Intranasal Trauma and Epistaxis
The majority of children who present to the clinician with epistaxis can be treated medically with ointments and saline. This chapter demonstrates surgical techniques for those who have ongoing recurrent or severe epistaxis despite medical management.
10-1 Evacuation of Septal Hematoma and Abscess
Introduction
Septal hematomas may develop following blunt nasal trauma. The septum is often fractured, but not displaced. Blood collects between the perichondrium and cartilage on one or both sides of the nose. A septal abscess can result from a hematoma that is not promptly drained.
Indications
Hematomas and abscesses must be drained expeditiously to prevent septal cartilage necrosis with loss of nasal support and a resultant saddle nose deformity.
Preoperative Evaluation
Preoperative evaluation consists of a thorough intranasal examination, recognition of the abscess or hematoma, and evaluation for associated facial and cranial trauma.
Operative Technique
1. General anesthesia is recommended in children in order to accomplish complete evacuation of the hematoma.
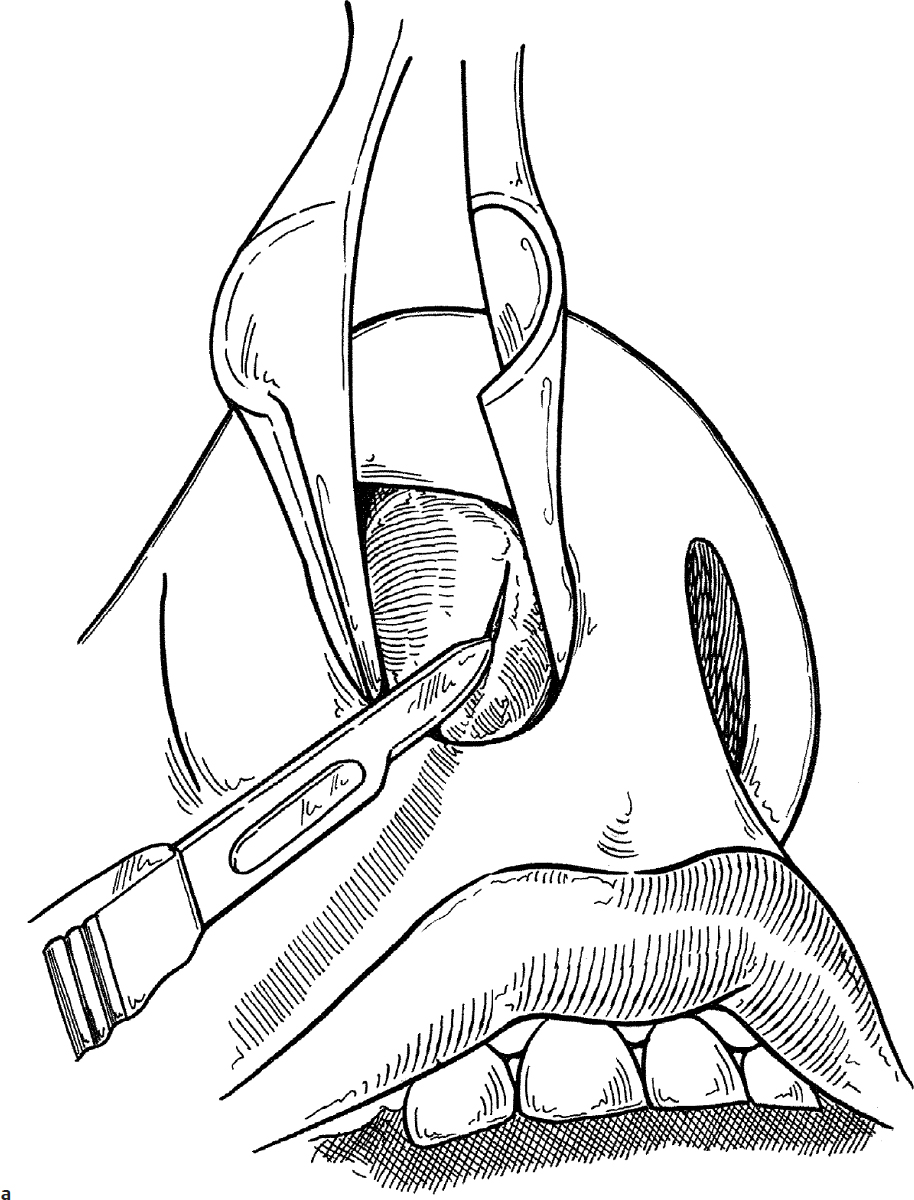
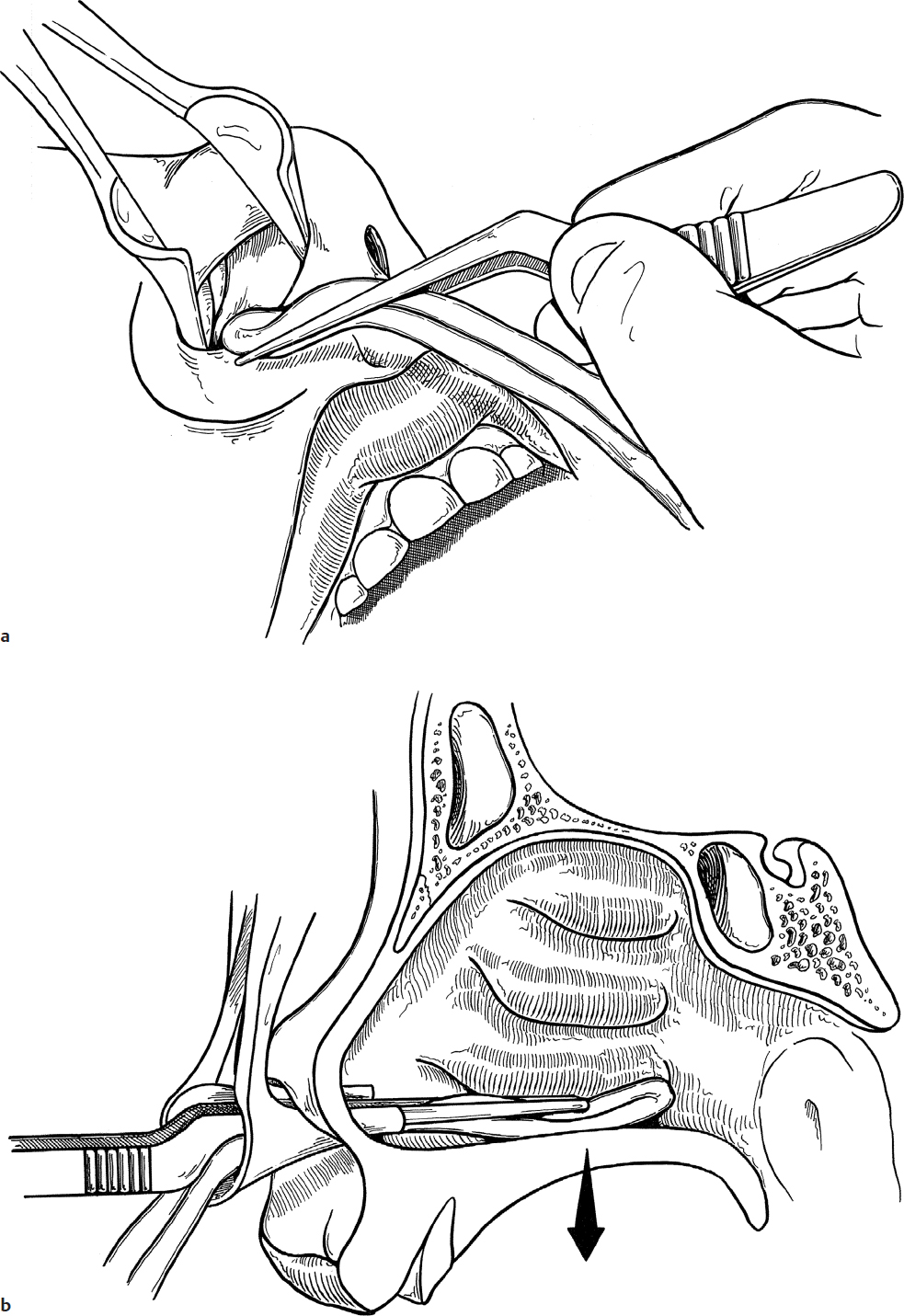
2. An incision is made at the caudal edge of the fluctuance (Fig. 10.1a).
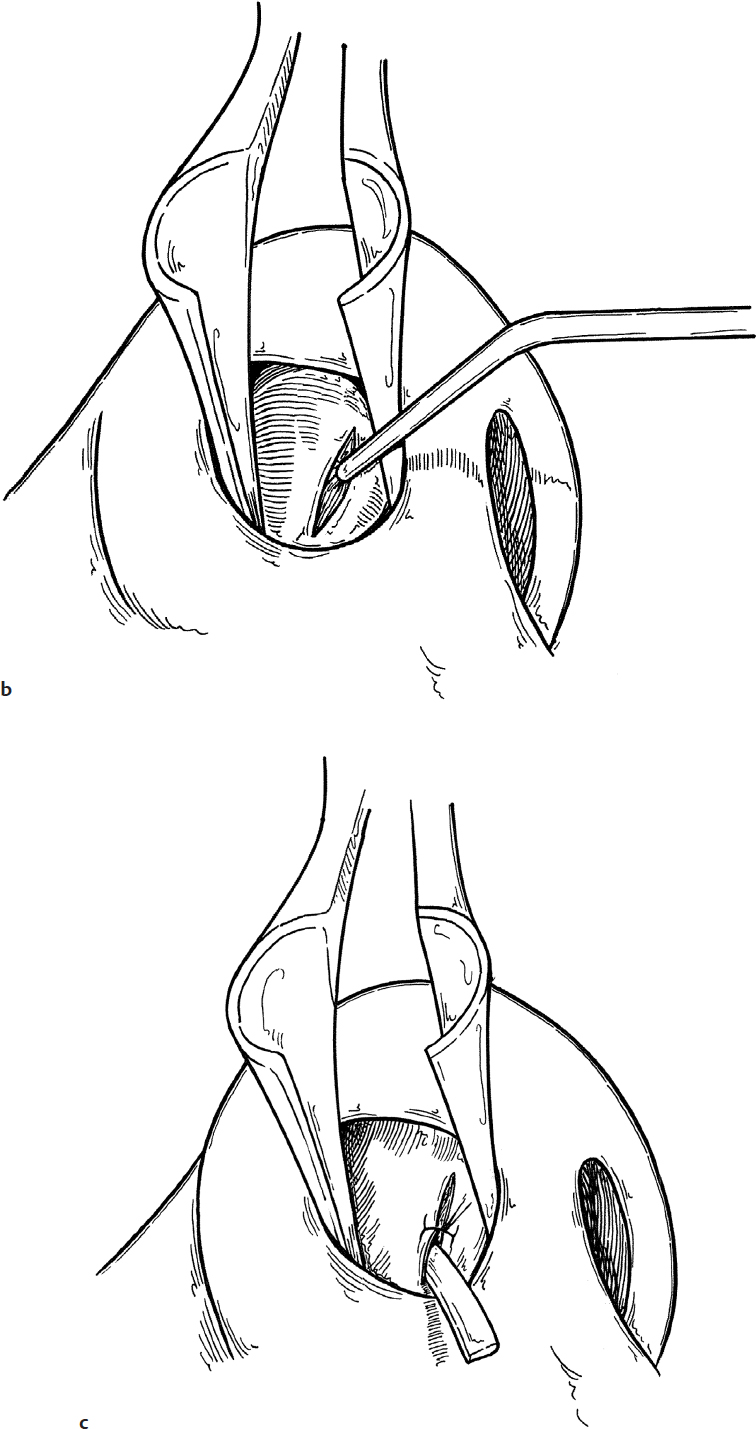
3. The contents of the hematoma or abscess are removed by suction and, if necessary, gentle curettage (Fig. 10.1b).
4. A cut rubber band drain is placed in the cavity and brought out of the bottom of the incision. The incision is closed loosely with one 5-0 chromic suture (Fig. 10.1c).
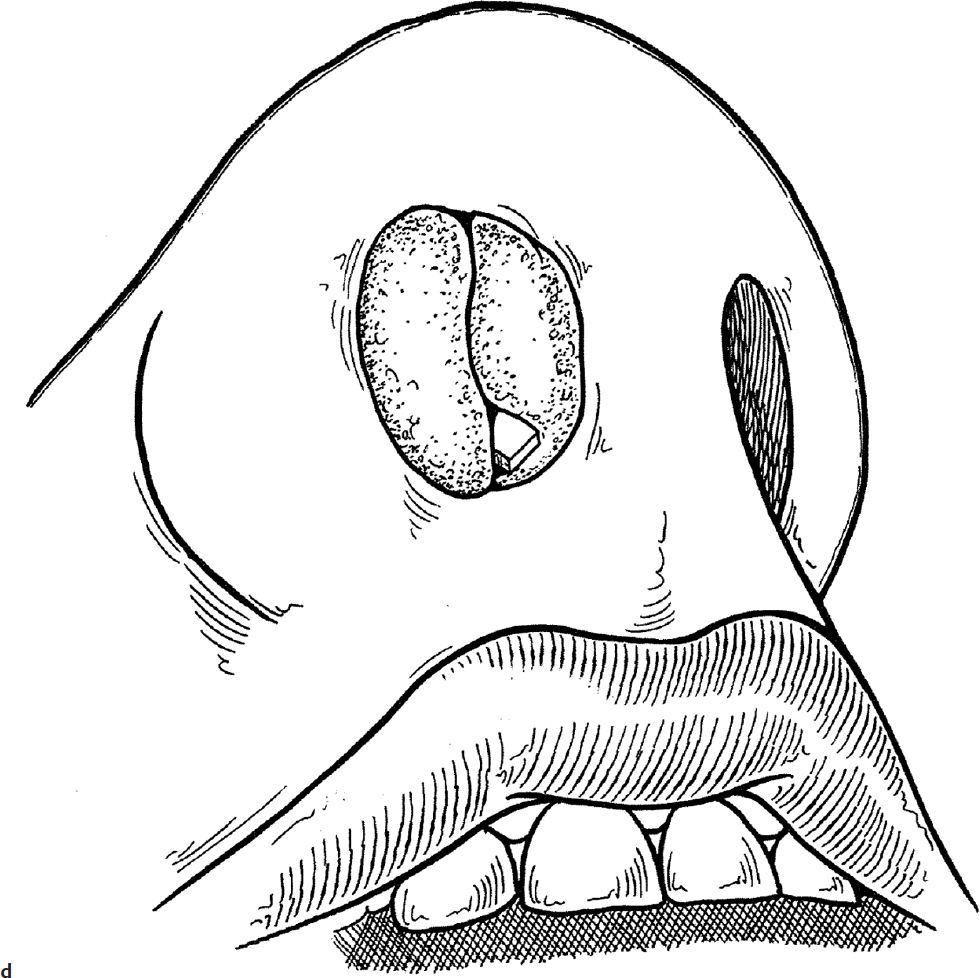
5. The nose is then packed with Gelfoam (Pfizer), Surgicel (Ethicon), or gauze to approximate the perichondrial flap to the cartilage. Antibiotic-impregnated gauze may be used in older children, but biodegradable material is easier to remove in the young child (Fig. 10.1d). Both the drain and the packing are removed in 2 days.
6. Ten days of oral antistaphylococcal antimicrobial treatment are indicated when treating a child with septal abscess or hematoma.
Complications
1. Saddle nose deformity
2. Septal perforation
3. Reaccumulation of hematoma/abscess
10-2 Nasal Cautery
Introduction
Epistaxis is a common problem of childhood and adolescence. Most episodes stop spontaneously or with gentle pressure. However, recurrent epistaxis can be debilitating because of its frequency and/or severity. In those instances, surgical intervention is required.
Indications
Cauterization is indicated in those cases of recurrent epistaxis that do not respond to conservative methods of humidification and topical ointments.
Preoperative Evaluation
The preoperative evaluation of a patient with recurrent epistaxis must include a thorough examination of the nose and nasopharynx. This is essential to identify hemangiomas, neoplasms (e.g., juvenile angiofibromas), septal deflections, or foreign bodies that may be the cause of the epistaxis. If there is a strong family history of bleeding, then a referral to Hematology is necessary preoperatively. A complete coagulation profile does not rule out the more common causes of mild bleeding disorders, such as von Willebrand’s disease. Radiographic examination of the sinuses and pharynx may be done. While plain films can demonstrate large masses, computed tomography (CT) affords the best radiographic view of the nose and sinuses.
Operative Technique
1. Nasal septal cauterization in children is most effectively accomplished utilizing general anesthesia.
2. The nose should be cleared of all debris and clots before cotton pledgets soaked in 4% cocaine are applied to the bleeding area (alternately, any combination of a topical vasoconstrictor and local anesthetic may be used). This provides a dry field for cautery. If there is no active bleeding, this step may be unnecessary.
3. The septal blood vessels feeding the bleeding area are cauterized individually with a protected suction or needle-point cautery or hyfrecator (Fig. 10.2).
4. Cauterization of only the feeding vessels provides the best control of epistaxis, allows rapid healing, and avoids a large mucosal burn that may result in atrophic mucosa or a septal perforation.
5. Antibiotic ointment should be applied to the cauterized area twice daily until the site has healed, usually 7–10 days.
Complications
1. Continuing epistaxis
2. Septal perforation
10-3 Anterior Nasal Packing
Indications
When active epistaxis is not controlled by measures such as gentle pressure or silver nitrate cautery, nasal packing may be required. The source of the bleeding is usually from the superior septal vessels or the lateral wall of the nose. Both sides of the nose should be packed for maximum control and stabilization of nasal structures.
Preoperative Evaluation
No further preoperative evaluation is needed (see Section 10-2).
Operative Technique
1. Because bleeding is uncontrolled, packing the nose is urgent and performed utilizing a topical anesthetic.
2. Mucoid debris and blood clots should be cleared from both sides of the nose with a suction.
3. The nasal mucosa should be anesthetized and vasoconstricted with 4% cocaine-soaked neurosurgical pledgets (alternately, any combination of a topical vasoconstrictor and local anesthetic may be used). Three 1/2″ × 3″ pledgets on each side of the nose are usually sufficient.
4a. In some cases, bleeding can be controlled with absorbable packs and may be the preferred treatment in children with bleeding disorders. These commercially available agents include oxidized cellulose (Surgicel), absorbable gelatin sponge (Gelfoam), or agents with a combination of gelatin matrix and thrombin (FloSeal; Baxter).
4b. A 1/4″ × 72″ gauze strip is impregnated with antibiotic ointment by rubbing the ointment into the gauze.
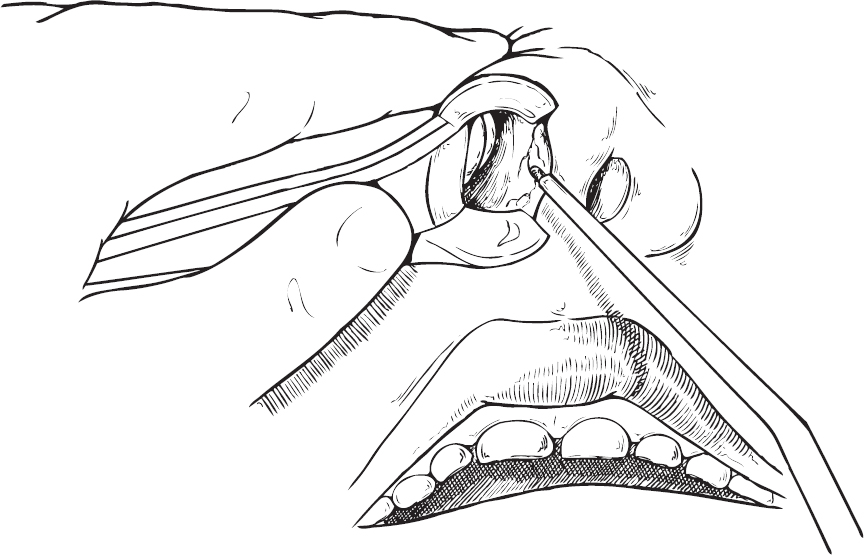
5. The nasal cavity is then packed by grasping the gauze with a bayonet forceps and placing it deep in the nose (Fig. 10.3a).
6. The packing is pushed down against the floor of the nose (Fig. 10.3b).
7. Each side of the nose is packed in a similar fashion: layering the packing from the floor of the nose toward the top of the nasal cavity. The final portion of packing is placed anteriorly (Fig. 10.3c).
8. Alternately, commercially available expanding sponge packs may be used instead of gauze packing to control anterior hemorrhage, including Merocel packs (Medtronic). Some prefabricated packs also have balloons that can be inflated to control anterior bleeding.
9. The packing is kept in place by taping the nose across the nostrils. It is removed after 72 hours (Fig. 10.3d).
10. Antistaphylococcal antibiotics are administered for 7–10 days to prevent the occurrence of toxic shock syndrome that has been associated with nasal packing.
Complications
1. Continuation of bleeding
2. Mucosal abrasion