Purpose
To describe 6 patients representing a new entity of Meibomian gland keratinous cysts.
Design
Retrospective, interventional, clinicopathologic study.
Methods
Review of clinical histories and findings, histopathologic evaluations, and immunohistochemical studies of the cysts’ linings with monoclonal antibodies directed against cytokeratins and cell surface epithelial markers.
Results
Six patients with an average age of 62.5 years had noninflamed, upper eyelid nodules fixed to the tarsus. Eyelid eversion revealed a white–yellow nodular bulge in 3 cases, a bluish coloration in 2 cases, and a translucent appearance in 1 case. The cysts were lined by undulating squamous epithelium possessing an inner eosinophilic cuticle that produced a peculiar refractile, strand-like intracavitary keratin. Immunostaining for cytokeratin 17 and carcinoembryonic antigen showed strongly positive results in the Meibomian gland cysts and, by comparison, negative results in cutaneous epidermal cysts. Multiple recurrences occurred after incomplete excisions.
Conclusions
After chalazia and sebaceous cell tumors, Meibomian gland keratinous cysts seem to be the third most common primary intratarsal lesion. Anterior fixation to the tarsus and posterior protrusion beneath the palpebral conjunctiva without inflammation suggest the diagnosis. Histopathologic and immunohistochemical evaluations can distinguish unequivocally the current entity from common epidermal cysts. The optimal treatment consists of an en bloc excision of the cyst with a tarsectomy, or else wide excision with intratarsal cautery of any remnants of the cellular lining.
Chalazia and sebaceous cell (Meibomian) carcinomas are the mass lesions of the tarsus that have received the most clinical attention. Other intratarsal tumors occasionally have been documented to occur, but only as curiosities. Recently, intratarsal epidermal inclusion cysts encountered in older individuals have been described. This valid new entity is probably the third major cause of primary tarsal swellings. For reasons that will be given later in this article, we have concluded that the diagnostic term that was initially selected for it is a double misnomer.
We report a series of 6 cases highlighting new clinical observations and amplifying certain histopathologic and immunohistochemical features that are virtually pathognomonic. The major reason to diagnose these novel lesions accurately as intratarsal keratinous cysts of the Meibomian gland and to distinguish them from relatively innocent epidermal (inclusion) cysts of the eyelid is that they can exhibit multiple recurrences, and therefore require a more aggressive surgical approach in their management.
Methods
After we observed an unusual squamous cell-lined cyst of the eyelid, we reviewed the diagnostic files of the Cogan Ophthalmic Pathology Laboratory since 2006 to identify similar cases that might have been designated as epidermal cysts, epidermoid cysts, epidermal inclusion cysts, or pilar (trichilemmal) cysts. Five additional cases were found that shared the unusual histopathologic features of the index case. These characteristics could be used to distinguish them from garden variety epidermal cysts commonly occurring within the dermis of the eyelid skin. Clinical histories, clinical photographs of the lesions obtained externally and on eversion of the eyelids, and intraoperative findings were reviewed. Routine hematoxylin and eosin staining of paraffin-embedded sections, and Alcian blue, mucicarmine, Brown-Hopps, Prussian blue, and Von Kossa histochemical staining were performed.
Immunohistochemical investigations were performed on: 5 specimens of either normal glands (n = 3; displaying undisturbed secretory acini and short lateral ductular passages that led to the large vertical draining excretory ducts) or glands with ectatic ducts and atrophic acini (n = 2; secondary to obstruction by a basal cell carcinoma or chalazion); 3 specimens of the current Meibomian gland cysts; 4 specimens containing normal epidermis; and 5 specimens of common epidermal cysts situated in the dermis that exhibited a keratohyalin granular cell layer in the lining. Ki-67 nuclear immunostaining for cells in S-phase was performed on 6 Meibomian gland cysts, 3 specimens with epidermis, 2 epidermal cysts, and 1 specimen containing sebaceous secretory acini.
