Although Cairns intention was to avoid “unnecessary and a nonphysiologic bypass” of the collector channels by excising a portion of the trabecular meshwork and adjusted Schlemm’s canal, we know today that the mechanism responsible for lowering intraocular pressure (IOP) after guarded filtration procedure is a through-and-through fistula, through the scleral flap borders, connecting the anterior chamber with the subconjunctival space.
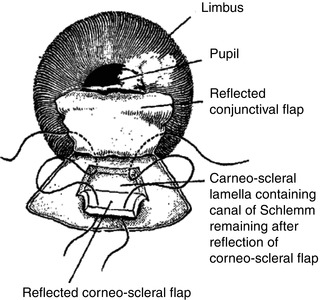
Possible alternative routes of filtration after trabeculectomy surgery (Fig. 26.3) are through:
Since then, many surgical and wound-healing modifications were added to the procedure. In order to keep the fistula open and functional, these modifications mainly address the wound-healing process in order to minimize the fibroblast proliferation and secondary scar tissue formation.
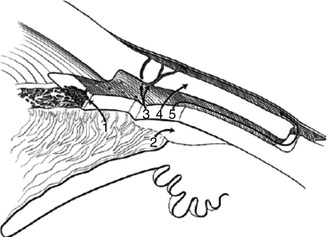
1.
The cut ends of Schlemm’s canal
2.
Suprachoroidal space
3.
Scleral vessels
4.
Thin scleral flap
5.
The scleral flap borders
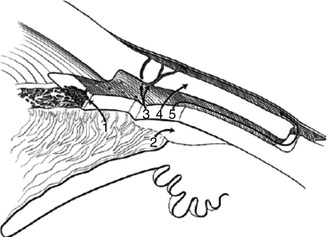
Fig. 26.3
Possible alternative routes of filtration after trabeculectomy surgery
At this point, it is necessary to define that all the trabeculectomy modifications still use a common concept to lower the IOP by creation of a fistula between the anterior chamber of the eye and the sub-Tenon and subconjunctival space. The aqueous humor is diverted by this fistula from the anterior chamber outside of the eye into the Sub-Tenon and subconjunctival spaces and finally collected into the episcleral and conjunctival veins.
In order to guide the reader systematically through the trabeculectomy procedure and all controversial aspects of this procedure (see Sidebar 26.1 ), we will explain the procedure step by step, in chronological order.
Anesthesia
General anesthesia is reserved for noncooperative patients.
Topical anesthesia with eye drops – Localin (oxybuprocaine hydrochloride 0.4 %), tetracaine/amethocaine (2-(dimethylamino) ethyl p-(butylamino) benzoate monohydrochloride 0.5 %), lidocaine 2 % (lignocaine hydrochloride 2 %), and jelly (Xylocaine – lidocaine 2 %) – should be preferred in most cases. When compared to peribulbar or retrobulbar anesthesia, there was no difference regarding pain control or surgical complication [3, 4]. Another option is to inject nonpreserved lidocaine 1 % into the anterior chamber.
In addition to the anesthetic effect, intracameral lidocaine dilates the pupil. Although there is an advantage in combined surgery (cataract extraction combined with trabeculectomy), this effect is unwanted in trabeculectomy alone.
The main disadvantage of the topical anesthesia is the lack of akinesia, which can be achieved with retrobulbar injections, or partial akinesia with peribulbar or sub-Tenon injections. Subconjunctival injection at the bleb site is to be avoided because it delivers poorer surgical outcomes [5].
For retrobulbar or peribulbar injections, a mixture of 50 % lidocaine and 50 % bupivacaine 0.75 % is used in order to prolong the anesthetic effect up to 6 h from 15 to 30 min with lidocaine only. It is recommended not to inject more than 5 ml of anesthetic volume around or behind the globe in order to avoid a “positive” pressure on the globe, which may add to the ischemic damage of the already-compromised optic nerve. Complications of injections are globe perforation, optic nerve damage, and peribulbar or retrobulbar hemorrhage.
