Etiologies of preseptal cellulitis
Infection of ocular adnexa: conjunctivitis, chalazia, hordeola, blepharitis, dacryocystitis, trauma with or without foreign body, insect bites, skin face wound, dacryoadenitis, impetigo
Hematogenous spread
Acute ethmoid or maxillary sinusitis
Etiologies of retroseptal cellulitis
Acute sinusitis
Trauma with or without foreign body
Progression of preseptal cellulitis
Hematogenous spread
Ophthalmic surgery: anterior segment surgery, eyelid surgery, strabismus surgery, peribulbar injection, orbital implants
Dental abscess
Otitis media
Endophthalmitis
Inhaled cocaine abuse
Diagnosis and characterization of orbital infection as preseptal infection or postseptal infection (orbital cellulitis) are primarily based on clinical findings, and imaging is very helpful in confirming the diagnosis and evaluating the extension of the infectious process. Early diagnosis and prompt, proper management of orbital infection is essential to prevent sight-threatening, as well as life-threatening, complications.
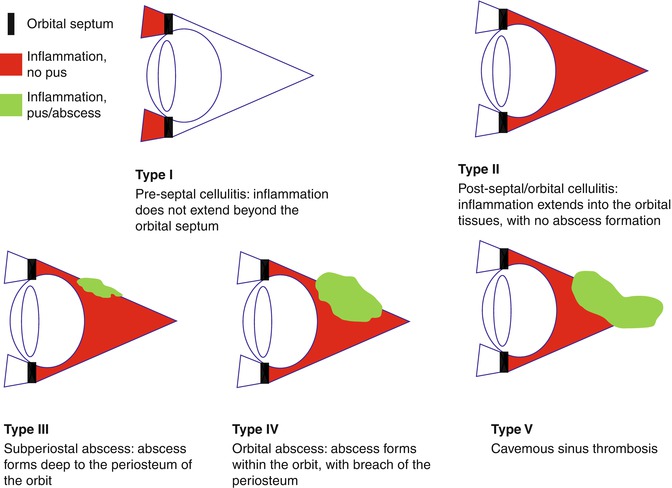
3.2 Pathophysiology
Orbital infections can develop by extension of infection from adjacent paranasal sinuses or upper respiratory infection, ocular and adnexal structures, direct inoculation as a result of trauma or surgery, or hematogenous spread in the setting of bacteremia [4–7]. The pathophysiology of orbital infection is related to local anatomical structures, especially the orbital septum and the lamina papyracea. According to a classification system proposed by Chandler in 1970 (Fig. 3.1), the orbital septum delineates orbital infections into preseptal (type 1) and retroseptal (type 2) cellulitis [5, 8]. The lamina papyracea, which is the medial orbital wall, is the thinnest bone separating the orbit from the sinuses and has numerous natural dehiscences as well as being perforated by numerous vessels and nerves [9]. This may explain why sinusitis and upper respiratory tract infection are the most common causes of orbital infection and why the ethmoid sinus is the most frequent orbital infection source [2, 10–12]. Natural defects on the lamina papyracea also facilitate communication between the ethmoid air cells and the subperiosteal space on the medial wall of the orbit leading to subperiosteal abscess (type 3 cellulitis). Moreover, the lack of lymphatic channels promotes the spread of infection from superficial tissues into the orbit. Orbital veins lack valves, so passage of infectious processes in both anterograde and retrograde directions is possible. Following progressive preseptal or orbital cellulitis, the inflammatory process may progress to abscess formation occurring inside or outside the muscle cone leading to an orbital abscess (type 4 cellulitis). Additionally, valveless orbital veins allow for the intracranial retrograde spread of infection to the cavernous sinus causing infectious cavernous sinus thrombosis (CST) (type 5 cellulitis). Sources of orbital infections other than paranasal sinusitis and upper respiratory infection include orbital trauma, with or without foreign body, dacryocystitis, ruptured dacryocele or dermoid cyst, dental infections, otitis media, endogenous endophthalmitis, ophthalmic surgery, eyelid lesions (chalazia, hordeola), insect bites, and impetigo (Table 3.1) [2, 10, 13–22]. Risk factors for orbital infection include diabetic ketoacidosis, history of HIV or immunosuppressive therapy, hematological malignancies, and renal transplant.
