Fig. 14.1
Fulminant CMV retinitis
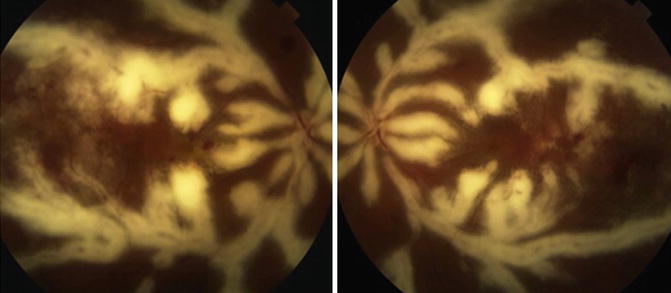
Fig. 14.2
Frosted branch angiitis due to perivascular CMV retinitis (Courtesy of Nicholas Jones)
This classification is somewhat abstruse as it is often seen when examining CMV retinitis patients in that they can harbor all these clinical forms concurrently.
Retinopathy lesion are generally plottes in one or more of three zones [26]. Zone 1 is the area within 1,500 mm of the optic nerve or 3,000 mm of the fovea. Zone 2 extends to the equator defined by ampullae vortex veins, and Zone 3 consists of the remaining anterior retina.
The median rate of progression for the retinal lesions towards the fovea without therapy is usually slow at around 24 μm/day. Those on anti-CMV treatment have a therapeutic benefit with a median progression rate of 11.5 μm/day [27]. Due to the apparently slow evolution of retinal lesions, serial photographs are much more sensitive than fundoscopy or fundus drawings for the detection of relapsing CMV retinitis [1].
14.4 Diagnosis
CMV retinitis is diagnosed on the basis of clinical examination that reveals typical ophthalmoscopic findings in immunocompromised patients. Seropositivity is of no big value as it can be detected in the majority of normal individuals. Nevertheless, documented rising CMV DNA blood levels appear to be associated with active CMV retinitis in individuals with low CD4+ T cell count [28]. In patients with active retinitis, there was a strong association between high tear levels of anti-CMV antibodies and active ocular infection [29]. PCR-based analysis of ocular fluids is of high sensitivity and specificity to aid in diagnosing critical cases to differentiate CMV from other causes of necrotizing retinitis like herpes viruses and toxoplasma retinochoroiditis in immunocompromised patients [30]. This is of utmost importance in patients who are not responsive to treatment, or in those with atypical lesions.
The differential diagnoses of CMV retinitis include those of cotton wool spots (CWS) in the early stage of the disease. In later disease, acute retinal necrosis (ARN) and progressive outer retinal necrosis (PORN) due to HSV or VZV, toxoplasma retinochoroiditis, syphilitic necrotizing retinitis, fungal infections, and intraocular lymphoma should be differentiated from CMV retinitis.
14.5 Treatment
Successful treatment of CMV retinitis requires both anti-CMV therapy and HAART. Therefore collaborating with the treating physician is a must in order to tailor the treatment plan as to get the most favorable response to anti-CMV therapy [31–33].
14.5.1 Ganciclovir
This is a virostatic antiviral agent that selectively inhibits CMV DNA polymerase. Due to its poor oral bioavailability, it is usually administered intravenously. Induction dose is 5–7.5 mg/kg twice daily for 2–4 weeks followed by 5 mg/kg/day for 5 days per week as a maintenance dose. Intravitreal route is an alternative means of delivery. Intravitreal injections are given at a dose of 200–2,000 mg/0.1 ml twice a week for 2–4 weeks as an induction dose. This is followed by a weekly injection as maintenance. The intravitreal implants – a polymer-based depot – provide a higher effective concentration at the site of action probably due to slow constant release of ganciclovir for up to 8 months and are exchangeable if empty or if infection recurs [34].
Intravitreal ganciclovir may be effective in cases of previously failed intravenous therapy to avoid serious systemic disadvantages and toxicity especially bone marrow suppression [35].
14.5.2 Foscarnet
Foscarnet is a virostatic agent that inhibits CMV DNA polymerase. Due to its antiretroviral activity however, it results in decreased mortality when compared to ganciclovir [10]. Nevertheless, it is less tolerated by patients and highly nephrotoxic, but renal functions can revert to normal upon drug cessation [39].
Induction dose is 90 mg/kg intravenously twice a day for 2–3 weeks followed by 90–129 mg/kg once daily for maintenance. Intravitreal injections as an alternative can be given at a dose of 2.4 mg/0.1 ml twice a week for 2–3 weeks followed by maintenance injection once a week.
14.5.3 Cidofovir
This drug suppresses viral replication by selectively inhibiting CMV DNA polymerase. Due to its toxic effects, it is administered along with probenecid and intravenous hydration. It may also cause severe anterior uveitis and inflammation leading to hypotony [42].