Sidebar 26.1. Incisional Glaucoma Surgery: Making the Decision to Operate
(2)
C.U. Richter, MD Department of Ophthalmology, Harvard Medical School, Boston, MA, USA
Glaucoma is a group of diseases with patients who present with varying degrees of optic nerve damage and visual field loss as well as individually varied general medical, ophthalmic, and social issues. All of these factors combine to make the risk/benefit ratio and the decision to do glaucoma surgery different for each patient. Incisional glaucoma surgery, whether by filtering surgery, aqueous tube shunt, or nonpenetrating procedures, lowers intraocular pressure (IOP) by providing an alternative path for aqueous humor outflow and often stops or limits progression of the disease. The decision to perform incisional glaucoma surgery is based upon knowledge of the natural history of glaucoma progression correlated with a particular patient’s history and status, the patient’s response to medical and laser therapy, the benefits of surgery, and contraindications to and risks of surgery.
Patients with advanced glaucoma who have not reached a targeted low IOP are appropriately managed surgically in order to reach the clinically indicated low target IOP. Incisional glaucoma surgery is typically recommended only when medical and laser therapies have failed to prevent optic nerve damage or visual field loss or lower IOP to a level that will prevent such loss. Initial glaucoma surgery without prior medical or laser therapy is rarely appropriate or performed in the USA but may be for a patient presenting with advanced glaucoma damage and high IOP for whom urgent IOP control is the best hope to salvage vision. Most patients are tried on multiple topical antiglaucomatous medications, often in combination, including a prostaglandin analog, a beta-adrenergic blocker, an alpha agonist, and a topical carbonic anhydrase inhibitor. Pilocarpine, phospholine iodide, and oral carbonic anhydrase inhibitors may be tried, but their side effects frequently preclude long-term use. All the topical antiglaucomatous medications may cause side effects that limit their use: allergic reactions, precipitation of asthma, keratitis, and decreased vision, for example. Some patients may experience annoying side effects such as increased skin pigmentation, hyperemia, and ocular irritation. Should these patients have glaucoma surgery to relieve their symptoms? That question can be answered only after an extensive discussion of the possible benefits and complications of surgery. The complex medication schedule and the cost of chronic medical therapy may prevent a patient’s persistence with an otherwise successful medication plan. If these barriers to chronic successful management of glaucoma cannot be overcome, glaucoma surgery may be necessary to provide long-term control of the disease.
Patient’s Response to Medical and Laser Therapy, the Benefits of Surgery, and Contraindications to and Risks of Surgery
Glaucoma is frequently a slowly progressive illness with a long disease period before optic nerve damage and visual loss are detectable. However, once glaucoma damage is present, progression of damage may occur at lower IOPs and more rapidly than earlier in the disease course. Glaucoma progression may occur more rapidly with greater IOP elevation above the targeted pressure. Additionally, the greater the degree of glaucoma damage, the lower is the pressure required to minimize future vision loss. Patients with advanced glaucoma may require IOPs approximating 12 mmHg to minimize the risk of further glaucomatous damage, a level difficult to reach and maintain with only medical and laser therapy. Conversely, patients with little glaucomatous damage and few risk factors may tolerate higher pressures.
Laser trabeculoplasty (LTP) often lowers IOP for a number of years, reportedly as often as 75 % after initial laser treatment, and is indicated prior to incisional glaucoma surgery in those patients with a type of glaucoma that may respond. LTP may be performed prior to initiating topical glaucoma medications or after a trial of one to several medications. There is currently no consensus as to the best time in the disease course for laser intervention, with some ophthalmologists using it as first-line therapy. The efficacy of LTP in controlling glaucoma fades with time, and 30–50 % of eyes require additional surgical therapy within 5 years of treatment. Additional sessions of LTP are less successful than initial therapy. However, even considering the limitations of this procedure, LTP does lower IOP for an extended time in many patients with fewer complications than incisional surgery and should be considered prior to incisional surgery. However, LTP is not indicated prior to incisional glaucoma surgery in those patients with advanced glaucoma and high IOP because it is not always successful, takes time to be effective, and may cause IOP elevations – these patients require urgent glaucoma control to prevent progression.
Incisional glaucoma surgery is successful in 70–80 % of patients in reducing IOP and preserving vision. It also frequently eliminates or reduces the need for antiglaucomatous medications, reducing ocular side effects, compliance problems, and the ongoing cost of disease management for the patient. However, glaucoma surgery may fail 20–30 % of the time and carries risks of significant complications. Therefore, the recommendation for surgery should include an extensive discussion with the patient of the proposed procedure, the postoperative management necessary to maximize success, and the potential complications.