3.3 Symptoms and Signs
A patient with orbital infection usually presents with unilateral painful eyelid edema and erythema (Figs. 3.2 and 3.3). There may be a history of acute sinusitis or upper respiratory tract infection. Past medical history significant for HIV, diabetes, immunosuppression, steroid use, hematological malignancies, or renal disease is important to consider [23]. Early diagnosis and characterization of orbital cellulitis as preseptal or retroseptal infection are primarily based on clinical findings, and this is of utmost importance for prompt initiation of appropriate therapy to prevent ocular and systemic morbidity.
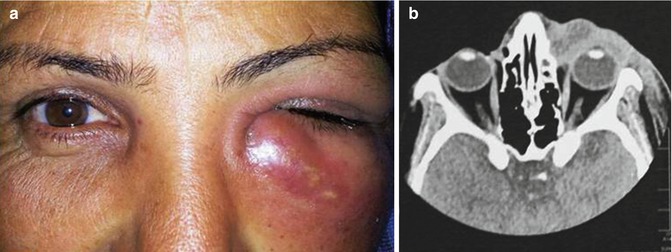
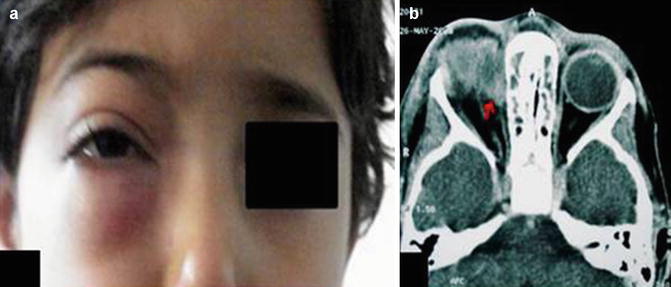
Fig. 3.2
(a) Photograph of a 38-year-old woman with 1-week history of acute dacryocystitis shows left inferior eyelid edema and erythema. (b) Axial CT scan shows left eyelid swelling and extent of preseptal inflammatory swelling in periorbital tissues consistent with preseptal cellulitis
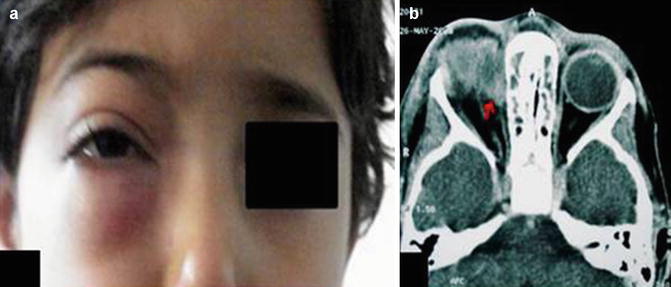
Fig. 3.3
(a) Photograph of an 8-year-old girl shows palpebral swelling with erythema and mild proptosis. (b) Axial CT scan shows subperiosteal abscess (type 3 orbital infection, red arrow) adjacent to the medial rectus and ethmoid sinusitis
Patients with preseptal cellulitis (type1) will present with preserved visual function, without proptosis, and full ocular motility without painful movement, as the extent of infection is superficial and does not extend posteriorly into the orbit (Table 3.2). Preseptal cellulitis may extend posteriorly, owing to the valveless communication of the facial and ophthalmic veins to the cavernous sinus, to cause one of the retroseptal infections (types 2–5) [24, 25]. Retroseptal septal infection (orbital cellulitis) is characterized by the presence of orbital signs including chemosis, proptosis, resistance to retropulsion of the eye, and extraocular muscle motility disturbance, with the potential for severe vision loss and life-threatening complications [13, 26, 27].
