Chapter 24
INTRAOCULAR FOREIGN BODIES

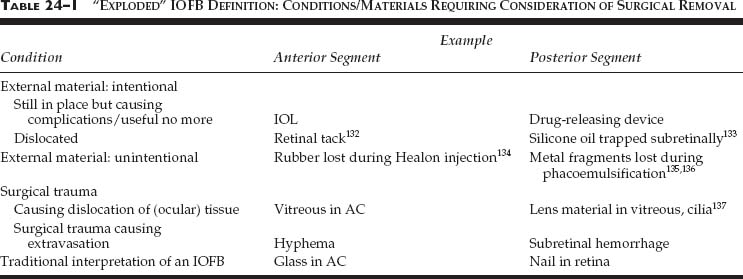
IOFBs are traditionally defined as intraocularly retained, unintentional projectiles, although surgeons commonly remove objects of different types from the eye (see Table 24–1). IOFBs have typically caused so much concern to both patients and health care providers (from ancient barbers to modern ophthalmologists) as to prompt urgent extraction. This urge all too commonly has taken precedence over the most important goal: vision.1
HISTORY
Ferenc Kuhn, Viktoria Mester, and Robert Morris
IOFB extraction dates back thousands of years2; the first successful magnetic IOFB removal was reported in 1624.3 The EEM, introduced by Hirschberg in 1789, became the ultimate tool with a high success rate in extracting fresh ferrous IOFBs, even if these were invisible. The EEM also served diagnostic purposes,4 verifying the IOFB’s magnetic nature by inflicting pain on the unanesthetized patient. The introduction of vitrectomy not only improved the results considerably: it refocused the ophthalmologist’s attention from IOFB removal to complex visual rehabilitation.5
PEARL… The primary goal in managing IOFB injuries is to treat/prevent associated conditions such as endophthalmitis, retinal detachment, and late metallosis. Only occasionally is removal of the IOFB in the vitrectomy era the sole or ultimate purpose of the management; rather, it is the means to preserve vision.
Incidencea:
• 18–41% among open globe injuries6–9 (USEIR: 16%).
Age (years):
• average: 29–388,10–13 (USEIR: 31);
• range: 3–798,10–12 with 66% between 21 and 4014 (USEIR: 2–76 with 61% between 21 and 40 and only 3% being 60).
Sex: males in 92–100%8,10–13,15,16 (USEIR: in 93%). Place:
• work in 54–72%8,12,13,16 (USEIR: 33%);
• home in 30%8,16 (USEIR: 42%).
Cause:
• hammering in 60–80%14–17 (USEIR: 53%);
• power or machine tools in 18–25%14,17;
• weapon-related in 19% (USEIR).
IOFB injury is rare in persons wearing eye protection10,18; in the USEIR, only 3% of patients claimed having safety goggles on when the injury occurred.
PEARL… It is the ophthalmic community’s responsibility to call the public’s attention to the importance of using adequate safety glasses while conducting dangerous activities such as hammering18 and fireworks19,20 or power tool14,17 use (see Chapters 4 and 27).
PATHOPHYSIOLOGY
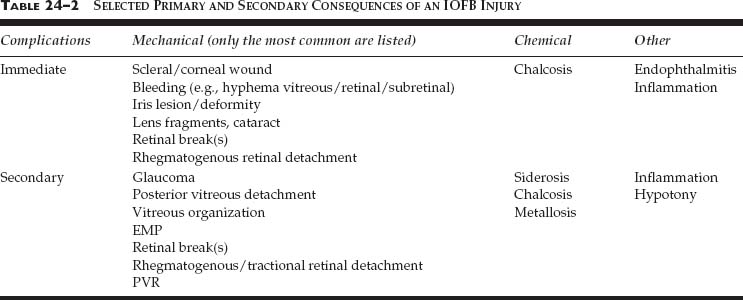
Occasionally, an IOFB has so much momentumb that the damage is incompatible with anatomical reconstruction (see Chapters 8 and 31). However, in the vast majority of cases the injury allows globe preservation via appropriate surgery, during which typically the following consequences must be addressed:
• entrance wound (must have occurred by definition);
• inflammation; and
• immediate and secondary
 physical (mechanical);
physical (mechanical);
 chemical; and
chemical; and
 other complications (e.g., endophthalmitis; see Table 24–2).
other complications (e.g., endophthalmitis; see Table 24–2).