For most patients with uncontrolled IOP or progressive optic nerve damage and visual field loss, surgery will be the correct decision. Some patients with compliance difficulties or medication side effects will choose to improve their compliance or endure side effects and therefore delay or avoid surgery. The physician and patient must carefully weigh the risks of vision loss in the patient’s lifetime without surgery, which is often difficult and always imprecise. If a patient appears to have a life-threatening disease or a limited life expectancy, consultation with the patient’s other physicians may be helpful in the decision-making process.
In summary, incisional glaucoma surgery is usually required when the IOP in uncontrolled or optic nerve cupping is progressing or visual field loss is progressing despite a comprehensive medication trial and LTP. The greater the degree of glaucoma damage and the more elevated the IOP, the more urgent the surgery. While frequently successful, glaucoma surgery may also have vision-threatening complications, both in the early postoperative period and later, and requires careful counseling of the prospective surgical patient of the potential risks as well as benefits and the postoperative care necessary.
Bibliography
Ederer F, Gaasterland DA, Dally LG, Kim J, VanVeldhuisen PC, Blackwell B, Prum B, Shafranov G, Allen RC, Beck A, AGIS Investigators. The advanced glaucoma intervention study (AGIS):13. Comparison of treatment outcomes within race: 10-year results. Ophthalmology. 2004;111:651–64.
Migdal C, Gregory W, Hitchings R. Long-term functional outcome after early surgery compare with laser and medicine in open-angle glaucoma. Ophthalmology. 1994;101:1651–6.
Richter CU, Shingleton BJ, Bellows AR, et al. Retreatment with argon laser trabeculoplasty. Ophthalmology. 1987;94:1085–9.
Shingleton BJ, Richter CU, Dharma SK, et al. Long-term efficacy of argon laser trabeculoplasty. A 10-year follow-up study. Ophthalmology. 1993;100:1324–9.
Spaeth GL, Baez KA. Argon laser trabeculoplasty controls one third of cases of progressive, uncontrolled, open angle glaucoma for 5 years. Arch Ophthalmol. 1992;110:491–4.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130:429–40.
The Glaucoma Laser Trial (GLT) and Glaucoma Laser Trial follow-up study: 7. Results. Glaucoma Laser Trial Research Group. Am J Ophthalmol. 1995;120:718–731.
Weber PA, Burton GD, Epitropoulos AT. Laser trabeculoplasty retreatment. Ophthalmic Surg. 1989;20:702–6.
Eye Exposure
A good exposure of the surgical field is mandatory and is achieved with a lid speculum, which opens the eye, preferably without creating pressure on the globe.
It is important not to drag the conjunctiva with the speculum arms because this may tighten the conjunctiva and create an unnecessary surgical difficulty.
Traction Suture
This step is useful since it helps to keep the eye in the desired inferior position throughout the surgery. The suture can be placed in clear cornea or underneath the superior rectus muscle. For the clear corneal traction suture, a 7/0 spatulated Vicryl or silk corneal traction suture is placed half thickness and 2 mm anterior to the limbus. The eye is rotated inferiorly, and the suture is affixed to the drape inferior to the eye (Fig. 26.4a–c).
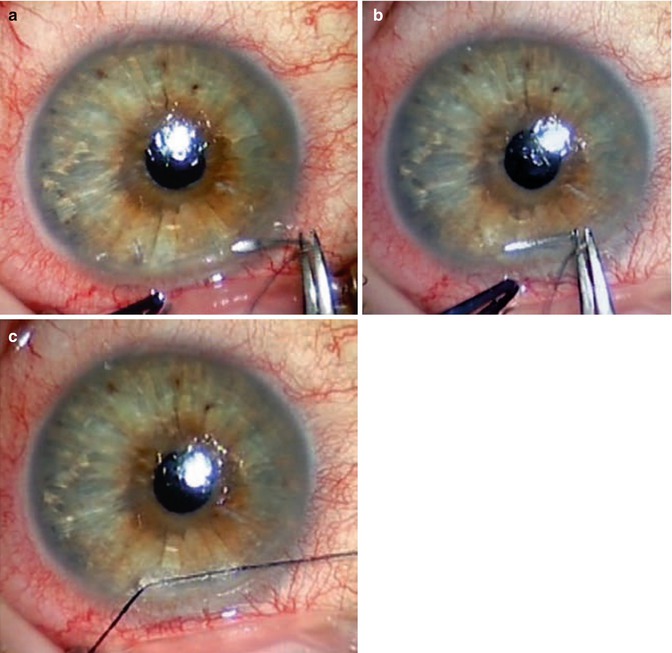
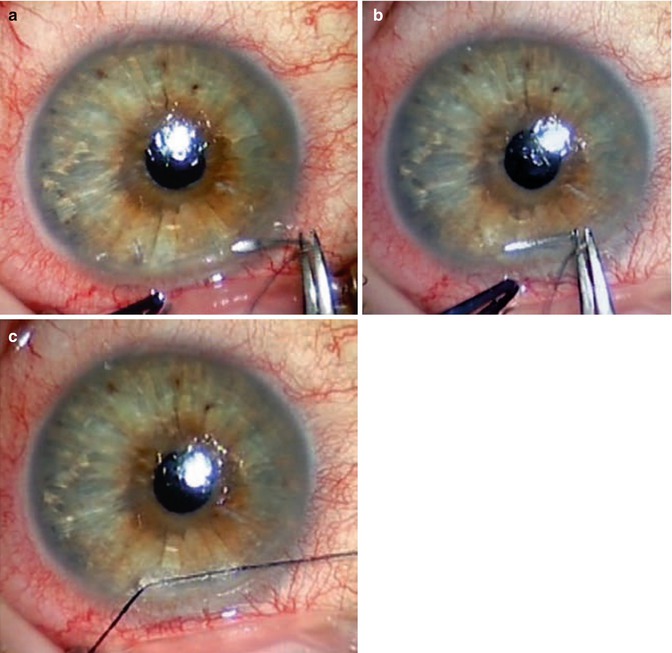
Fig. 26.4
Clear corneal traction suture. (a, b) A corneal traction suture is placed half thickness and 2 mm anterior to the limbus. (c) The eye is rotated inferiorly, and the suture is affixed to the drape inferior to the eye
In the superior rectus muscle traction suture technique, a 4/0 silk suture is passed approximately 12 mm behind the superior limbus, underneath the superior rectus muscle, and attached to the drape over the patient’s forehead.
The clear corneal traction suture is preferred because it provides better exposure (more firmly attached), no risk for subconjunctival hemorrhage or conjunctival damage, no risk of postoperative proptosis due to the superior rectus damage, and has been found to provide a better surgical outcome by the UK National Survey of Trabeculectomy [6].
Sidebar 26.2. Anticoagulants and Glaucoma Surgery
(3)
S.S.R. Iyer, MDDepartment of Ophthalmology, University of Tennessee Health Science Center, Memphis, TN, USA
(4)
S. Salim, MD, FACSHamilton Eye Institute, University of Tennessee, 930 Madison Avenue #470, Memphis, TN 38163, USA
(5)
Department of Ophthalmology, University of Virginia School of Medicine, 800715, Charlottesville, VA 22908-0715, USA
Many patients requiring glaucoma surgery are concomitantly receiving anticoagulation therapy for other comorbidities, including arrhythmia, cardiac prosthetic valve, or thromboembolic disease resulting from various etiologies. The alternative of complete discontinuation of anticoagulation therapy before surgical intervention has raised concerns about the risk of serious thromboembolic events in the perioperative period in these patients. Glaucoma surgeons are usually concerned about hemorrhagic complications of anticoagulation that can ultimately affect surgical success.
Anticoagulation therapy is commonly categorized in two groups: those undergoing therapy with warfarin and those undergoing therapy with an antiplatelet agent (clopidogrel and aspirin [acetylsalicylic acid]). The common intraoperative and postoperative surgical complications associated with blood thinning medications include retrobulbar hemorrhage, hyphema, vitreous hemorrhage, and suprachoroidal hemorrhage.
A few retrospective studies have analyzed hemorrhagic complications of glaucoma surgery in patients using anticoagulation therapy.1,2 Law and colleagues reported a higher incidence of complications following glaucoma surgery in patients who were on either warfarin or antiplatelet therapy compared to controls, with the highest rate of complication noted in patients who continued warfarin therapy through surgery. In this study, there were less hemorrhagic complications in patients who discontinued coumadin compared with those who continued anticoagulation; however, the difference failed to reach statistical significance. Similarly, in a retrospective examination of 367 trabeculectomies, Cobb et al. observed that continuation of either warfarin or aspirin therapy in those undergoing surgery had approximately twice the risk of hyphema. However, the use of aspirin did not adversely affect the eventual surgical outcomes, whereas warfarin’s use ultimately resulted in poor surgical outcomes and intraocular pressure (IOP) control.
