Intraoperative Monitoring of the Facial Nerve and Hearing
Robert A. Levine
Steven F. Ronner
Aaron R. Thornton
The authors thank B. Kiang for preparing many of the figures and M. Skrip and J. Wilkins for their valuable assistance with the middle ear and mastoid section.
The ideal in any medical intervention is to achieve its purpose with no or minimal adverse effects. For temporal bone surgery, that includes no postoperative cranial nerve deficits. Facial nerve monitoring can minimize the likelihood of injuring the facial nerve intraoperatively for two reasons. First, the nerve can be localized by electrical stimulation when its location may not be visually apparent. Second, electrophysiologic monitoring can detect facial nerve irritation in the absence of any overt facial movement (1, 2, 3, 4, 5, 6). Immediate postoperative facial function can also be predicted by stimulation of the most proximal segment of the facial nerve (7, 8, 9, 10). However, at present delayed facial weakness cannot be predicted.
For historical reasons, each of the authors’ two hospitals has independently developed its own facial nerve monitoring program. Middle ear and mastoid surgery is done at the Massachusetts Eye and Ear Infirmary and suboccipital cerebellopontine angle surgery at Massachusetts General Hospital. As will be apparent from this presentation, the methods are very similar, but by the nature of the different surgical techniques some differences in monitoring have evolved. For example, because rigid head fixation is used in suboccipital cerebellopontine angle surgery, facial movements can be monitored with a motion sensor, but such monitoring is impractical for middle ear surgery because the unrestrained head is relatively free to move.
MIDDLE EAR AND MASTOID SURGERY: FACIAL NERVE MONITORING
Instrumentation and Technique
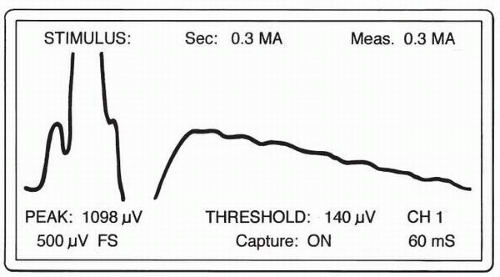
The facial nerve passes through the internal auditory meatus of the temporal bone and traverses the mastoid through the fallopian canal, passing near several surgical landmarks in the middle ear, including the facial ridge, hypotympanum, and oval window. Although normally protected by bone, the nerve can be exposed due to atypical anatomy, erosion of the bone by disease, or removal of bone from prior surgery. Facial nerve irritation is detected by increased electrical activity of muscles innervated by the facial nerve (passive monitoring), and the facial nerve is located by detecting facial muscle contractions from direct electrical stimulation of the nerve from various points in the operative field (active monitoring). This electrical stimulation uses 4-per-second, 0.2-msec duration pulses, whose amplitude usually ranges between 0.1 to 0.6 mA. As with any nerve conduction study, a compound muscle action potential (CMAP) is produced (with about a 3-msec latency), and it can be readily detected with an oscilloscope triggered by the stimulus pulse (Fig. 7.1).
Aside from the stapedial nerve, the motor portion of the facial nerve has no other branches before it emerges at the stylomastoid foramen. Consequently, stimulation of the nerve trunk within the mastoid or middle ear may excite any or all of the muscles of the head and neck that are innervated by the facial nerve. Stimulation during surgery, intentional or inadvertent, can be expected to activate muscles over a large portion of the face. Differential recording electrodes placed at the outer canthus of the eye and near the nares and upper lip are sensitive to myogenic activity from all muscle groups in the central portion of the face. The myoelectric signals are relatively strong in this region, providing good sensitivity and signal-to-noise ratio of the recordings. The differential ground is typically placed on the cheek. Surface and needle electrodes perform equally well for this type of broadly spaced, nonspecific array. The monitoring device presently being used by us for mastoid and middle ear surgery, the Xomed Neural Integrity Monitor (NIM), can record two channels simultaneously, typically with one pair of electrodes near the eye and the other near the upper lip. However, this somewhat increased specificity for site of activity provides no greater sensitivity for active or passive
monitoring; furthermore, two channels have the disadvantage of dividing the monitor’s attention and thereby increasing the likelihood of missing a fleeting event. For these reasons, we routinely monitor with a single channel.
monitoring; furthermore, two channels have the disadvantage of dividing the monitor’s attention and thereby increasing the likelihood of missing a fleeting event. For these reasons, we routinely monitor with a single channel.