Entrance Wound
The IOFB must possess certain energy to perforate the eye’s protective wall. The length of the entry wound is predictive of the risk of retinal damage: the shorter the wound, the less energy to be lost during penetration (see Table 24–3).
PEARL… Objects entering the eye through the sclera preserve more energy than those entering through the cornea21 and are thus more likely to exit the eye posteriorly (i.e., causing a perforating injury).
Mechanical Intraocular Damage
Little or no damage is expected if the IOFB has completely lost its kinetic energy upon entry. Typically, however, intraocular tissue injury also occurs. The primary impact may be followed by additional impaction(s) via ricocheting (see Table 24–4 and the following). Blunt IOFBs are more destructive than sharp objects.22
| Length of Corneal/Scleral Wound (mm) | Proportion of Eyes with Retinal Injury (%) | |
|---|---|---|
| 3 | 43 | |
| 4–6 | 26 | |
| 7 | 5 |
Source: F. Kuhn and R. Morris, unpublished data from the USEIR.
PEARL… A posterior segment IOFB has a 68% chance of causing one and a 21% chance of resulting in two or more retinal lesions.23
Inflammation
Breach of the eyewall, intraocular hemorrhage, and lens/vitreous admixture, among other lesions, incite an inflammatory response. Inflammation can cause synechia formation and IOP elevation and has been implicated in the development of PVR.24
Chemical Implications
Metallic IOFBs are rarely pure.25 The damage an alloy inflicts is generally proportional to the content of the harmful component.26 Toxicity is more closely related to the active surface area than to the volume of the IOFB.27,c
Siderosis
IOFB-related corrosion is caused by the interaction between trivalent iron ions and proteins primarily in the eye’s epithelial cells. The cytotoxicity involves enzyme liberation and lysosome breakdown, leading to cell degeneration.28 The ferric iron, stored in siderosomes as ferritin, is thought to be toxic by generating free radicals.29
| Location of IOFB | Risk of Development of at Least One Retinal Lesion (%) | Risk of Development of Multiple Retinal Lesions (%) | ||
|---|---|---|---|---|
| Vitreous | 68 | 8 | ||
| Retinal/subretinal | 76 | 29 | ||
| Posterior segment | 68 | 21 |
Siderotic changes include the following clinical findings:
• iron deposits on the corneal endothelium;
• chronic open-angle glaucoma;
• brownish discoloration of the iris, leading to conspicuous heterochromia in people with light-colored irisesd;
• dilated, nonreactive pupil (another common first sign32),e which may also show light/near reaction dissociation and supersensitivity to weak miotics33;
• yellow cataract with brown deposits on the anterior capsule;
• pigmentary retinal degeneration, eventually leading to attenuated vessels and visual field loss; and
• optic disk swelling/hyperemia.34
The clinical diagnosis is confirmed by characteristic ERG changes such as:
• increased A wave initially; and a
• progressive reduction of the B wave subsequently.
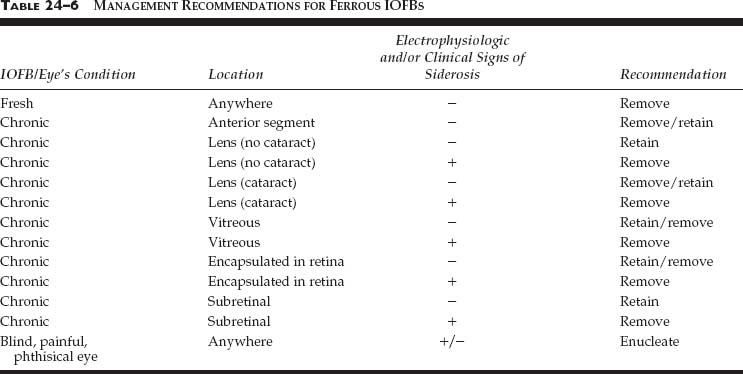
The threat of siderosis is a powerful argument to remove all fresh ferrous IOFBs. Nevertheless, siderosis is not inevitable; see Table 24–5 for various misconceptions. If there is associated IOP elevation despite removal of the foreign body, filtration surgery may be required.
