Asthma is a dynamic and complex inflammatory disease. Recent research suggests that it is a manifestation of a systemic disorder of the entire respiratory system including both upper and lower airways. The diagnosis of asthma can be made based on clinical history, physical findings, and pulmonary function tests such as spirometry. In children, spirometry may be difficult; therefore, diurnal changes in peak expiratory flow rate can be used instead to assist in the diagnosis of asthma. Increasing the use of objective pulmonary measures will help better identify and monitor treatment of lower respiratory inflammatory disease.
Asthma is a chronic inflammatory disease of the lower airway that, despite considerable advances in understanding and treatment, continues to have a significant impact. Recent studies have shown a relationship between asthma and allergic rhinitis and rhinosinusitis in what has been called “unified airway disease” (also referred to as the “integrated airway hypothesis,” “chronic respiratory inflammation syndrome,” or “rhinosinobronchitis”) because of common characteristics in pathophysiology and anatomy . Both asthma and rhinosinusitis involve an inflammatory process with similar cellular influx, cytokine release, and changes in basement membrane thickening. Both also have similar histology in ciliated, pseudostratified columnar respiratory epithelium . Asthma is a dynamic inflammatory process with complex interactions of age, time, seasons, environmental factors, and multiple comorbidities. As such the diagnosis and treatment can be challenging, but using objective measures such as pulmonary function tests (PFT) can help in diagnosis, predict severity, and monitor both disease progression and therapeutic response.
The diagnosis of asthma is made by history and physical examination. Symptoms include cough, shortness of breath, chest tightness, and decreased exercise tolerance. Physical findings include wheezing, chest hyperinflation, and associated signs of atopy. Laboratory studies are nondiagnostic and are not used routinely but when examined can reveal increased blood and sputum eosinophilia and increased total serum IgE. Other adjuvant tests include allergy skin testing to identify inciting factors and imaging studies to rule out other airway diseases and exclude contributory diseases such as sinusitis.
Pulmonary function testing
PFTs can be used to obtain objective data, but their use should be considered complementary to history and physical examination. A thorough understanding of respiratory pathophysiology is necessary to understand expected changes in the PFT. Asthma involves reversible, hyperresponsive airway inflammation with intermittent airway obstruction. Bronchoconstriction, edema, mucous plugs, or airway remodeling can cause changes in asthma airway physiology.
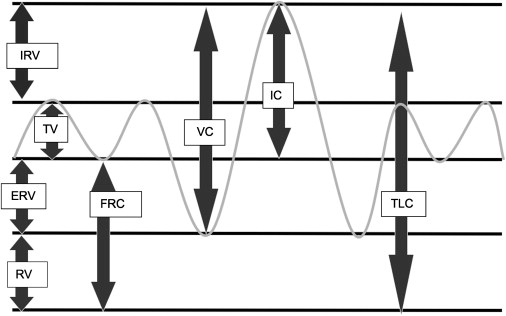
There are several methods to evaluate various aspects of pulmonary function. The different components of the PFT include (1) assessment of lung volumes, (2) spirometry, (3) flow-volume loops, (4) diffusion capacity, and (5) body plethysmography. The different subdivisions of lung volumes and capacities (sum of various lung volumes) are depicted in Fig. 1 .
Lung volumes
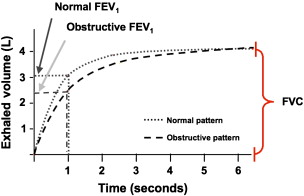
The tidal volume is the volume of air inspired or expired with each normal breath. Inspiratory reserve volume is the volume that can be inspired over and above the tidal volume. Expiratory reserve volume is the volume that can be expired after the expiration of a tidal volume. The residual volume is the volume that remains in the lungs after a maximal expiration and cannot be measured by spirometry. Functional residual capacity is the sum of the expiratory reserve volume and the residual volume and is the volume that remains in the lung after a tidal volume is expired. Vital capacity or forced vital capacity (FVC) is the sum of the tidal volume, the inspiratory reserve volume, and the expiratory reserve volume and is the volume of air that can be expired forcibly after a maximal inspiration. Total lung capacity is the volume of gas in the lungs at maximal inspiration and the sum of all four lung volumes . Forced expiratory volume (FEV 1 ) is the volume of air that can be expired in the first second of a forced maximal expiration ( Fig. 2 ).