Alwitry and colleagues reported that most glaucoma surgeons in the UK do not routinely stop anticoagulation therapy prior to glaucoma surgery. A smaller percentage of these surgeons chose to discontinue long-term anticoagulation therapy and initiate heparin therapy. Bleeding complications secondary to anticoagulation therapy are not limited to the glaucoma surgical patient, as there have been concerns among surgeons in other subspecialties including vitreoretinal surgery and oculoplastic surgery. However, a unique aspect of glaucoma surgery is the risk of hypotony and hypotony-related complications, including suprachoroidal hemorrhage, during the early postoperative period. In high-risk eyes, glaucoma surgeons may choose to discontinue anticoagulation during the perioperative period or use other techniques to reduce the risks of hemorrhagic complications during and after surgery.
When surgeons choose to discontinue anticoagulant therapy, the approaches vary and can be individualized to each patient. In patients treated with warfarin, the drug can be discontinued for a minimum of 3 days prior to surgery to improve coagulation intraoperatively and postoperatively. The patient’s primary care practitioner may allow withholding warfarin for an additional several days after surgery, which may avoid postoperative complications in high-risk eyes. It is worth noting that warfarin cessation may lead to a rise in clotting factors that put the patient in a hypercoagulable state, shown to peak at one week afterwards [5, 8]. Because aspirin has a prolonged anti-platelet aggregation effect, some surgeons recommend cessation of aspirin therapy one or two weeks prior to surgery, with approval by the patient’s primary care provider. Discontinuation of aspirin on the day of surgery probably has little or no influence on the antiplatelet effect of the drug during the perioperative and immediate post-operative period.
There are risks associated with discontinuation of long-term anticoagulation therapy in patients undergoing surgery. The risk of thromboembolic events is probably low (less than 1 %). However, some of these problems such as pulmonary embolus or stroke can be life-threatening. In each patient, the ocular risk of continuation of anticoagulant therapy should be weighed against the systemic risk of life-threatening hemorrhagic complications. Communication and coordination with the physician who is managing the long-term anticoagulant therapy is strongly recommended, along with a frank discussion with the patient of the risks and benefits of altering anticoagulation therapy in the perioperative period.
Alternatives to discontinuation of anticoagulation therapy may be tried in order to reduce the risk of bleeding complications. Modifying anesthetic methods may be helpful, including use of topical and local anesthesia in order to minimize the risk of retrobulbar hemorrhage associated with retrobulbar injection of anesthetic. Surgical techniques, also, may be modified to avoid hemorrhagic complications. Meticulous use of hemostasis during flap dissection, anterior placement of sclerotomy to avoid the ciliary body, and omitting surgical iridectomy have been shown to avoid bleeding. Tightly securing the scleral flap to prevent bleeding and postoperative hypotony has been advocated. Postoperative hypotony increases the risk of bleeding complications, specifically suprachoroidal hemorrhage. In glaucoma drainage implant surgery, use of suture ligatures around the tube or two-stage surgery can reduce the rate of postoperative hypotony. Intraoperative and postoperative use of viscoelastics may avoid or mitigate problems associated with hypotony. Gradual reduction of the IOP during surgery may avoid dramatic fluctuations in IOP, which increase the risk of bleeding complications.
In summary, the current literature suggests that patients receiving anticoagulation therapy with warfarin and/or antiplatelet agents who are candidates for glaucoma surgery are at increased risk for serious hemorrhagic complications. Many glaucoma subspecialists continue anticoagulation through surgery, although surgeons may modify their anesthetic and surgical techniques to minimize complications. In patients at high risk for ocular hemorrhagic complications, the surgeon may recommend withholding anticoagulant therapy during the perioperative period. In all instances, ophthalmologists should collaborate with the patient’s physician and other medical specialists in assessing the patient’s risk of hemorrhagic ocular complications, the systemic risk of discontinuing anticoagulant therapy, and the perioperative plan for use of anticoagulant drugs.
Bibliography
Alwitry A, King AJ, Vernon SA. Anticoagulation in glaucoma surgery. Graefes Arch Clin Exp Ophthalmol. 2008;246(6):891–6.
Baudo F, de Cataldo F, Mostarda G, et al. Management of patients on long-term oral anticoagulant therapy undergoing elective surgery: survey of the clinical practice in the Italian anticoagulation clinics. Intern Emerg Med. 2007;2:280–4.
Cobb CJ, Chakrabarti S, Chadha V, Sanders R. The effect of aspirin and warfarin therapy in trabeculectomy. Eye. 2007;21(5):598–603.
Grip L, Blomback M, Schulman S. Hypercoagulable state and thromboembolism following warfarin withdrawal in post-myocardial infarction patients. Eur Heart J. 1991;12(11):1225–33.
Jampel H. Glaucoma surgery in the patient undergoing anticoagulation. J Glaucoma. 1998;7(4):278–81.
Jeganathan VS, Ghosh S, Ruddle JB, Gupta V, Coote MA, Crowston JG. Risk factors for delayed suprachoroidal hemorrhage following glaucoma surgery. Br J Ophthalmol. 2008;92(10):1393–6.
Konstas AGP, Jay JL. Modification of trabeculectomy to avoid postoperative hyphema. The ‘guarded anterior fistula’ operation. Br J Ophthalmol. 1992;76:353–7.
Law SK, Song BJ, Yu F, Kurbanyan K, Yang TA, Caprioli J. Hemorrhagic complications from glaucoma surgery in patients on anticoagulation therapy or antiplatelet therapy. Am J Ophthalmol. 2008;145(4):736–46.
McCormack P, Simcock PR, Tullo AB. Management of the anticoagulated patient for ophthalmic surgery. Eye. 1993;7:749–50.
Narendran N, Williamson TH. The effects of aspirin and warfarin therapy on haemorrhage in vitreoretinal surgery. Acta Ophthalmol Scand. 2003;81:38–40.
Parkin B, Manners R. Aspirin and warfarin therapy in oculoplastic surgery. Br J Ophthalmol. 2000;84:1426–7.
The Fluorouracil Filtering Surgery Study Group. Risk factors for suprachoroidal hemorrhage after filtering surgery. Am J Ophthalmol. 1992;113:501–7.
Tuli SS, WuDunn D, Ciulla TA, Cantor LB. Delayed suprachoroidal hemorrhage after glaucoma filtration procedures. Ophthalmology. 2001;108(10):1808–11.
Conjunctival Incision
The bleb surgical site is in the upper globe, preferably under the upper eyelid in order to reduce infections or bleb leakage [7]. It is advised to use a topical vasoconstrictive agent, like adrenaline 0.01 %. Efrin 10 % can also be used but provides less vasoconstriction. The vasoconstrictive agent is used before conjunctival dissection in order to minimize conjunctival bleeding. The conjunctival incision can be performed in a limbal-based or fornix-based fashion [8, 9]. In general, the limbal-based technique first described by Cairns was abandoned due to higher rate of postoperative complications (Table 26.1). The higher rates of complications are probably related to the differences in bleb morphology, with limbal-based flap cases more likely to develop cystic blebs [8].
Table 26.1
Postoperative complications of limbal-based versus fornix-based techniques
Complication | Limbal based (%) | Fornix based (%) |
|---|---|---|
Cystic bleb | 90 | 20 |
Blebitis | 20 | None |
Leakage | 24 | 65 |
Limbal-based bleb creation is more time consuming, has more risk of buttonhole formation, and allows poorer surgical exposure, which prevents diffuse antibiotic application. A large and diffuse antibiotic-treated area results in a postoperative diffuse posterior filtering bleb and an increase in bleb survival [8, 10].
One of the risks with fornix based opposed to limbal based may be a higher rate of early leakage, but this was not found to be a risk factor of bleb failure [11]. This leakage can be minimized with new surgical methods of tight suture techniques [12–14] (Fig. 26.5a–c).