| Myth | Truth | |
|---|---|---|
| All IOFBs with iron content eventually cause siderosis | Neither electrophysiologic nor clinical signs of siderosis are inevitable138,139 | |
| Once siderotic changes occur, they are permanent | Timely removal of the IOFB can improve the visual acuity,140 the visible siderotic changes,138 and the ERG signs; even marked reduction of the ERG B wave may be reversible141 | |
| Intralenticular IOFBs do not cause siderosis | Siderosis has been reported to develop even if the IOFB is intralenticular142,143 as iron eventually may “leak out” from the lens25; these changes can occur as early as weeks after the injury.144 The threat of siderosis is greater when the IOFB is located in the lens periphery40 | |
| Encapsulated IOFBs do not cause siderosis | The fibrous tissue, forming around an intraretinal IOFB usually within 10 days after injury,145 does not necessarily prevent iron dissolution into the inner eye, and severe loss of vision may develop146 | |
| The condition of the eye, once stable, remains so | Intraocular manipulations may dislodge the IOFB and lead to late siderosis development34 |
PITFALL
Rarely, siderosis is caused by objects presumed not to have a free iron content (steel, stone)35–37 and by vitreous hemorrhage.38
It is best to discuss all treatment options with the patient, who must make the ultimate decision in cases of a chronic IOFB with threatening or existent siderosis (see Table 24–6 for our guidelines). If an IOFB is retained, regular follow-up of the informed patient is necessary using visual acuity, slit lamp, IBO, ERG, and diagnostic x-ray spectrometry.39 The ERG is especially important because electrophysiologic signs of siderosis may arise earlier than clinical changes.40 If the patient is not expected to return for follow-up, IoFB removal should be recommended.
Chalcosis
PITFALL
Although uncommon, copper IOFBs cause particular concern because they can elicit a rapid, sterile, but endophthalmitis-like reaction41 including corneal/scleral melting, hypopyon, and retinal detachment.2,42 Untreated, this violent response may lead to loss of vision within a few hours,2,f eventually leading to phthisis.43
Once the danger of the acute reaction has passed, however, the risk of toxicosis drops dramatically and the IOFB may be tolerated for many years without complications.
Copper tends to deposit in membranes (e.g., Descemet’s, lens capsules, ILM2,44) and causes destruction by increasing lipid peroxidation.26 The typical clinical findings include:
• copper particles in the aqueous;
• green discoloration of the iris;
• greenish/brown-colored sunflower cataract with spokes of copper deposits radiating from a central ring;
• copper particles in the vitreous; and
• copper deposits on the retinal surface.2
Unlike siderosis, chronic chalcosis rarely leads to blindness, and even the associated cataract does not severely impede vision. Improvement may occur spontaneously or after surgical removal45; conversely, the chalcosis may intensify despite successful IOFB removal due to the intraocular retention of copper powder2.
“Inert” Substances
Substances generally well tolerated inside the eye (e.g., gold, glass, plastic, porcelain) may on occasion cause substantial damage40:
• hot plastic can lead to massive foreign body reaction and eventual loss of the eye46;
• aluminum may result in metallosis42;
• sharp edges of glass can inflict secondary mechanical damage47;
• lead may result in medically uncontrollable glaucoma48;
• nucleus material left in the vitreous after cataract surgery may cause a foreign body reaction49 (see Chapter 21).
EVALUATION
Based on a detailed history, inspection at the slit lamp and by ophthalmoscopy, and certain diagnostic tests (see later in this Chapter and Chapter 9), the ophthalmologist should (be able to) determine whether an IOFB is indeed present. The medicolegal implications are considerable; missed IOFBs constitute up to 56% of all trauma-related legal claims (see Chapter 7).50 The following basic questions must be answered:
• Is there a foreign body?
• Is the foreign body truly in the eye (IOFB) or is it in the orbit?
• Are there multiple IOFBs?
• Exactly where inside the eye is the IOFB situated?
• What were the circumstances of the injury?
• What associated conditions are present (e.g., endophthalmitis, vitreous hemorrhage) or threaten (e.g., retinal detachment)?
PITFALL
Multiple IOFBs are especially common in young patients,51 in cases of explosion or war trauma,52 and in MVCs if the windshield is not laminated.53
History
Ask specific questions to determine the circumstances of the injury (when, where, how, by whom and what, distance, energy, material, etc.), and keep in mind that:
• most patients seek medical attention shortly after injury because of pain and/or visual complaints;
• if the history is suspicious but no IOFB is found, it is best to continue the search for an elusive IOFB54,55;
• IOFBS may not be discovered until siderotic signs appear33.