Induction dose is 5 mg/kg intravenous infusion given once weekly for 2 weeks, then every 2 weeks as a maintenance dose. Intravireal injections can be used to avoid systemic toxicity at a dose of 15–20 microgram (µg) every 6 weeks [43].
14.5.4 Fomivirsen
Fomivirsen binds the complementary sequence of mRNA and thus inhibits CMV replication [44]. It is only available as an intravitreal injection at a dose of 330 µg/week for 2 weeks as an induction regimen followed by the same dose every 4 weeks for maintenance. Side effects include anterior uveitis, vitritis, high intraocular pressure, retinal pigment epitheliopathy, and an increased risk of retinal detachment [45, 46].
Regardless of the antiviral agent, both intravitreal implants and injections are relatively safe in comparison to intravenous antiviral therapy. A recent study has shown that intravenous anti-CMV therapy seems to provide more benefits in terms of longer survival and decreased CMV dissemination. In addition, intraocular therapy had greater rates of retinitis progression and greater visual field loss. Hematologic and renal side effects were similar between systemic and intraocular anti-CMV therapy [47].
14.6 Complications
Rhegmatogenous retinal detachment is a serious complication of CMV retinitis occurring in 11–35 % of eyes [48, 49]. Such complication occurs due to necrotic breaks at the junction of healed retinitis and normal retina [50]. These breaks are usually multiple, irregular, and anterior in location which makes it difficult to visualize and increase the risk for retinal detachment [51].
The treatment of choice for rhegmatogenous retinal detachments associated with CMV retinitis is pars plana vitrectomy with silicone oil tamponade [52]. Relatively low redetachment rates have been shown after silicone oil removal [50, 53]. Prophylactic argon laser has been shown to reduce the risk of subsequent retinal detachments in patients treated medically for CMV retinitis [54].
Another recently described complication is immune reactivity uveitis (IRU). First described by Zegans and Karavellas [55, 56], this severe vitreous and anterior chamber inflammation is believed to occur in AIDS or immunocompromised patients with CMV retinitis who recover their immunity with HAART therapy. The postulated mechanism of IRU is believed to be due to immune reaction against CMV antigens [57–59]. Patients with IRU complain of blurred, decreased, or foggy vision and floaters. IRU can cause complications such as epiretinal membranes, cystoid macular edema, or vitreomacular traction [55, 60, 61]. The most common effective treatment for IRU is corticosteroids [62, 63]. Although continuing anti-CMV agents after immune reconstitution is not protective, it has been shown that aggressive anti-CMV administration before and early after starting HAART reduces incidence of IRU [55, 58, 60].
14.7 Prognosis
Although HAART has improved outcomes in CMV retinitis as compared to the pre-HAART era, a recent long-term study showed that AIDS patients with CMV retinitis are still at a high risk for mortality, retinitis progression, complications of the retinitis, and visual loss over a 5-year period [64]. Nevertheless, stopping anti-CMV agents after immune reconstitution did not increase possibility of poor outcome [15, 65].
14.8 Prevention
Before the advent of HAART, recommendations for ophthalmic screening in AIDS patients to rule out CMV retinitis were based on the CD4+ T cell count: yearly screens in patients with a CD4+ T cell count of >100 cells/ml, biannually for those with a CD4+ T cell count ranging from 50 to 100 cells/ml, and every 3 months for those with <50 cells/ml [1, 18, 31]. Those at high risk can receive oral ganciclovir 1,000 mg three times daily and valaciclovir 2,000 mg four times a day as it will significantly reduce the risk of developing CMV disease, including CMV retinitis [66, 67]. This prophylaxis is not used in HIV-infected individuals who achieve immune reconstitution with HAART. Furthermore, patients with previous CMV retinitis should be examined regularly after immune reconstitution [68].
Compliance with Ethical Requirements Conflict of Interest The authors declare that they have no conflict of interest. Informed Consent No human studies were carried out by the authors for this article. Animal Studies No animal studies were carried out by the authors for this article.
References
1.
2.
3.
Ahmed SA, et al. The prevalence of human cytomegalovirus seropositivity among blood donors at the Unit of Blood Transfusion Medicine. Hospital Universiti Sains Malaysia. Southeast Asian J Trop Med Public Health. 2006;37:294–6.PubMed
4.
5.
6.
7.
Pertel P, et al. Risk of developing cytomegalovirus retinitis in persons infected with the human immunodeficiency virus. J Acquir Immune Defic Syndr. 1992;5:1069–74.PubMed
8.
Sugar EA, et al. Incidence of cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Am J Ophthalmol. 2012;153:1016–24.e5.PubMedCentralPubMedCrossRef
9.
10.
Mortality in patients with the acquired immunodeficiency syndrome treated with either foscarnet or ganciclovir for cytomegalovirus retinitis. Studies of Ocular Complications of AIDS Research Group, in collaboration with the AIDS Clinical Trials Group. N Engl J Med 1992;326:213–20.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


