Chapter 27
INJURY TO THE POSTSURGICAL EYE

Eye injuries are common and expensive (see Chapter 4),1–4 making it essential for society to determine whether and how common surgical procedures affect the globe’s resistance to trauma. A few of the most obvious questions include the following.
• How much force does it take to penetrate or rupture the eye?
• Is the postsurgical eye more prone to serious injury? If so, how much?
• What is the velocity difference between paintballs causing contusion versus rupture?
• When is it appropriate for a patient to resume full activity after ocular surgery?
PITFALL
A new drug’s safety must be clearly proved before it becomes available, but no such requirements exist for new types of ocular surgeries or to reveal their potential for complications, which surgeons have a natural bias to underreport.
The true incidence of postsurgical trauma-related complications is thus difficult to determine. Injuries remain a largely neglected public health problem.5
THE MECHANISM OF EYE INJURIES
Expansion of the eyeball perpendicular to the direction of impact is the cause of many closed globe injuries (e.g., angle recession, iridodialysis, lens subluxation, choroidal rupture; see Chapters 17,20,21, and 23).
• The damage is more severe as the impact force increases and the time to maximum force decreases.
• Because the energy is transmitted throughout the globe, the tissue damage may occur distant from the impact site.
When the globe is penetrated/perforated/ruptured, the eyewall’s tensile strength is exceeded by a combination of local strain, shock waves, increased IOP, and acute cavitation of dissolved intraocular gas.
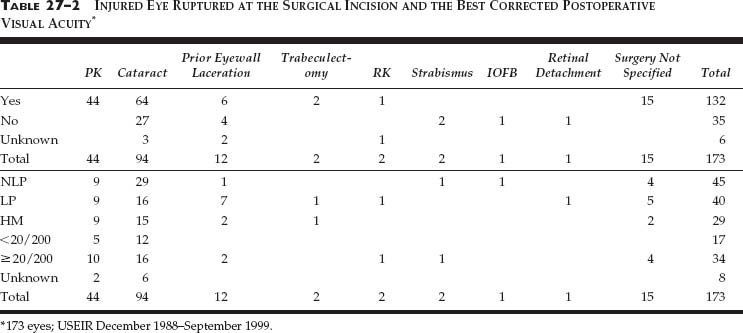
Because ruptures have the worst prognosis (see Chapter 3),6–9 the major concern is whether eyes sustain rupture, rather than contusion, because a prior surgery weakened the eyewall. Table 27–1 summarizes the energy various objects require to cause an open globe injury in the unoperated eye. Less energy is required to penetrate or rupture the eye with high-speed, small, hard missiles (BB) than with low-speed, softer, larger missiles (squash ball).
PEARL… The external factors that determine an eye’s injury include maximum force, time to maximum force, area of contact, and properties of the impacting object.
Theoretical Considerationsa
Energy transmitted to the eye via impact depends on the mass and velocity of the object.23 The entire spectrum of eye trauma can be produced by varying the impact force and the onset rate. For instance, when changing the speed of a 0.345 g BB:17
• at 13 m/s, the energy is less than the 0.03 J required to cause contusion;
• at 62.3 m/s, retinal tears occur at the vitreous base;
• at 72.0 m/s, the globe is penetrated;
• at 124 m/s, even bone is penetrated.16,17
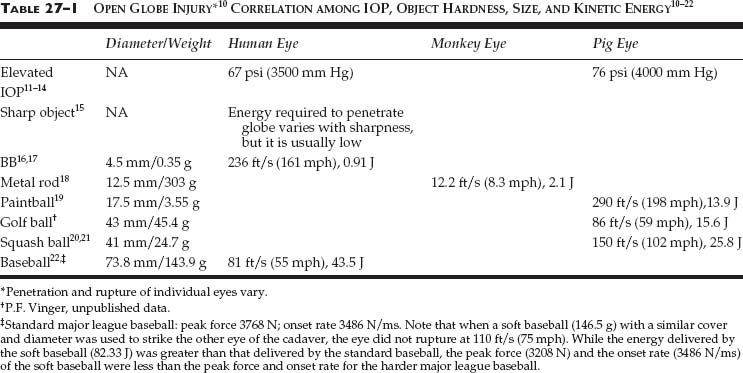
Test devices24 and mathematical models25 have been devised for documenting the eye injury potential of various products. The force onset rate needed to produce clinically detectable contusion is ~ 750 N/ms. Certain toy dart guns propelling suction cups exceed this level26 (see Fig. 27–1). Certain protective eyewears27 prevent/reduce injury by decreasing the force onset rate and the peak force by spreading the total force over time.
SPECIAL CONSIDERATION
Injury as related to force onset rate applies only to total forces in a limited range, which is yet undetermined. Even with an onset rate below 750 N/ms, the slowly applied force of a bulldozer would cause significant injury.