PITFALL
An estimated 20% of the patients do not experience pain,53–55 and vision may remain excellent.33 Children, observers, and passers-by are especially susceptible to being unaware of the injury, even if specifically asked,56 and are prone to late presentation. In addition, IOFBs may be present despite a negative history57 because the person is in denial (see Chapter 30); IOFBs as large as 13 × 1 mm have gone undetected.56 The physician should suspect an IOFB in virtually all cases of open globe injury.58
External Inspection and Slit Lamp
An anterior entrance wound is commonly visible to the naked eye (use a penlight if necessary) or there may be warning signs (e.g., hemorrhage over the sclera, localized corneal edema, nonsurgical hole in the irisg).
PITFALL
Even in fresh cases with fairly large IOFBs, the entrance wound may be impossible to find,56,59 especially if the wound is posterior.
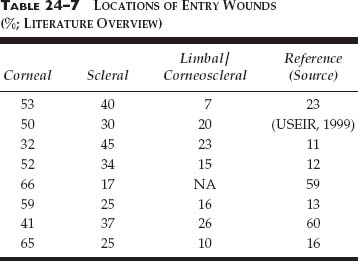
Reports on wound size vary widely (1 to 17 mm16,60); most wounds are <5 mm. Slit-lamp biomicroscopy is mandatory, and a 90–diopter lens can provide additional information regarding IOFB position and com-position as well as the associated intraocular damage. Gonioscopy, performed after wound closure, may also be helpful (see Table 24–7 for literature data on the distribution of the entry sites).
PEARL… Even in inside-out (i.e., rupture) or apparently closed globe injuries, or in the presence of uveal prolapse14 or lens dislocation,61 IOFBs can be present.
Ophthalmoscopy
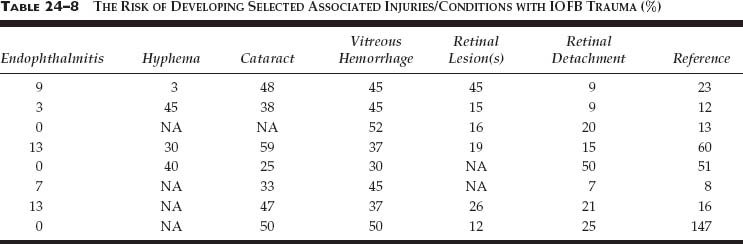
By also showing the damage to intraocular tissues (see Table 24–8 for literature data on risk factors) and the IOFB’s relationship to these tissues, information provided by direct visualization is superior to that by any other diagnostic technique.10 Especially if located anteriorly, however, IOFBS may be missed, even in the presence of clear media.29
Ultrasonography
In the hands of an experienced clinician, ultrasonography is a very effective method to detect the presence and location of even nonmetallic IOFBs. It is the best indirect method to find associated tissue injuries such as choroidal and vitreous hemorrhages and retinal detachment10,62 and to follow eyes after the primary repair.
PITFALL
False-negative results are possible on echography if the IOFB is small, wooden, or of vegetable matter, and a false-positive result may be found in the presence of gas bubbles.10,62
With extreme caution, ultrasonography may be performed on eyes with an open wound;63 alternatively, it is used on the operating table once the wound is closed. The B scan tends to overestimate the size of the IOFB and should not be used for measuring purposes.64
For finding and localizing small, nonmetallic IOFBS in the anterior segment, ultrasound biomicroscopy is superior to CT, MRI, and contact B-scan ultrasonography.65,66 It is limited in its ability, however, to distinguish between different materials and cannot be used if the globe has an open wound.65
Radiology
Plain X-Ray
Although still widely used, this traditional method is slowly being replaced by CT as the primary radiological diagnostic tool. Inaccuracies have been described in numerous individual case reports and large studies.17,31,67–73 Screening by plain x-ray has been found unnecessary.74 Dental x-ray is more helpful by virtue of its bone-free image.
CT
With a sensitivity of 45 to 65% for IOFBs < 0.06 mm3and of 100%75 for IOFBs >.06 mm3, CT is the best indirect method for both detecting and localizing IOFBs. Appropriate software and technique allow some differentiation of IOFB composition, although CT still cannot distinguish between various types of metals.62,76,77
PITFALL
CT can miss plastic,78 even metallic79 IOFBs, especially if too wide cuts are used or the eye moves during the procedure.67 Wood may cause problems by giving an image similar to that caused by air. Conversely, a false-posi-tive finding can also occur (see Fig. 24–1).