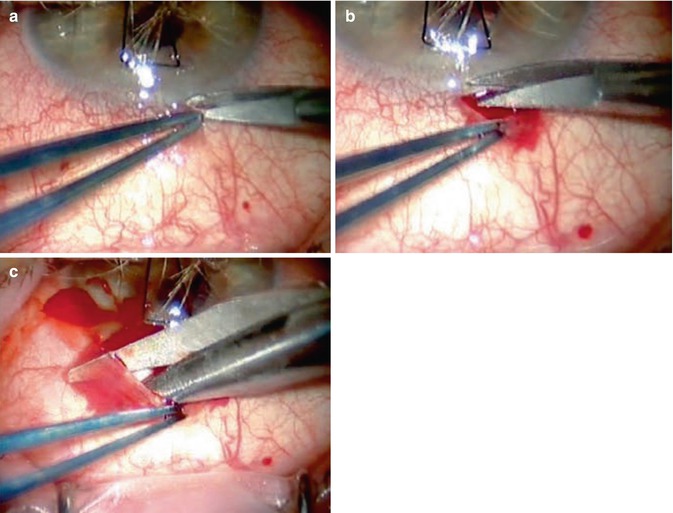
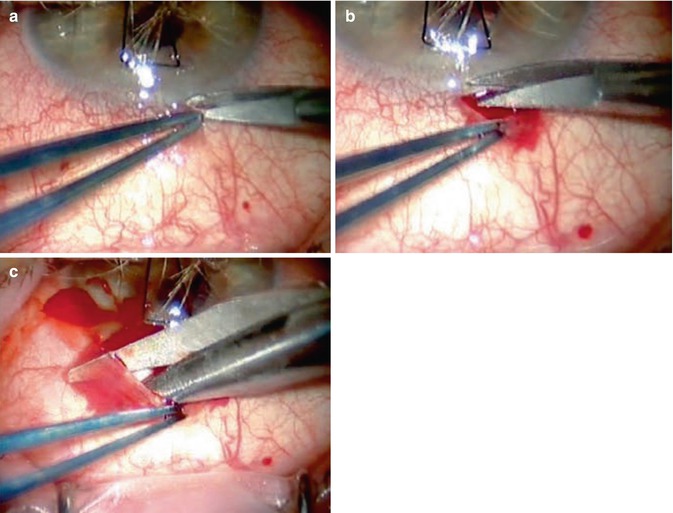
Fig. 26.5
Tight suture techniques. (a) The conjunctiva is grasped close to the limbus. (b) The conjunctiva is then lifted, and an initial small incision parallel to the limbus is made with Vannas or Westcott scissors. (c) The incision is extended parallel to the limbus
The conjunctiva is grasped close to the limbus at the selected superior nasal or temporal quadrant, with a nontraumatic fine forceps. Toothed forceps that can cut the conjunctiva should not be used. The conjunctiva is then lifted and an initial small incision parallel to the limbus is made with Vannas or Westcott scissors (preferable blunt-tipped instruments). The incision is extended parallel to the limbus up to two clock hours.
The 12 o’clock or superior nasal quadrant is preferred unless the conjunctiva is scarred from previous surgery. The first reason for selecting these positions is to reserve the nearby areas, mainly the temporal or superotemporal quadrant for subsequent cataract surgery. Another reason is that these sites provide lower IOPs at long-term follow-up compared to the superior or superotemporal positions [15].
The Tenon’s capsule can be separated together with the conjunctiva or in two steps. Performing a separate incision and separation of the Tenon’s capsule improves the ability to enter the sub-Tenon space. A blunt and, as much as possible, nontraumatic undermining of the Tenon is carried out with Westcott scissors, in order to minimize inflammatory mediator release and to reduce the postoperative scar formation [16]. The sub-Tenon’s space should be dissected at least 8 mm posterior from the limbus. Meticulous care must be made to prevent conjunctiva buttonhole formation, and it is advised to grasp just the Tenon layer as this may result in a buttonhole. An area of approximately 5.5-mm exposed sclera is desired.
Bleeding episcleral blood vessels should be gently diathermized, in order to minimize clot and fibrin formation and to reduce the postoperative inflammation. Wet-field cautery with or without the use of a Weck-cel sponge is the preferred technique (Fig. 26.6). Care must be taken not to cauterize the conjunctiva. Smaller-tipped cautery units are preferable. This can be achieved by pushing the conjunctiva away from the cautery tip with the Weck-cel sponge.
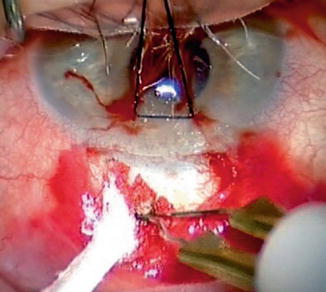
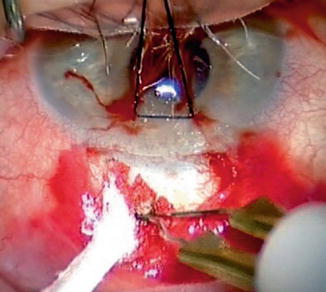
Fig. 26.6
Wet-field cautery
Cautery of deep scleral blood vessels is not necessary and may also just increase inflammatory mediators in the field. Excessive and loose episcleral tissue should be removed with a sharp blade to minimize postoperative scar tissue formation. Small incision trabeculectomy (SIT) [17] avoids Tenon dissection. A limbal parallel conjunctival incision of 2.5 mm is performed, and then a scleral pocket extending posteriorly is carried out, and the subconjunctival space is entered (see Sidebar 26.3). There are still not enough published reports of success rates or prevalence of cystic bleb or scar tissue development around these small blebs.
Sidebar 26.3. Fornix-Versus Limbal-Based Flaps
Kenneth B. Mitchell6
(6)
K.B. Mitchell, MD Department of Ophthalmology, West Virginia University School of Medicine, Morgantown, WV, USA
Surgeons become comfortable with either limbal- or fornix-based flaps and it becomes their “fastball.” That being said, it is useful to note the advantages and disadvantages of both incisions for trabeculectomy.
The Fornix-Based Flap
Advantages
The fornix-based incision can be quickly made (Fig. 26.7a–d). Conjunctiva and Tenon’s are fused at the limbus, and Tenon’s is thinnest anteriorly. There is much less manipulation of the conjunctiva and Tenon’s after the initial incision and dissection. Vessel transection is anterior where the vessel diameter is smallest. This relates to less bleeding, which may be controlled by application of brimonidine with or without light wet-field cautery. There is usually no need for dissecting Tenon’s from the limbal zone, and visualization is excellent. Closure may be quicker. The surgeon may be less in need of an experienced assistant.
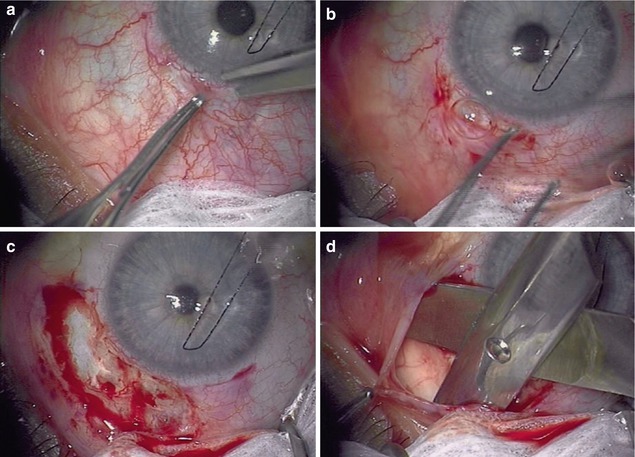
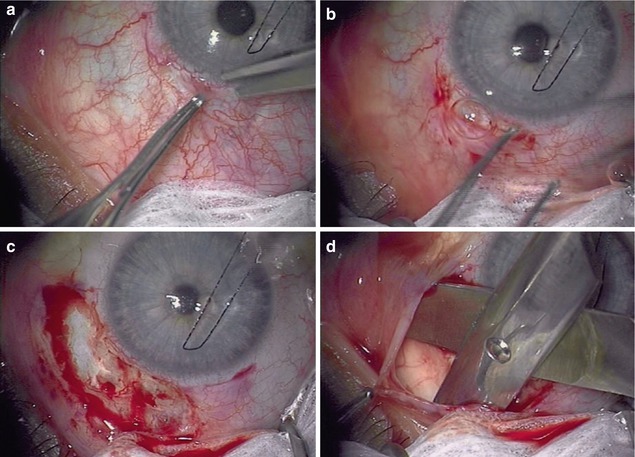
Fig. 26.7
Steps in creating a fornix-based flap. (a) Beginning the fornix-based flap with nontoothed forceps and scissors tenting the fused conjunctiva and Tenon’s up at the limbus. (b) Ending the curvilinear limbal incision. (c) Exposing the scleral bed. (d) Blunt dissection posteriorly for antimetabolite or tube shunt plate insertion
A fornix-based flap is easily combined with a single-site phaco-trabeculectomy.
Disadvantages
Any posterior hemorrhage from tissue plane dissection with scissors is more difficult to visualize and treat with fornix-based flaps.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree