Lamellar Keratoplasty
John D. Goosey
Christopher W. Sturbaum
The history of lamellar keratoplasty covers more than 100 years, beginning with the first successful lamellar corneal transplantation performed by Arthur von Hippel at the end of the 19th century (1). Lamellar keratoplasty represents a more conservative surgical approach than penetrating keratoplasty in that only the diseased portions of a compromised cornea are removed, whereas the healthy structures remain intact. Traditionally, lamellar keratoplasty replaces abnormal anterior corneal tissue from the host with healthy tissue from the anterior portion of a donor cornea while maintaining the integrity of the recipient’s Descemet’s membrane and endothelium. The advantages of such a technique have long been recognized. The most obvious advantage is that sparing the host endothelium eliminates the possibility of endothelial rejection, which is the leading cause of graft failure with penetrating keratoplasty. Other advantages of anterior lamellar keratoplasty result from it being an extraocular procedure, which mitigates complications such as endophthalmitis, expulsive hemorrhage, glaucoma, and cataract formation. In spite of these advantages, most corneal surgeons have eschewed lamellar keratoplasty because of its perceived technical difficulty and the widely held belief that penetrating keratoplasty gives superior visual outcomes. Recent microsurgical techniques and instrumentation have led to increased interest in lamellar keratoplasty. One of the largest factors contributing to this increased interest is the growing popularity of the refractive lamellar procedure, laser-assisted in situ keratomileusis (LASIK). As corneal surgeons have gained more familiarity with microkeratomes and the lamellar aspects of LASIK, the overall interest in lamellar keratoplasty has grown.
Recently, the lamellar surgical philosophy of conservatively sparing healthy host tissue and removing diseased corneal tissue has been applied to the posterior layers of the cornea (2). Posterior lamellar endothelial keratoplasty involves the removal of posterior stroma, Descemet’s membrane, and unhealthy endothelium, followed by replacement with similar healthy donor corneal tissue (3,4). The advantages of posterior lamellar endothelial keratoplasty are derived from maintaining the anterior corneal surface of the recipient, with resultant improved control of postoperative astigmatism. This evolving technique offers the hope of faster visual rehabilitation for those patients with a compromised endothelium than the currently used penetrating keratoplasty techniques. However, the long-term efficacy of deep lamellar endothelial keratoplasty remains to be determined (5).
Lamellar keratoplasty can now be used to replace any specific part of the cornea. The indications, techniques, outcomes, and complications of both anterior lamellar keratoplasty and posterior lamellar keratoplasty are covered in this chapter.
ANTERIOR LAMELLAR KERATOPLASTY
Anterior lamellar keratoplasty is defined as the removal and replacement of deformed or diseased anterior corneal tissue (epithelium, Bowman’s layer, and stroma) while sparing the host Descemet’s membrane and endothelium. The depth of the lamellar dissection is determined by the depth of the anterior corneal pathologic process. Complete removal of stromal tissue to the level of Descemet’s membrane is seldom indicated and carries the risk of penetrating into the anterior chamber. Anterior lamellar keratoplasty can be divided into two major categories: optical and tectonic. Optical lamellar grafts are often large in diameter, and tectonic grafts vary in shape and can be fashioned into specific shapes depending on the indication (Fig. 62-1).
Indications
Anterior lamellar keratoplasty is indicated for the treatment of corneas that have a healthy endothelium but have structural or pathologic changes anterior to Descemet’s membrane. Optical anterior lamellar keratoplasty is very useful for visual rehabilitation of patients with anterior stromal scars after infectious keratitis or trauma. A growing indication for optical lamellar keratoplasty is the treatment of complications after refractive surgery. Visually significant haze after photorefractive keratectomy or scarring of
the anterior cornea following LASIK or radial keratotomy can be successfully managed with optical lamellar keratoplasty (Figs. 62-2 and 62-3). Other optical indications include corneal dystrophies such as Reis-Bückler, Salzmann’s nodular dystrophy, and lattice, granular, or macular dystrophy. Because macular corneal dystrophy can involve both the stroma and endothelium, anterior lamellar keratoplasty should be restricted to those cases of macular corneal dystrophy that have no significant endothelial involvement (Fig. 62-4). Reis-Bückler dystrophy commonly recurs in lamellar grafts, but this problem is safely and easily managed by replacing the graft (6).