Structural Anatomy of the Eyewall
The eyewall is a union of two thin-walled (~0.5 mm) spheres (radii: 8 mm and 12 mm) with centers 5 mm apart.28 At the junction of the optic nerve sheath, which may be represented by a cylinder (radius: 2 mm), the scleral sphere is perforated by multiple openings (lamina cribrosa,29 Fig. 27–2). However, the eyewall is not of uniform thickness,30 is significantly thinner in myopia,31 and loses elasticity with age.32 The intact eyewall tends to rupture where its structural strength is weakest:
• at the limbus where the radius of curvature changes;
• near the equator behind exertion of the extraocular muscles where the sclera is thinnest; and
• at the lamina cribrosa where the sclera is perforated.33
How does a surgical incision influence the force necessary to open the eyewall?
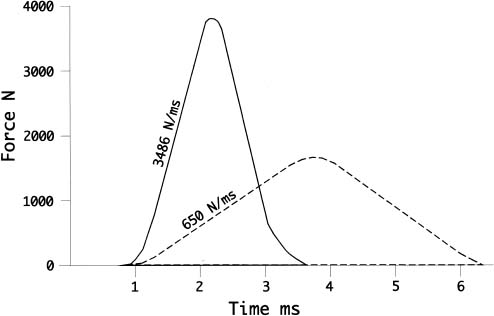
FIGURE 27–1 The same total force (area beneath the curves) with different onset rates and durations. (Solid curve) Major league baseball ruptures a human cadaver eye in an artificial orbit; peak force of 3768 N, onset rate of 3486 N/ms.22 (Dotted curve) Force spreads over time and has a peak onset rate below the 750 N/ms required to cause contusion.
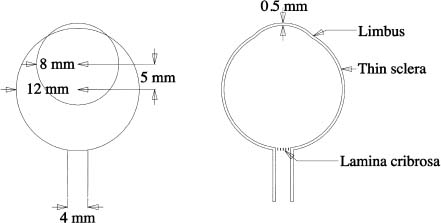
FIGURE 27–2 An unoperated eyewall ruptures at the limbus, equatorial sclera, and lamina cribrosa.
THE EFFECTS OF COMMON SURGICAL INCISIONS
PITFALL
The wound is most susceptible to rupture during the healing process. Full healing in the cornea requires 2 to 3 months, but the wound still develops only half of the original tensile strength.34,35 It would take an ideal glue for surgical incisions not to weaken the globe’s structural resistance.
When the healing process is complete but the wound is not as strong as the surrounding normal tissue, the stress concentration caused by the incisional notch must be considered.36 For example, the presence of an epithelial plug creates stress concentration at the RK incision site, a risk factor for rupture.
The required force is hard to predict and may depend on factors such as the size of the plug and the strength of the wound collagen.37
It is the combination of stress concentration and a diminished tensile strength that causes eyes to rup-ture at the site of surgical incision–provided the incision site has less tensile strength than the limbus, the equatorial sclera, or the lamina cribrosa (see Fig. 27–3).
PEARL… Not all incisions are prone to rupture; for example, even though a tapering 1-mm paracentesis incision has some weakening effect locally, this eye is still more likely to rupture at the limbus or equatorial sclera.
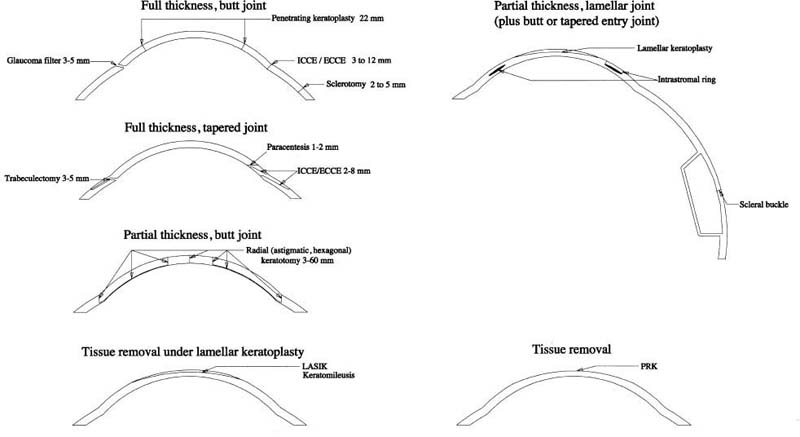
FIGURE 27–3 Common eyewall surgical incisions.
TRAUMA FOLLOWING DIFFERENT TYPES OF INTRAOCULAR SURGERY
Of 4798 eyes with open globe injury in the USEIR,38 3.6% of eyes were reported to have had prior surgery (Table 27–2).
PK
The incision length for a 7-mm PK graft is ~ 22 mm, prone to rupture due to trauma by a blunt object (Fig. 27–4). Of patients with prior PK:
• the lifetime risk of traumatic wound dehiscence (i.e., rupture) is 2.5 to 5.7%39–41;
• the average time of rupture is 3.4 years after PK;
• there is no time period after which the eye is “safe”: PK incisions have been reported to dehisce as long after the procedure as 13,42 25,43 and even 7538 years;
• the trauma may be trivialb;
• sutures do not help in retaining the graft42; and
• the prognosis is poor: only 28.6 to 33% of eyes recover ≥20/200 vision.40,49
The following information is from the USEIR on ruptured eyes with prior PK.