The antibodies used and their sources were the following: anticytokeratin 5/6 mouse monoclonal antibody, 1:50 dilution (DAKO Corp, Carpenteria, California, USA); anticytokeratin 7 mouse monoclonal antibody, prediluted (Ventana Medical Systems, Tucson, Arizona, USA); anticytokeratin 14 mouse monoclonal antibody, prediluted (Ventana Medical Systems); anticytokeratin 17 mouse monoclonal antibody, 1:50 dilution (DAKO Corp); CAM 5.2, 1:80 dilution (Becton Dickinson, Franklin, Lakes, New Jersey, USA); cytokeratin AE1/AE3 mouse monoclonal antibody, 1:160 dilution (Signet Laboratories, Dedham, Massachusetts, USA); anti-epithelial membrane antigen (EMA) mouse monoclonal antibody, prediluted (Signet Laboratories); anti–carcinoembryonic antigen (CEA) mouse monoclonal antibody, prediluted (Ventana Medical Systems); and Ki-67 rabbit monoclonal antibody, prediluted (Ventana Medical Systems).
The staining was carried out on BenchMark XT automated tissue staining systems (Ventana Medical Systems) using validated protocols. Endogenous peroxidase activity was blocked by H 2 O 2 before antibody incubation. A combination of ethylenediaminetetraacetic acid and boric acid in Tris buffer (CC1 reagent; Ventana Medical Systems) was applied to the tissue sections for antigen retrieval as needed, and the process was carried out before primary antibody incubations. The tissue sections were washed and incubated with primary antibodies indicated above, followed by incubation with UltraView HRP-conjugated multimer antibody reagent (Ventana Medical Systems). Antigen detection was performed using Ultraview and diaminobenzidine as the chromogen (Ventana Medical Systems). Tissues were counterstained with hematoxylin.
Results
Clinical Findings
Table 1 summarizes the salient demographic characteristics and the preoperative and intraoperative findings of 6 patients with solitary lesions. All developed in the upper eyelids of adults with a median age of 68 years and an average of 62.5 years. The patients became aware of a lump in the eyelid and were symptomatic from 10 weeks to 3 years before the first excision. Three lesions were diagnosed as chalazia even after several recurrences; 1 lesion originally was suspected of being a melanoma, and 2 lesions were diagnosed correctly clinically from the outset. At the time of the last excision of their lesions, 2 patients were known to have an epithelial cystic lesion based on the results of an antecedent pathologic evaluation. One patient had 3 recurrences ranging from 9 months to 5 years after the first surgery, whereas a second had 4 recurrences at intervals between 5 months to 2 years. Only 1 patient had a decline of visual acuity to 20/80 with additional reports of pain and photophobia. The latter resulted from a tarsal surface irregularity that caused a superior marginal erosive keratitis. Otherwise, the patients described no discomfort or other ocular symptoms.
| Patient No. | Age (years) | Gender | Duration of Symptoms before First Presentation | Location and Size of First Lesion or Last Recurrence | Reported Symptoms | Visual Acuity | External Examination | Findings on Eyelid Eversion | Preoperative Diagnosis | Surgical Approaches | Intraoperative Findings | Recurrence(s) and Intervals between Surgeries | Follow-up since Last Surgery (mos) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 76 | M | 2 yrs | LUL; 6 × 9 mm | Slowly enlarging lump | Right eye, 20/30; left eye, 20/50 | Uninflamed and immobile subcutaneous cyst | Yellow-white, round cystic lesion | Tarsal cyst | Anterior cutaneous with full-thickness partial tarsectomy | Cyst rupture; whitish keratinlike material extruded from excised tarsus | None | 4 |
| 2 | 49 | F | 9 mos | LUL; 7 mm in diameter | Lump | Right eye, 20/15; left eye, 20/20 −1 | Uninflamed lump with mobile overlying skin | Uninflamed opalescent tense lesion | Chalazion during early recurrences; epithelial inclusion cyst at third recurrence | Early I&C; final anterior cutaneous, through lid crease, with tarsectomy | Rupture of cyst with extrusion of white keratinous contents; small opening remained in the tarsus | 3 recurrences: 5 yrs, 7 mos, 9 mos | 6 |
| 3 | 31 | M | 2 to 3 yrs | RUL; 8 mm in diameter | Painless lump | Right eye, 20/25 +2 ; left eye, 20/20 | Uninflamed round mass with mobile overlying skin | Uninflamed white lesion protruding through tarsus | Tarsal cyst | Anterior cutaneous, through lid crease, with tarsectomy | Cyst emanated from tarsus with protrusion posteriorly; rupture of cyst with extrusion of whitish contents; intratarsal cavity cauterized | None | 5 |
| 4 | 63 | F | 3 mos | LUL; 5 × 7 mm | Painless, nonprogressive lump | Both eyes, 20/20 | Uninflamed lump | Bluish nodule | Chalazion | Posterior conjunctival, with tarsectomy | Cyst rupture during excision; grey/bluish, gelatinous contents extruded | None | 12 |
| 5 | 73 | M | 10 wks | LUL; 3 × 5 mm on palpebral conjunctival surface | Ocular pain with photophobia | Right eye, 20/80; left eye, 20/25 | Uninflamed; no visible lesion; marginal keratitis | Uninflamed blue/grey tarsal lesion with linear pigment extending vertically to notched lid margin | Intratarsal melanoma | Full-thickness eyelid resection | Cyst removed in toto, embedded in tarsus | None | 20 |
| 6 | 67 | M | 2 mos | LUL; 8 × 9 mm | Lump with mild surrounding swelling | Right eye, 20/30; left eye, 20/40 | Uninflamed lump with edema | Uninflamed rounded white mass | Chalazion during early recurrences; intratarsal cyst at fourth recurrence | I&C of presumed chalazia during early treatments; partial wall excision during last I&C; final surgery through lid crease with tarsectomy | Discolored material seen during third I&C; keratinous material during 4th I&C; thick-walled tarsal cyst finally completely excised, causing rupture and extrusion of keratinous material | 4 recurrences: 5 mos, 2 mos, 5 mos, 2 yrs | 14 |
In 5 patients, careful external examination revealed a clearly visible noninflamed lump on the cutaneous aspect of the upper eyelid that felt firm and nonfluctuant and also was nonpainful ( Figure 1 , Top left and Top middle). In 1 patient ( Table 1 ; Patient 5), an externally discernible skin lesion was not present. The lesions measured from 3 to 9 mm in diameter. The overlying skin was of normal color, evidenced a healed scar where there had been earlier surgery ( Figure 1 , Top middle), and sometimes exhibited tenseness or tautness over the nodule. The externally palpable lesions were fixed to the tarsus; the overlying skin freely moved over the nodule. On eversion of the eyelids, the palpebral conjunctival surface was involved in all 6 cases (including the one without an obvious cutaneous lesion) and revealed signs of a subsurface intratarsal lesion. Three of these were clearly defined, upraised white or pale yellow bulges ( Figure 1 , Top right and Bottom left); 2 were gray to blue ( Figure 1 , Bottom middle), 1 of which had a vertical linear bluish extension that reached the eyelid margin to create a small notch; and the last appeared as a translucent area of the palpebral conjunctiva. None of the lesions was subjected to transillumination, nor was ultrasonography performed.
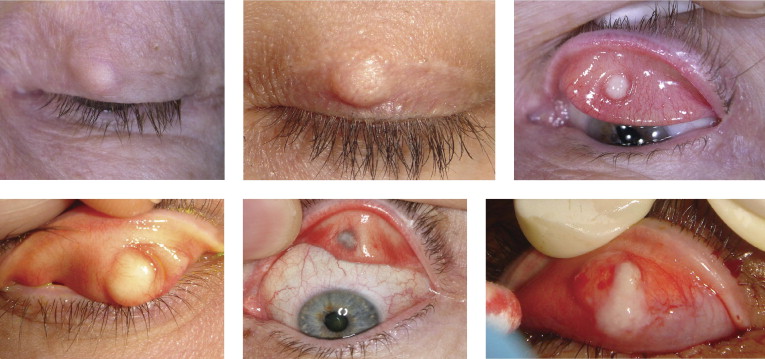
Four surgical approaches initially were adopted. In 1 case (Patient 5), a full-thickness pentagonal central eyelid resection initially was performed that included the totality of the unruptured cyst. In 2 cases, there were sequential incisions and curettages until an anterior cutaneous incision through the eyelid crease led to complete removal. In 2 other cases, the first approach was an eyelid crease incision that included a partial tarsectomy; in only 1 patient was a transconjunctival partial tarsal excision attempted. During dissections, the cysts had a thick and well-developed wall or capsule that was always fused focally to the tarsus as an intrinsic part of it. During these dissections, the walls of all 5 of the locally excised cysts ruptured. Milky fluid ( Figure 1 , Bottom right), rather than semisolid, pasty, or cheesy material characteristic of a chalazion or a conventional epidermal cyst, was released in 4 of these 5 cases; dark bluish viscid material was extruded in the fifth. In each case, a full-thickness hole in the tarsus was left after a wide local excision was performed that included normal surrounding tarsus in the tarsectomy. Cautery was used in 3 cases to extirpate any potential remnants of the cysts’ epithelial lining after a correct histopathologic diagnosis ruling out a chalazion had been established.
The patient with the full-thickness eyelid resection has not experienced a recurrence during 20 months of follow-up. Two patients with one local excision have had follow-ups of 5 and 12 months without recurrence. The other 2 patients with multiple recurrences have been disease free for 6 months and 14 months since the last surgery, which finally included a partial tarsectomy and cautery. One patient who had an initial partial tarsectomy has been followed up for a disease-free period of 4 months.
Histopathologic Findings
The specimen obtained from the full-thickness eyelid resection ( Table 1 ; Patient 5) contained 2 cysts, a larger one at mid-height in the tarsus and a smaller one nearer the eyelid margin ( Figure 2 , Top left). The cysts were positioned approximately in the center of the tarsus, with somewhat more collagen separating the posterior edge from the palpebral conjunctiva than from the anterior orbicularis muscle. The tarsus was blandly scarred without inflammation and was devoid of sebaceous lobules and ducts above the cysts. A few surviving elements of the acinar elements of the Meibomian glands were observed near the eyelid margin. The cysts were filled with compact keratin and were lined by a smooth, curvilinear, multilaminar squamous epithelium that was devoid of keratohyalin granules and a distinct cuticle ( Figure 2 , Top right). No hair structures were observed within the keratin. Hematoxylinophilic granular material was found between the keratinous lamellae ( Figure 2 , Top right) within the central cavity. The Brown-Hopps stain ( Figure 2 , Top right, outer inset) disclosed clusters of positive, blue-staining cocci without any associated inflammation; the von Kossa stain ( Figure 2 , Top right, inner inset) revealed the black staining of calcium; and the Prussian blue stain for iron demonstrated negative results.
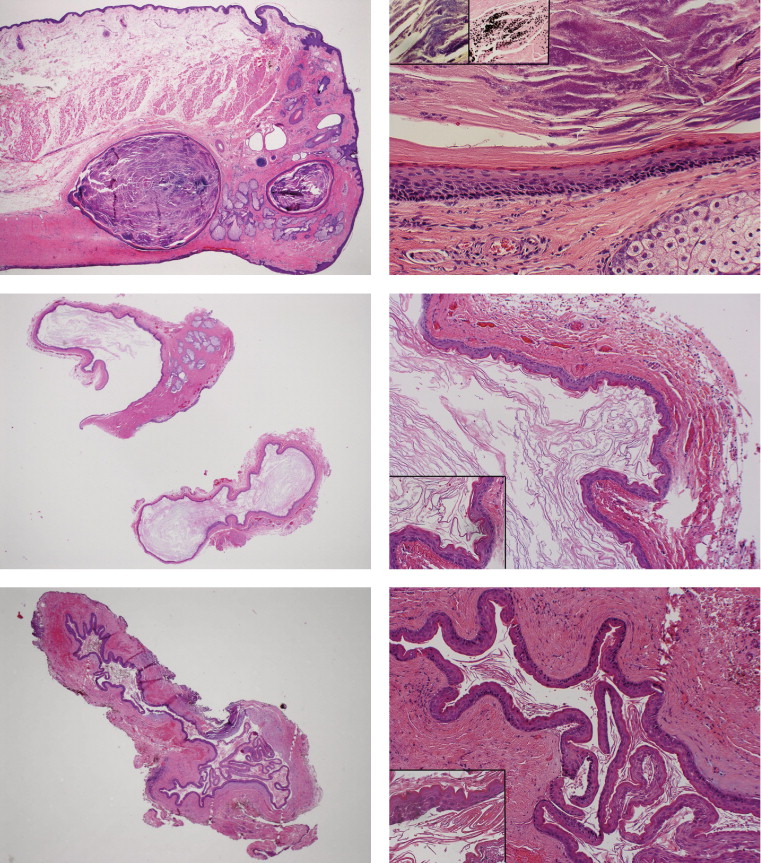
The other 5 specimens of the locally excised lesions showed remarkably similar histopathologic findings. If the cyst protruded anteriorly into the eyelid skin, it was still clearly attached to a portion of excised tarsus ( Figure 2 , Middle left). The 5 locally excised cysts exhibited poorly vascularized, thick collagenous walls ( Figure 2 , Middle right, Bottom left and right). No focal collections of mononuclear inflammatory cells or hemosiderin-laden macrophages were observed in the pericystic dense connective tissue. The epithelial linings were composed of squamous cells without keratohyalin granules or intermixed goblet or sebaceous cells ( Figure 2 , Middle right and Bottom right). The innermost cells were thrown into undulations or corrugations (crenulations) with an intensely eosinophilic cuticular layer bordering the lumen. The cuticle diffusely desquamated into the lumen as needle-like or string-like refractile, loose, anuclear, keratinous structures ( Figure 2 , Middle right, inset and Bottom right, inset), rather than resembling the more loosely woven keratin typical of epidermal cysts. Atrophic Meibomian sebaceous glands were found in the vicinity of the cysts in 2 specimens. One specimen of a subtotally removed cyst that was obtained via a transconjunctival approach caused some initial interpretive confusion. The conjunctival surface was covered by shaggy, nonkeratinizing epithelium that eventually was demonstrated to possess goblet cells by means of Alcian blue staining. It was distinguished readily from a nearby portion of the cyst’s lining, which exhibited larger cohesive eosinophilic squamous cells with undulations, an inner cuticular layer, and the absence of goblet cells.
Immunohistochemical Findings
Table 2 summarizes the results of the immunohistochemical studies. The immunolabeled antigens that most sharply distinguished the intratarsal Meibomian gland keratinous cysts from the cutaneous epidermal cysts were cytokeratin (CK) 17 ( Figure 3 , Top left and right), CEA, and EMA. This staining profile paralleled that of the normal ducts (short lateral ductules and main vertical excretory ducts) and the obstructed and secondarily ectatic Meibomian ducts. CK-5/6 and CK-17 stained only the outer basal cells of the normal Meibomian acini. With respect to the Meibomian gland cysts, CK-5/6 ( Figure 3 , Middle left) stained the basal and suprabasal region along with the cuticle and luminal keratin strands, whereas CK-14 ( Figure 3 , Middle right) stained most layers, but not the cuticle or keratin. CEA strongly stained the cuticle, and EMA did so to a lesser degree ( Figure 3 , Bottom left). The staining characteristics of the intracavitary keratin contents revealed by the various probes were not helpful in differential diagnosis. The epidermal cysts were best distinguished by negative immunostaining for CK-17, CEA, and EMA ( Figure 3 , Bottom right). AE1/AE3 consistently was positive only in the duct cysts and unreliably in the epidermal cysts; CK-7 was of no value in differentiating the 2 types of cysts.
| Anatomic Structures/Lesions | CK-5/6 | CK-7 | CK-14 | CK-17 | Cam 5.2 | AE1, AE3 | EMA | CEA |
|---|---|---|---|---|---|---|---|---|
| Normal meibomian acini (lobules) | + (basilar) | − | ++ | −/+ (basilar) | − | − | ++ | − |
| Normal meibomian ducts (vertical and short lateral) | + | − | ++ | −/+ | − | −/+ | −/+ | − |
| Meibomian gland cysts | ||||||||
| Lining | ++ | − | ++ | ++ | − | + | + | ++ |
| Cuticle | + | − | − | + | − | + | + | ++ |
| Keratin contents | ++ | +/− | − | + | − | + | −/+ | ++ |
| Normal epidermis | + | − | + | − | − | − | − | − |
| Cutaneous epidermal cysts | ||||||||
| Lining | + | − | ++ | − | − | −/+ | − | − |
| Cornified layer | − | − | − | − | − | − | − | − |
| Keratin contents | −/+ | − | − | − | − | − | − | − |
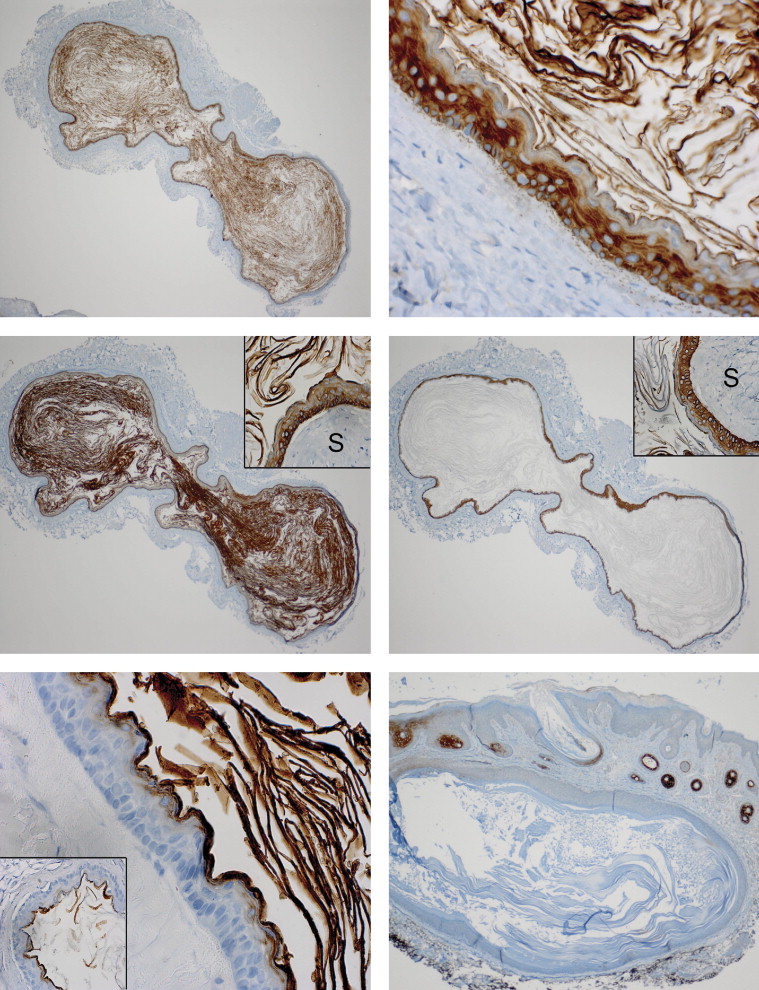
The different cytokeratins were located preferentially in varying cellular layers: 1) basal and suprabasal, 2) parabasal or mid-level, 3) apical or adlumenal, and 4) cuticular. For the Meibomian cysts, CK-5/6 was identified in the basal and suprabasal layers, and CK-14 and CK-17 were detected in the basal, suprabasal, and parabasal layers. CK-14 stained the cytoplasm more intensely than CK-5/6 and CK-17. Whereas CEA and EMA both stained the cuticular and adlumenal layers of the cysts, CEA also stained the keratin within the duct cysts but EMA did not. For the cutaneous epidermal cysts, CK-17 was totally negative in all layers, CK-5/6 was observed in the basal and suprabasal layer, and CK-14 was observed in the basal, suprabasal, and parabasal layers.
Positive Ki-67 absolute counts (average of immunolabeled nuclei in 3 high-power ×400 microscopic fields) were: 18 for 2 separate examples of secondarily ectatic Meibomian ducts; 24 for the 6 Meibomian cysts; 22 for the germinal layer of normal epidermis in 3 specimens; and 14 for 2 epidermal cysts. In 1 specimen ( Table 1 ; Patient 5) with a preserved Meibomian gland secretory lobular architecture, the average Ki-67–positive cell count was 40.3 and was restricted to the outer compressed rim of basal germinal cells.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