Although both are able to find IOFBs as small as 0.048 mm3,75 helical (spiral) CT:
• provides an image superior to that of a conventional axial CT80,81;
• has a shorter examination time;
• has the ability to reconstruct coronal/sagittal images without further scanning; and
• reduces motion artifacts and radiation.82
MRI
A powerful tool for cross-sectional and soft-tissue analyses, MRI is very sensitive in detecting IOFBs, allowing discovery even when performed for nonophthalmological indications.83
CONTROVERSY
The literature is rather confusing in determining whether MRI is safe in cases of ferrous IOFBs.h Some reports found that IOFB movement is rare,85 whereas others have shown that movement is not only very common86 but may occur even when the test is performed for distant body problems such as a lumbar spine herniation.87 Furthermore, damage due to IOFB movement during MRI has not been seen by some authors88 but reported to occur by others.89
PITFALL
The most important diagnostic question is whether the foreign body is intra- or extraocular. Unfortunately, the margin of error of radiological methods is greatest when the object is closest to the eyewall. Personal consultation with the radiologist 6efore the test is conducted and making an effort to personally read the test resultsreduce the incidence of radiological errors.
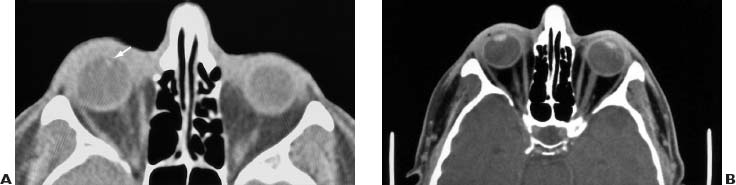
FIGURE 24–1 Even a positive CT finding is not infallible. (A) Preoperative CT scan; the radiologist described an IOFB 3 mm from the surface inside the right eye (his arrow is still visible on the scan). Careful investigation failed to detect the IOFB during vitrectomy. (B) Postoperative CT scan shows a right orbit without any foreign object.
Metal Detectors
Having been supplanted by superior diagnostic methods90 or because they are not commercially available,39 metal detectors are rarely used today.
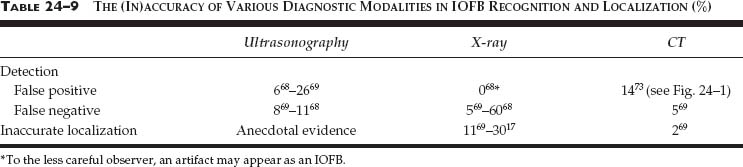
Table 24–9 summarizes certain shortcomings of ultrasonography, plain x-ray, and CT; Table 24–10 shows some of the potential diagnostic traps, threatening even when different evaluation methods are combined.10 It must be emphasized that in the vitrectomy era:
• accurate preoperative IOFB localization is less important;55 and
• the IOFB may move from its predetermined position before or during surgery.37
PITFALL
If an IOFB is not found during surgery, the most likely locations are behind the iris in the vitreous cavity at 6 o’clock, subretinally, or in the angle, in which case only gonioscopy may help in discovering it.i
MANAGEMENT STRATEGY AND COUNSELING
Before designing and discussing with the patient the management plan, all data must be analyzed carefully to answer the following crucial questions:
• Is this a high-risk injury?j If yes, immediate intervention is advised.
• Is a retinal break and/or detachment present? The more likely that retinal damage has occurred (see Table 24–4), the more urgent the intervention. If media opacity prevents retinal visualization, use indirect clues such as:
 wound length (see Table 24–3);
wound length (see Table 24–3);
 circumstances of the injury (the greater the kinetic energy of the object and the sharper it is, the more likely that deep penetration has occurred); and
circumstances of the injury (the greater the kinetic energy of the object and the sharper it is, the more likely that deep penetration has occurred); and
 wound location (i.e., corneal vs. scleral).
wound location (i.e., corneal vs. scleral).
Additional helpful factors to consider are:
• IOFB characteristics (see Table 24–11);
• risks and types of associated intraocular tissue damage (see Table 24–8);
• the surgeon’s experience, expertise, and the equipment available; and
• the legal environment.
| Trap | Reference | |
|---|---|---|
| IOFB masquerading as globe rupture | 148 | |
| IOFB masquerading as idiopathic chronic iridocyclitis | 57,149 | |
| IOFB masquerading as a choroidal melanoma, even as one with extrascleral extension | 72,150,151,152 | |
| IOFB causing subretinal neovascularization | 153 | |
| Ocular calcification masquerading as IOFB | 154 | |
| Encapsulated preretinal hemorrhage masquerading as IOFB | 155 |
| Variable | Findings | Reference (Source) | ||
|---|---|---|---|---|
| Number | 58% in posterior segment | (USEIR, 2000) | ||
| 13–24% in anterior segment | 8,9,17,60,97 | |||
| 7–10% in lens | 8,17,156 | |||
| 25–48% in vitreous | 8,17,60,97 | |||
| 16–44% in retina | 8,17,60 | |||
| 52% retina and choroid | 92 | |||
| 0–15% subretinally | 8,16,60 | |||
| Size (mm) | Average: 3.5 (range: 0.5–25) | 60,97 | ||
| 73%>3 | 97 | |||
| 45% ≥ 2 | 13 | |||
| 2×1 to 5×9 | 11 | |||
| Material | 41–89% magnetic | 10,11,12,14,60 | ||
| 78–100% metallic | 9,10,11,12,60 | |||
| 5–18% glass | 8,9,60 |
PITFALL
A surgeon unfamiliar with the techniques of comprehensive globe reconstruction should notattempt removal of a posterior segment IOFB (see Chapter 8).
FIGURE 24–2 shows the management options; remember that:
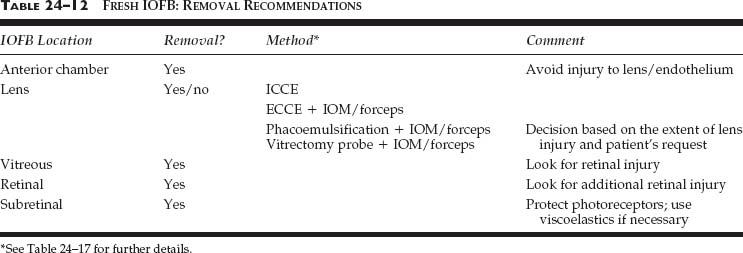
• if they are fresh, even inert IOFBs are best removed (see Figs. 24–3 and 24–4, and Table 24–12);
• if IOFB removal is decided upon and the eye shows associated tissue damage, it is better to perform complex reconstruction simultaneously than as a secondary reconstructive procedure because:
 vision is not improved just by IOFB removal;14 and
vision is not improved just by IOFB removal;14 and
 the risk of endophthalmitis is reduced only if the “cultured media” (i.e., vitreous) is also promptly removed9,23;
the risk of endophthalmitis is reduced only if the “cultured media” (i.e., vitreous) is also promptly removed9,23;
• in cases of posterior segment IOFBs, a decision must be made whether to perform vitrectomy:
 the more extensive the intraocular tissue damage, the more vitrectomy is indicated to treat existing lesions and to prevent subsequent retinal detachment91;
the more extensive the intraocular tissue damage, the more vitrectomy is indicated to treat existing lesions and to prevent subsequent retinal detachment91;
 an IOFB invisible due to vitreous hemorrhage is an absolute indication.
an IOFB invisible due to vitreous hemorrhage is an absolute indication.
In addition, decisions must be made regarding:
• instrumentation (see later in this Chapter);
• timing (see later in this Chapter); and
• the use of prophylactic antibiotics (see Chapter 28 and the Appendix).
General anesthesia is preferred, especially if the IOFB is in the posterior segment. If the intervention is urgent (high-risk case) and the patient ate recently, alternative methods are available (see Chapter 8).
SO has become so rare (see Chapters 8 and 29) that we feel it justified not to consider it as a major factor when the management plan is designed. The patient must nevertheless be fully informed (see Chapter 7), especially when deciding whether to retain a permanently blind eye, and careful follow-up is always advised.
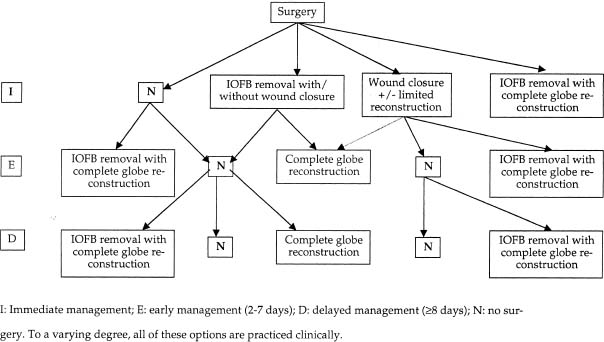
FIGURE 24–2 Flowchart showing the management options in eyes with IOFB injury.
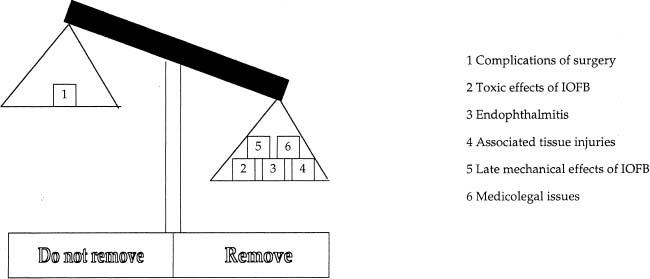
FIGURE 24–3 Scaling the decision whether to perform surgery to remove an acute IOFB.
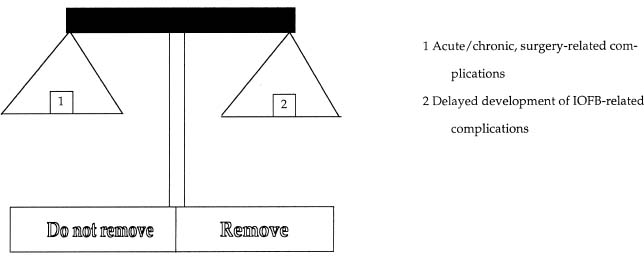
FIGURE 24–4 Scaling the decision whether to remove a chronic IOFB, which causes no visual complaints, no signs of metallosis, and no electrophysiologic alterations.
Literature data regarding the optimal time for intervention are conflicting. Endophthalmitis prevention is the primary goal (Table 24–13), for which as early surgery as reasonably possible is recommended for both medical and legal reasons.k Conversely, a recent study has confirmed earlier reports that there is no difference whether surgery is performed in the first 48 hours or later.92 Delaying the intervention never-theless requires vigilance (see Chapter 28) to quickly note signs of a developing infection.l
PEARL… The vast majority of eyes that develop endophthalmitis do so before the patient presents.9,10 With time, the risk of endophthalmitis development is rapidly and dramatically reduced.
• IOFBs in the AC are usually removed at the time of primary repair.
• Intralenticular IOFBs are typically extracted in conjunction with cataract removal.
• IOFBs in the posterior segment require careful analysis of the risks and advantages (see Table 24–14).
Certain additional factors to consider (see Chapter 8 for details):
• less experienced surgeons may want to delay the intervention because:
 the earlier the surgery is performed, the greater the danger of the development of difficult-to-control intraoperative hemorrhage;
the earlier the surgery is performed, the greater the danger of the development of difficult-to-control intraoperative hemorrhage;
 spontaneous detachment93 makes the critical step of posterior hyaloid face removal technically easier42 while significantly improving the prognosis94;
spontaneous detachment93 makes the critical step of posterior hyaloid face removal technically easier42 while significantly improving the prognosis94;
 early intervention may reduce91 the current 11%24 incidence of PVR development;
early intervention may reduce91 the current 11%24 incidence of PVR development;
• especially in cases of central corneal wounds, edema may initially prevent adequate visualization; intensive steroid therapy can substantially improve conditions in just a few days;
• the delay should not exceed 14 days: a few weeks will increase almost fourfold the risk of proliferation and subsequent tractional retinal detachment93;
• no statistically significant visual/anatomical difference is seen whether vitrectomy is performed during the first or the second week after injury8;
• spontaneous posterior hyaloid detachment may occur in a few days,95,m especially if vitreous hemorrhage is present.96
SPECIAL CONSIDERATION
Should the ophthalmologist perform emergency surgery on a patient presenting at 10 PM with a normal-risk injury or can the intervention be delayed until the morn-ing? Take into consideration the tissue damages as well as the surgeon’s expertise and experience, the staff/equipment available at night versus in the morning, the patient’s general condition, and the legal environment.