Surface electrodes are easily applied with the patient just prior to anesthesia. The recording instrument can be then be used to evaluate the amplitude of the EMG (electromyography), which is particularly helpful for patients with a preexisting facial paresis. If necessary, electrodes can be placed satisfactorily even after the start of surgery. Instruments such as the NIM display the ongoing EMG on a small screen and can provide alarms when the waveform exceeds specified criteria. However, electrical artifacts generated by instruments, irrigation, drilling, and manipulation of the patient are mixed with the EMG and are often large enough to set off the alarms, causing unnecessary confusion and irritation. Consequently, the alarms are generally silenced when (i) there is no risk to the nerve or (ii) a monitor operator is present who can observe the waveform to discriminate between artifacts and EMG, so that the surgeon is alerted only when there is evidence of facial nerve stimulation.
Unfortunately, the nerve cannot be monitored reliably under all conditions. Poorly grounded equipment such as electric drills, electrocautery, and anesthesia instruments may increase background electrical noise to such an extent that the facial EMG is obscured, particularly if the EMG is abnormally small. Electrocautery generates signals so large that electrical monitoring is not possible during cautery, even though cautery can damage the nerve. Under these conditions, partial or complete loss of facial function can occur without being detected. At these times, facial muscle contractions are detected by the anesthesiologist placing a hand on the patient’s face or by the use of mechanical tranducers to detect facial movement. It is important to note that persistent heating of the nerve by drilling without irrigation and rest will make the nerve less likely to respond if damaged.
The condition of the patient also affects the quality of the monitoring. Preexisting nerve dysfunction may not be readily discerned during a clinical evaluation, but it can reduce EMG amplitudes. Although it may be possible to monitor patients with paresis as low as House grade IV, the procedure will be much more susceptible to artifacts; consequently, reliability will be greatly diminished. These conditions can be anticipated by preoperative electroneurography. Care must be exercised in the use of muscle relaxants, because their very action is to reduce the responsiveness of the muscles being monitored. When excessive, they may prevent monitoring altogether.
During passive monitoring, the role of the operator is to detect any signs of facial nerve irritation. When the nerve is encountered, a sudden burst response, bipolar in morphology, is seen. The underlying timing of nerve firing is slow enough so that when amplified and presented through a loudspeaker a characteristic low-frequency sound can be heard. Such sounds can occur from touching or transecting the facial nerve. The differences in response between a brief touch and complete division of the facial nerve are slight. A continuous “growling” sound has been associated with irritation of the nerve (e.g., stretching of the nerve or sudden change in temperature).
Active monitoring with a stimulating probe may be used by the surgeon whenever there is a need to locate the nerve and differentiate it from surrounding tissue. The monitor assists by adjusting current levels of the stimulator, discriminating CMAPs from artifacts, and reporting on the relative sizes of CMAPs. By varying the probe location and the current, the amplitude of the CMAP can often reveal the precise location of the facial nerve. In the case of a nerve enveloped in cholesteatoma or other soft tissue, for example, the monitor operator will reduce the stimulus current to a very low level (0.1 to 0.4 mA) so that the probe will only stimulate if it is directly on the nerve. In this way the surgeon can systematically probe each piece of tissue before excising it. Because bone is a poor electrical conductor, the nerve within the intact bony canal cannot be reliably stimulated or localized with this method. Very high current levels are nonlocalizing because they can produce a maximum CMAP over a wide area. However, as the bone overlying the nerve is thinned, the stimulator becomes more effective, so that current level can sometimes be used to assess the relative thickness of the remaining bone.
CEREBELLOPONTINE ANGLE SURGERY: FACIAL AND HEARING MONITORING
Facial Nerve Monitoring
Cerebellopontine angle tumor resection is done by our surgeons, employing either the posterior or middle fossa approaches. In the past the posterior fossa approach had been used almost exclusively (11); more recently the middle fossa operation is being used for small intracanalicular tumors when hearing preservation is paramount. However, there may be a small increased risk of facial nerve injury with the middle fossa approach (12).
Anesthetic Considerations
Although the facial nerve can be stimulated and facial movements detected while patients receive low-dose muscle relaxants (13), to optimize monitoring sensitivity, no muscle relaxant should be used after intubation. Anesthesia is maintained with intravenous anesthetics such as propofol and remifentynl. Once tumor removal is complete and dural closure has begun, muscle relaxants may be used freely.
Localization of the Facial Nerve
Unlike mastoid and middle ear monitoring, direct electrical stimulation of the facial nerve is detected with facial movements rather than the CMAP. The facial nerve is electrically stimulated in the operative field with a Prass flush-tip monopolar handheld probe (Xomed-Treace, Inc.). The probe is connected to a Montgomery nerve-stimulating unit that delivers a continuous 60-Hz constant-voltage sinusoid whose peak-to-peak amplitude can be varied between 0.1 and 1 volt (14). The patient’s Bovie pad completes the circuit. This mode of stimulation results in a tetanic facial nerve discharge pattern, which induces a facial movement that can be detected. To locate the facial nerve, stimulation of the tumor capsule is typically initiated with one volt, whereas stimulation within the tumor capsule begins with 0.3 or 0.5 volts. Once facial movements are detected, the nerve is located by remapping the region using progressively lower voltages until only a very restricted region evokes facial movements.
Detection of Facial Nerve Activation
Three complementary techniques are used to detect facial nerve activity.
Electromyography
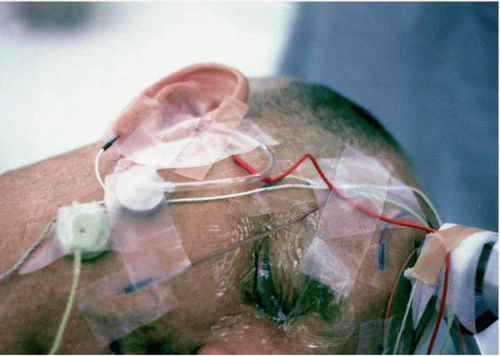
Electrical myogenic activity from 13-mm intramuscular needle electrodes is recorded routinely from two muscles innervated by the ipsilateral facial nerve, namely, the orbicularis oculi and orbicularis oris (15,16). A contralateral forehead electrode serves as the reference (Fig. 7.2). For larger acoustic neuromas, the trigeminal nerve is monitored with an additional EMG channel recording from an electrode in the trigeminally innervated ipsilateral masseter muscle. An ipsilateral forehead electrode provides the isolated ground for the amplifiers. All electrodes are secured to the face with tape and connected to a biopotential-isolated electrode board. EMG signals are then amplified, filtered (30 to 1,000 Hz), and displayed on both an oscilloscope and a chart recorder. The multichannel oscilloscope sweeps at 5 msec/cm and is triggered by line voltage. An eight-channel pen recorder set to paper speeds of either 5, 50, or 500 mm/min continuously records each EMG channel, as well as electrocardiograph (ECG) and arterial blood pressure. EMG activity is audible from the sound of the chart recorder pen movements. A special circuit shuts off all pens whenever electrocautery is in use.
Mechanical Detection of Face Movements
Because the EMG is swamped by the electrical signal from electrocautery and irreversible facial nerve damage can occur if cautery is too close to facial nerve fibers, alternative methods of detecting facial nerve activation are necessary during cautery. We use a motion detector (accelerometer housed in a button-shaped plastic casing) taped to the ipsilateral cheek (Fig 7.2). It generates a voltage with any movement (17,18); in this way, facial muscle contractions are readily detected. In fact, facial motion due to the cardiac cycle can be detected as well and is useful as an indicator that the motion sensor is
operating properly. Other techniques, such as the use of airinflated rubber sensors (19) or strain-gauge clips attached to the cheek, can serve the same purpose (20).
operating properly. Other techniques, such as the use of airinflated rubber sensors (19) or strain-gauge clips attached to the cheek, can serve the same purpose (20).
In our arrangement the output from the motion sensor triggers a strobe light whenever the face moves, thereby immediately alerting the surgeon. The accelerometer output is also recorded on the chart recorder as a permanent record of facial movements.
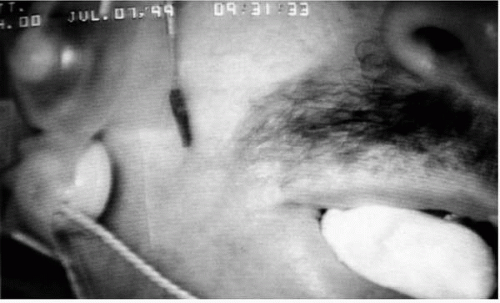
Video Monitoring of Facial Movements
A closed-circuit video system is routinely used as a third technique for monitoring facial movements (Fig. 7.3). The patient lies supine with the head turned to the side so that the ipsilateral ear is superior and almost horizontal. The head is secured by a Mayfield frame to which all lead wires are taped. The endotracheal tube exits from the contralateral side to avoid distortion of the ipsilateral face. The surgical drapes are kept off the face with a metal frame, so that the face can be observed at all times. A fiber-optic light illuminates the face, and a closed-circuit video system records the image of the face, which is displayed along with the video output from the operating microscope.
When EMG is not available, this technique is most useful as a complement to the motion detector because it can clarify the source of movement. During direct electrical stimulation of the nerve with electrocautery, simultaneous activation of both the facial nerve and the motor division of the trigeminal nerve can occur if a large acoustic neuroma displaces the facial nerve toward the trigeminal. In such a case, viewing the video monitor can indicate whether the motion sensor output is signaling face or jaw movements. Movement of the upper and lower lips indicate facial nerve stimulation, whereas jaw movements point toward trigeminal nerve stimulation. Other occasional uses of directly viewing the face include observing horizontal eye movements (through the closed eyelid), indicating abducens nerve stimulation. Shoulder and neck movements from spinal accessory nerve activation or tongue movements due to hypoglossal nerve activation can also be observed by closed-circuit monitoring. Fasciculations of facial muscles occurring while tumor is dissected off the facial nerve can be observed synchronous with EMG activity, and signs of facial movements due to light anesthesia can also be detected.
Case Study
Figures 7.4, 7.5, 7.6, 7.7, 7.8 and 7.9 illustrate for one patient (no. 1123) the use of facial nerve monitoring during the total removal of a 2-cm acoustic neuroma via the posterior fossa approach; the postoperative facial function was normal. The first step prior to any tumor removal is to map the surface of the tumor capsule with the nerve stimulator. When 1 volt was applied to the superior portion of the tumor capsule, facial movement was detected by the motion sensor and could be seen on the video monitor. This area of the capsule was then restimulated using 0.3 volts (Fig. 7.4); facial movements occurred again but in a more restricted region. This result indicated that the facial nerve was displaced over the superior-posterior portion of the tumor—an infrequent finding that can be associated with a poor prognosis. On closer inspection of the region of stimulation, the nerve could be seen as a thin band. By electrically mapping the surface of the capsule prior to dissection, injury to the facial nerve was avoided.
The dissection then proceeded, with special care taken to avoid the region where the facial nerve could be stimulated. While dissecting the tumor in another location using bipolar cautery, movement of the face was detected by the motion
sensor and the strobe light flashed. The dissection was then halted, and the stimulator was used to locate the course of the nerve in this region (Fig. 7.5).
sensor and the strobe light flashed. The dissection was then halted, and the stimulator was used to locate the course of the nerve in this region (Fig. 7.5).
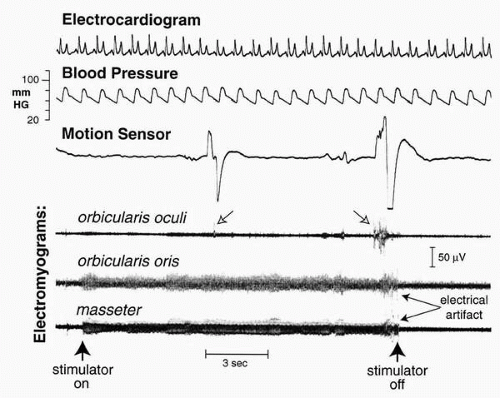 FIG. 7.4 Stimulation of the tumor capsule to locate the facial nerve. Shown are the chart recorder traces while the nerve stimulator is being moved over the tumor surface. The bursts of activity from orbicularis oculi (open arrows) that coincide with large changes in the motion sensor signal indicate that facial nerve fibers are near the stimulator tip. Continuous electrical activity on orbicularis oris and masseter channels is electrical artifact from the stimulator.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|