the anterior cornea following LASIK or radial keratotomy can be successfully managed with optical lamellar keratoplasty (Figs. 62-2 and 62-3). Other optical indications include corneal dystrophies such as Reis-Bückler, Salzmann’s nodular dystrophy, and lattice, granular, or macular dystrophy. Because macular corneal dystrophy can involve both the stroma and endothelium, anterior lamellar keratoplasty should be restricted to those cases of macular corneal dystrophy that have no significant endothelial involvement (Fig. 62-4). Reis-Bückler dystrophy commonly recurs in lamellar grafts, but this problem is safely and easily managed by replacing the graft (6).
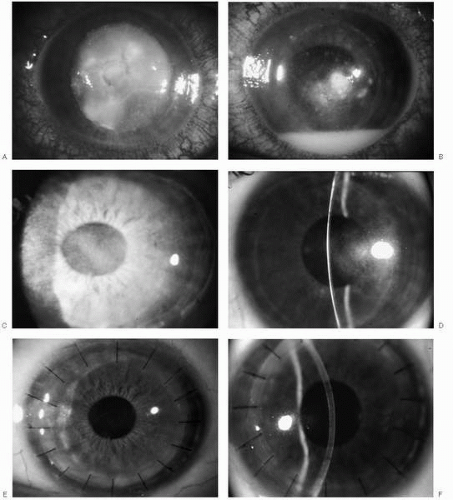
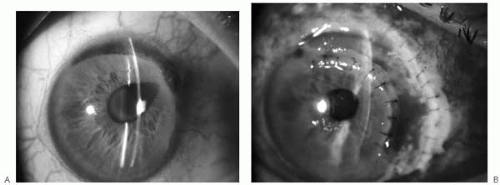 FIGURE 62-1. Tectonic lamellar keratoplasty for the treatment of a perforated Terrien’s marginal degeneration after trauma. A: Peripheral corneal perforation is shown with iris incarceration in the corneal wound and a peaked pupil. B: Corneal integrity is restored by a tectonic horseshoe-shaped lamellar graft. (Courtesy of Jeffrey D. Lanier, M.D., with permission)(see color image) |
Tectonic anterior lamellar keratoplasty is useful for reestablishing the structural integrity of the cornea from peripheral, noninflammatory thinning disorders such as Terrien’s marginal degeneration or pellucid marginal degeneration. Tectonic grafts can also be used to treat peripheral ulcerative keratitis in autoimmune disorders such as Mooren’s ulcer. The inflammatory condition must be resolved to ensure graft survival (7). Structural integrity of a neurotrophic corneal melt from herpes zoster or diabetes can also be managed with a tectonic graft. If the underlying or associated reason for the corneal melt is not recognized and treated, the tectonic graft will fail secondary to stromal melting. In the case of herpes zoster, inferior corneal melting is almost always associated with lagophthalmos, so a tectonic graft combined with a lateral tarsorrhaphy may give the optimal result.
Combined optical and tectonic indications for anterior lamellar keratoplasty include keratoconus, pellucid marginal degeneration and iatrogenic keratoectasia after refractive surgery. LASIK surgery performed on patients with subclinical keratoconus or pellucid marginal degeneration leads to accelerated corneal ectasia with high levels of irregular astigmatism. Such corneas are ideally managed with lamellar keratoplasty because the patient can be visually rehabilitated without future concerns for endothelial graft reactions. The treatment of advanced keratoconus in which the patient is contact lens intolerant is another indication for anterior lamellar keratoplasty (8,9).
Surgical Procedure
A basic understanding of the morphology and biomechanical properties of the corneal stroma is necessary to develop an optimal surgical approach to lamellar keratoplasty. The stroma comprises approximately 90% of the total corneal thickness and is made up of 300 to 500 lamellae (10). Anteriorly, the lamellae are significantly interwoven and often oriented obliquely to the corneal surface. In the posterior two thirds of the stroma, the lamellae are stacked parallel to the corneal surface (11). These features explain why shearing corneal lamellae is much more difficult anteriorly than posteriorly. Collagen interweaving is also more extensive in the corneal periphery than in its center (12). This explains the finding that cohesive strength is greater in the corneal periphery than in the central cornea (13). Cohesive strength is defined as the force required to separate a stromal sample along a cleavage plane parallel to the lamellar axis by pulling in a direction perpendicular to the cleavage plane. Knowing the relative cohesive strength of different areas of the stroma is useful when performing lamellar surgery.
Preparation of the Host Bed
Optical Lamellar Keratoplasty (Malbran’s “Peeling Off” Technique)
The first step in the procedure is to center a trephine over the host corneal tissue to be removed (14,15). Most disorders requiring an optical lamellar keratoplasty can be treated with an 8- to 9-mm diameter trephine. Popular trephines include the Hessburg-Barron vacuum trephine (Jedmed Instrument Co., St. Louis, MO; Katena Products, Denville, NJ), the Hanna trephine (Moria, Antony, France), and the Krumeich trephine system (Rhein Medical, Tampa, FL). The Hessburg-Barron trephine is easy to use and is disposable, but an exact trephination depth can only be approximated. Because the blade of the Hessburg-Barron vacuum trephine spirals downward, the depth of the annular keratotomy created by this trephine is not uniform. One complete revolution of the blade of this trephine incises an annular keratotomy depth of approximately 250 to 300 μm. The desired depth of the trephination is determined by the depth of the corneal lesion, keeping in mind that too deep a trephination could result in entering the anterior chamber and require aborting the procedure. Regardless of the depth of the corneal lesion, a minimum trephination depth of a at least 300 μm is recommended to ensure that the lamellar dissection is started within the posterior stromal lamellae. Lamellar dissection within the anterior stroma is very difficult because of the interlacing nature of these lamellae.
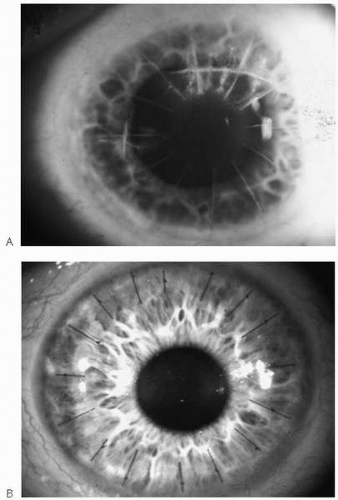
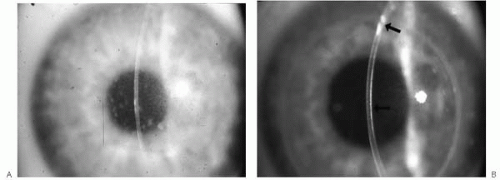 FIGURE 62-4. Macular corneal dystrophy. A: Preoperative photograph showing diffuse stromal opacities consistent with macular dystrophy. B: Clear lamellar graft 3 months after surgery. Top arrow shows the perforation site, which required closure with a 10 nylon suture to complete the procedure. Bottom arrow shows slight interface haze, but patient has 20/25 acuity.(see color image) |
Once the trephination is completed to the desired depth, a 0.12 forceps is used to grasp the inner edge of the annular keratotomy at the 12 o’clock position and, after pulling the inner edge of the trephine cut centrally, the depth is visually inspected. A microsurgical blade (Grieshaber 681.21) is then positioned at the base of the keratotomy incision and lamellar dissection is initiated at the 12 o’clock position by gently cutting the deep lamellae immediately anterior to the base of the trephination. Keeping the microsurgical blade just anterior to the base of the trephination minimizes the risk of inadvertently entering the anterior chamber. The lamellar dissection is then extended for approximately 3 mm centrally from the inner edge of the trephine incision. This 3-mm peripheral dissection should extend along the perimeter of the inner
edge of the keratotomy incision for 270 degrees. Before extending the lamellar keratectomy centrally, the interlacing peripheral corneal lamellae are dissected, thereby reducing the biomechanical forces that resist shearing of the corneal lamellae. This surgical maneuver allows for a much easier and safer dissection of the central posterior lamellae. Some surgeons start the lamellar dissection centrally and omit the initial peripheral dissection. However, if one takes time to perform this peripheral dissection, the central lamellae peel away with mechanical traction applied by pulling the host tissue with a 0.12 or Pollack forceps, obviating the need to cut the central lamellae with the microsurgical blade. Upward traction is applied to the inner edge of the keratectomy at the 12 o’clock position and then the tissue is pulled both upward and axially (centrally). As the posterior lamellae begin to shear, air appears in the fibers at the base of the lamellar keratectomy, making the lamellar fibers appear snowwhite (Fig. 62-5). By keeping the microsurgical blade angled slightly upward, a fine sweeping motion just anterior to the base of the keratectomy is used to tease these white fibers away from the stromal bed and extend the lamellar keratectomy centrally. As the central point of the dissection is reached, the cohesive forces of the posterior lamellae are easily overcome by mechanical traction applied with the 0.12 or the Polack forceps. In Malbran’s original description of this technique, two forceps were used to apply traction with firm and sustained movement, always working from the periphery to the center. The safety advantage of not using a knife over the central cornea is obvious, but an additional advantage of using this peeling method is the natural tendency of the dissection to stay in the same lamellar plane so that a very smooth dissection is obtained. As the dissection passes the central cornea and moves toward the inferior edge of the trephination, some additional peripheral dissection with the microsurgical blade may be required. Once the inferior edge is reached, Vannas scissors can be used to complete the removal of the lamellar keratectomy tissue. Using this dissection approach greatly reduces the risk of inadvertent entry into the anterior chamber when performing lamellar keratoplasty for deep stromal scars or advanced keratoconus. With advanced keratoconus, it is not unusual to bare Descemet’s membrane as one peels the central
stroma away from the host bed. At this point in the dissection, the use of a blade is both unnecessary and unsafe.
edge of the keratotomy incision for 270 degrees. Before extending the lamellar keratectomy centrally, the interlacing peripheral corneal lamellae are dissected, thereby reducing the biomechanical forces that resist shearing of the corneal lamellae. This surgical maneuver allows for a much easier and safer dissection of the central posterior lamellae. Some surgeons start the lamellar dissection centrally and omit the initial peripheral dissection. However, if one takes time to perform this peripheral dissection, the central lamellae peel away with mechanical traction applied by pulling the host tissue with a 0.12 or Pollack forceps, obviating the need to cut the central lamellae with the microsurgical blade. Upward traction is applied to the inner edge of the keratectomy at the 12 o’clock position and then the tissue is pulled both upward and axially (centrally). As the posterior lamellae begin to shear, air appears in the fibers at the base of the lamellar keratectomy, making the lamellar fibers appear snowwhite (Fig. 62-5). By keeping the microsurgical blade angled slightly upward, a fine sweeping motion just anterior to the base of the keratectomy is used to tease these white fibers away from the stromal bed and extend the lamellar keratectomy centrally. As the central point of the dissection is reached, the cohesive forces of the posterior lamellae are easily overcome by mechanical traction applied with the 0.12 or the Polack forceps. In Malbran’s original description of this technique, two forceps were used to apply traction with firm and sustained movement, always working from the periphery to the center. The safety advantage of not using a knife over the central cornea is obvious, but an additional advantage of using this peeling method is the natural tendency of the dissection to stay in the same lamellar plane so that a very smooth dissection is obtained. As the dissection passes the central cornea and moves toward the inferior edge of the trephination, some additional peripheral dissection with the microsurgical blade may be required. Once the inferior edge is reached, Vannas scissors can be used to complete the removal of the lamellar keratectomy tissue. Using this dissection approach greatly reduces the risk of inadvertent entry into the anterior chamber when performing lamellar keratoplasty for deep stromal scars or advanced keratoconus. With advanced keratoconus, it is not unusual to bare Descemet’s membrane as one peels the central
stroma away from the host bed. At this point in the dissection, the use of a blade is both unnecessary and unsafe.