• The median age at the time of the injury is 45 years.
• The rupture may have occurred 75 years after PK.
• 59% of the patients are male.
• Falls and assaults with fist are the most common causes.
• Only 21% of eyes recovered final ≥20/200 vision.
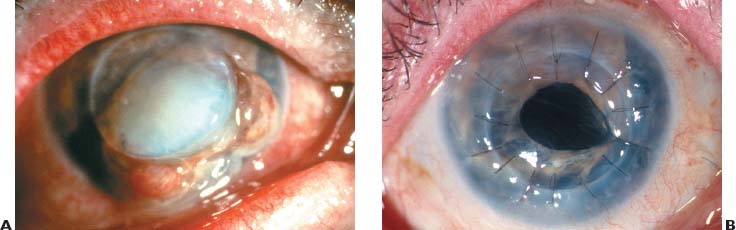
FIGURE 27–4 (A) Eye hit with blunt object 4 years after PK. Wound rupture with iris, lens, and vitreous prolapse. (B) Same eye after reconstruction. (Courtesy of Kathryn Colby, MD)
PEARL… Most basketball eye injuries are from body contact; trauma from the basketball is rare among eyes with no prior surgery.50
Cataract
PEARL… The tensile strength of healed limbal wounds remains less than that of the unincised scleral/corneal stroma (most new fibrils extend between and across, rather than into, the severed ends of existing collagen bundles); the surgical dehiscence of Descemet’s membrane generally remains unhealed in human eyes.51
• Rupture of ICCE and ECCE wounds (Fig. 27–5) often occurs long after surgery.
• The visual outcome is commonly poor.
• Frequent causes include falls and even minor trauma (e.g., a dog’s paw).52–55
• The lifetime risk of rupture is 1.4% with large-incision operations.56
• Phacoemulsification scleral pocket wounds 7.5 mm in length may also dehisce.57–58,c
• PC IOLs are more resistant to minor ocular traumad than AC or iris-fixated IOLs (see Chapter 21).55
• Improperly constructed small-incision clear corneal wounds may fail after even trivial trauma61; the length of the posterior lip is important62.
• Incisions with an internal corneal lip, which creates a self-sealing valve, provide a more pressure-resistant wound.65,66
• Manipulation of the entry wound during surgery may create a situation in which a longer incision is stronger than a shorter one.e
PEARL… The risk of wound dehis-cence is inversely correlated with incision length (Fig. 27–6).
CONTROVERSY
Clear corneal incisions 3.0 or 3.5 mm wide and at least 2.0 mm long have less tendency to rupture than shorter incisions and are comparable to similarly constructed scleral tunnel incisions.63 Conversely, square corneoscleral incisions with a 1.5-mm internal corneal lip have been found to offer greater stability and safety than the conventional rectangular clear corneal incision (3.2 × 2.0 mm).64

FIGURE 27–5 ICCE incision (no IOL implanted), rupturing 2 weeks postoperatively from a fall. Choroidal hemorrhage.

FIGURE 27–6 Fall causing a 4-mm phaco wound to rupture. (Courtesy of Roberto Pineda, MD)
PEARL… Self-sealing small sutureless cataract incisions, if properly constructed, provide a strong, pressure-resistant wound, which is unaffected even by scleral buckling.68
Analysis of the USEIR data shows that:
• 68% of eyes, rupturing after cataract surgery, do so at the surgical wound;
• the dehiscence may occur a long time after surgery:
 20% in 9 months to 15 years and only 16% in less than 5 weeks;
20% in 9 months to 15 years and only 16% in less than 5 weeks;
• the median age at the time of injury is 77 years;
• women slightly outnumber men (56% vs. 44%);
• the most common etiology is falling (54%);
• wearing eyeglasses does not appear to offer good protection;
• the IOL is extruded in 80% of eyes; and
• the prognosis is poor: less than 19% of eyes recover ≥20/200 vision.
Refractive Surgery
Incisional (radial, hexagonal, astigmatic) Keratotomy
This operation increases the susceptibility of the globe to rupture69,70 because of the following.
• The presence of epithelium in the wound.71–75
• The irregular scar tissue76 never regains the strength of the uncut corneal fibrils.77,f
• The total incision length is > 30 mm in an 8-incision and > 60 mm in a 16-incision RK.
• The incisions cut through 80 to 95% of the 0.5-mm corneal thickness.83,84
• The incisions often cut to or through the limbus.
SPECIAL CONSIDERATION
Standard RK incisions rupture at approximately half the impact force required to rupture unoperated eyes.78–81
PITFALL
RK and hexagonal keratotomy wounds not only require less energy (even the force of a clear corneal incision for cataract has been sufficient to dehisce an 8-month RK incision) than unoperated corneas to rupture but also remain susceptible for many years (Fig. 27–7).85–100,g The site of rupture also differs (see Table 27–3). Reducing the incision length appears to reduce the risk of corneal rupture, but as the IOP is increased, even eyes with “mini” RK eventually rupture.102.103