Lung volume measurements are dependent on functional residual capacity, which can be measured by three different methods: nitrogen washout, helium dilution, and body plethysmography. The nitrogen washout and helium dilution methods both use physiologically inert gases that are poorly soluble in alveolar blood and lung tissues to calculate volumes. In the nitrogen washout method all exhaled gas is collected while the patient inhales pure oxygen. The volume of nitrogen-containing gas present at the beginning of the maneuver can be calculated from the assumed initial concentrations of nitrogen and the total amount of nitrogen washed out from the lungs, . The helium dilution method is similar in concept, but the patient rebreathes a gas mixture containing helium until equilibration is achieved. The volume and concentration of helium are known, and thus final measurements of the equilibrium concentration allow calculation of the volume of gas in the lungs at the start of the maneuver . Both methods are sensitive to leaks in the system and cannot measure areas of poor air movement (ie, lung bullae).
Body plethysmography
There are three methods of body plethysmography: pressure, volume, and pressure-volume. The pressure method uses a closed chamber with a fixed volume in which a patient breathes and is best suited for small volume changes. Volume changes in the thorax are measured as pressure changes in the gas within the box . The volume method is an open-type method with a constant pressure and variable volume. When thoracic volume changes, the gas is displaced through a hole in the box and is measured, making this method suitable for both small and large volume measurements. Both systems use Boyle’s law, V 1 P 1 = V 2 P 2 , to calculate volume or pressure. The pressure-volume method uses a device that combines the two previously mentioned systems. As a patient breathes and thoracic gas volumes change, both the air surrounding the patient in the box that is displaced through a hole in the box and the pressure changes are measured.
Spirometry
Spirometry and flow-volume loops are used to evaluate FVC and FEV 1 . Spirometry records the volume of air inhaled and exhaled plotted against time during various ventilatory maneuvers . The graphs obtained from these studies can indicate normal patterns or abnormal patterns characteristic of obstructive, restrictive, or mixed lung disease. None of these patterns are specific, and spirometry alone cannot establish a diagnosis, but most disorders have predictable ventilatory defects; spirometry is reliably reproducible and can be used to assess and monitor disease and gauge response to treatment. These tests can be performed with simple, inexpensive recording spirometers. Data are compared with normal values established for reference patients of matched age, gender, size, and ethnicity . FEV 1 is the dynamic volume most often used with FVC in analysis of spirometry . Normal FEV 1 is 80% of the FVC, and the FEV 1 /FVC ratio is also used. Asthma is an obstructive lung disease in which expiration is impaired and is characterized by normal to decreased FVC, decreased FEV 1 and FEV 1 /FVC ratio , and increased residual volume caused by air trapping. Restrictive lung disease involves decreased lung compliance in which inspiration is impaired, with decreases in all lung volumes and a normal or increased FEV 1 /FVC ratio ( Figs. 3 and 4 ) .

Another measurement to evaluate airway obstruction is the mean forced expiratory flow during the middle of FVC (FEF 25%–75% ), which measures the mean rate of airflow between the two defined points ( Fig. 5 ). FEF 25%–75% targets the measurement of small airways during expiration and often can be more sensitive, although less specific, than FEV 1 . A value greater than 65% is considered normal for FEF 25%–75% .

Measured values from spirometry also can be used for evaluating the severity of obstruction and monitoring treatment response. FEV 1 is used to assess lower airway obstruction. A predicted value of FEV 1 between 70% and 85% is considered mild, a value between 60% and 69% is moderate, between 50% to 59% is moderate severe, between 35% and 49% is severe, and less than 35% is very severe obstruction . Lower respiratory airway obstruction in asthma is reversible and improves with administration of a short-acting bronchodilator; this improvement is termed “bronchodilator responsiveness.” An increase by 12% for the FEV 1 after a bronchodilator treatment supports a diagnosis of asthmatic disease.
Another method to support the diagnosis of asthma using lung volumes is pulmonary challenge, also known as “bronchial provocation.” Asthmatic obstruction of the reactive lower airway is triggered by various stimuli and can be provoked with agents such as methacholine, adenosine monophosphate, or histamine. The amount of stimulus needed to decrease the FEV 1 by 20% from the baseline is termed the “PC 20 ” . The PC 20 is lower in asthmatic patients than in the normal population ( Fig. 6 ). A value between 0.03 and 0.124 is classified as severe, between 0.125 and 1.99 is moderate, between 2.00 and 7.99 is mild, and between 8.0 and 25 is increased hyperresponsive reaction. The PC 20 does not diagnosis asthma definitively, because changes also can be seen in viral diseases, but it can contribute objective data to support the diagnosis of asthma (see Fig. 6 ).