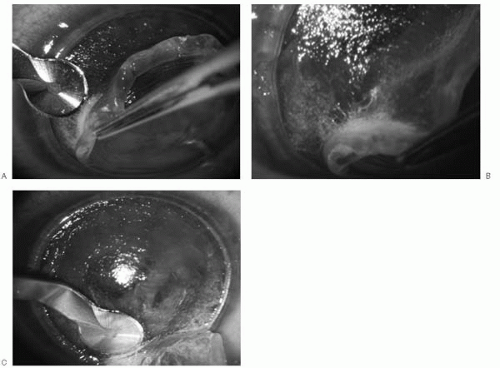 FIGURE 62-5. Intraoperative lamellar keratectomy using Malbran’s technique on a patient with advanced keratoconus. A: Peripheral lamellar dissection keeping blade slightly upward just anterior to white stromal fibers, which form when air enters the dissection plane. B: After peripheral dissection, the central lamellae peel away with mechanical traction without the need to use a microsurgical blade. C: As the peripheral aspect of the inferior edge is reached, the microsurgical blade is used to complete the lamellar keratectomy. Note the glassy, smooth appearance of the central stromal bed, which was safely created without the use of the lamellar blade.(see color image) |
After the lamellar dissection is completed, the recipient bed is inspected. If additional tissue requires removal, a deeper lamellar dissection can be performed by first scratching down on the peripheral edge of the recipient bed with a supersharp knife, and then a second pass at a deeper lamellar plane can be completed. This maneuver is risky and is rarely needed.
In summary, for optimal results, always start each lamellar dissection with a 270-degree peripheral dissection and keep the depth of the dissection at the level of the parallel posterior lamellae. This approach reduces the cohesive forces that naturally resist separation of corneal lamellae and allows for the safe and consistent creation of a smooth lamellar bed.
Air Dissection Technique
Intrastromal air injection can facilitate deep lamellar dissection along a plane in the posterior stroma immediately above or at the level of Descemet’s membrane (16,17). The cornea is trephined to access the deep lamellar tissue. A 30-gauge needle is bent approximately 5 mm from the tip so that the terminal segment angles upward 60 degrees and the bevel faces down. The needle is placed on a 3-mL air syringe. Then the needle is introduced bevel down into the base of the keratotomy incision and advanced obliquely 3 to 4 mm from the keratotomy edge in a plane parallel and just anterior to Descemet’s membrane. The needle is advanced bevel down to avoid penetrating Descemet’s membrane, and obliquely to avoid the thinner central part of the cornea. Approximately 1 mL of air is injected into the posterior stroma to create a plane of tissue separation. If the cannula is accurately placed just above Descemet’s membrane, a large bubble will fill the space between the posterior stroma and Descemet’s membrane. A successful dissection results in a white, semiopaque disk with a near-circular outline. An unsuccessful attempt yields a fuzzy region of white, opaque cornea. If the first attempt fails, the needle is withdrawn and the procedure may be repeated at another point on the perimeter of the trephine groove. The needle tip should be visible and bevel down at all times to avoid perforation. Because each attempt leaves part of the cornea opaque, only three or four tries are possible. Accurate needle placement is enhanced by using intraoperative ultrasonic pachymetry and a microcalibrated trephine to create an annular keratotomy at the pre-Descemet’s level (Hanna or Krumeich trephine).
After creating a large bubble separation of Descemet’s membrane from posterior stroma, a paracentesis is made at a site peripheral to the edge of the large air bubble, but no aqueous is drained at this time. A partial-thickness anterior keratectomy is manually performed, leaving a layer of posterior stroma in place anterior to the bubble. Then aqueous is drained through the paracentesis. A sharptipped blade held nearly parallel to the corneal surface is used to penetrate the remaining stromal layers near the center of the cornea. The knife should be held in one plane because if it is tilted after entering the bubble, air may escape prematurely. The opening is made large enough to insert a wire spatula (Anwar spatula; Katena Products). The spatula is advanced in the cleavage plane that was created by the air until its tip reaches the trephination groove. The spatula is lifted anteriorly to tent slightly the residual stromal layers. The layers are then dissected by cutting down on the spatula with a supersharp knife. This maneuver is repeated in other directions either at a 180-degree angle or in any other radial direction to enlarge Descemet’s membrane exposure. Then the deepest stromal layers are circularly excised with a blunt-tipped microscissors to leave a bare Descemet’s membrane recipient bed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree