under the epithelium with only a little stroma, and the matrix fibers disappeared. After the recipient was prepared, the traces of Descemet membrane rupture still could be seen in some patients ( Figure 3 ). A little aqueous humor leaked from the central recipient in 3 patients, but no perforation occurred ( Figure 4 ). No special treatment was performed for the leakage during DALK ( Figure 5 ). On the next day of the surgery, no more aqueous humor leaked between the interface of the recipient and the donor graft. With medication for 1 week, the graft became transparent. One month later, the recipients were completely clear in 7 eyes, without haze or folds. Fourteen patients had slight scars in a shape similar to Descemet membrane ruptures at the center of the recipients.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