Table 3.2
Clinical signs of orbital infections
Type | Diagnosis | Clinical signs |
|---|---|---|
I | Periorbital (preseptal) cellulitis | Upper eyelid swelling causing ptosis without extraocular or visual changes |
II | Orbital (postseptal) cellulitis | Eyelid swelling, periorbital swelling, ptosis, proptosis, chemosis, limited or no impairment of extraocular movement |
III | Subperiosteal abscess | Displacement of the globe downward and laterally, impairment of extraocular movement with diplopia, decreased VA (later finding), RAPD |
IV | Orbital abscess | Severe proptosis, complete ophthalmoplegia, decreased VA that can progress to irreversible blindness, RAPD |
V | Cavernous sinus thrombosis | Orbital pain, chemosis, proptosis, sepsis, ophthalmoplegia. Can progress to the other eye |
Search for abnormal vital signs (e.g., tachycardia, hyperpyrexia) is recommended. However, normal temperature or vital signs should not rule out postseptal infection. Orbital cellulitis may or may not progress to a significant subperiosteal abscess (Fig. 3.3b), orbital abscess, or cavernous sinus thrombosis. When a fluctuant mass is palpable along the orbital rim with local tenderness, a subperiosteal abscess (type 3) should be considered. If a patient presents with decreased visual acuity, afferent pupillary defect, retinal venous dilatation, optic disk swelling, ptosis, severe directional proptosis, and ophthalmoplegia, an orbital abscess (type 4) should be suspected. Extension of orbital infection posteriorly into the cavernous sinus leads to cavernous sinus thrombosis (CST) (type 5). This serious complication is clinically characterized by headache, generalized sepsis, nausea, vomiting, high fever, periorbital edema, increasing proptosis, chemosis, afferent pupillary defect, and paralysis of eye movements. Infectious CST may cause meningitis with signs of meningeal irritation and loss of consciousness.
Orbital infections should be differentiated from nonspecific orbital inflammation, which usually presents with eyelid swelling/mass, less ocular pain than orbital infection, and no identifiable associated local or systemic causes. Other diseases that may mimic orbital infections include thyroid ophthalmopathy, which is typically bilateral and painless; orbital myositis, which may produce mild vascular congestion and proptosis; rhabdomyosarcoma; and metastatic orbital tumor, especially from breast carcinoma. Magnetic resonance imaging (MRI) may be helpful in the differential diagnosis of orbital infection.
3.4 Laboratory Tests and Imaging
Blood testing may show high white cell count, particularly in children with orbital cellulitis [29]. Blood cultures may be positive in children [30], but they are usually negative in adults [6, 10, 31]. Abscess and sinus aspiration remain invasive surgical procedures and should be performed only in case of clinical worsening despite a broad-spectrum antibiotic therapy. Surgical specimens are more likely than swabbing nasal mucosa or conjunctiva to provide positive results [6, 10, 30–32].
Orbital infections have been associated with a wide range of organisms. Staphylococcus, followed by Streptococcus species, are the most common pathogens, particularly in pediatric population, and methicillin-resistant S. aureus accounts for more than 70 % of S. aureus isolates [12, 32–34]. The incidence of Haemophilus influenza has declined due to the wide use and introduction of Haemophilus influenza type B vaccine [35]. Polymicrobial infections with aerobic and anaerobic bacteria are more common in patients aged 16 years or older [12, 32, 36]. Escherichia coli, Enterobacter species, Actinobacter species, and Proteus mirabilis can rarely be responsible for orbital infection secondary to hematogenous spread, especially in elderly or immunocompromised patients [10, 16, 37]. Fungal infection (mucormycosis or Aspergillosis species) usually occurs in association with diabetic ketoacidosis or immunosuppression, leading to a high mortality rate [38].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree