Purpose
To ascertain the incidence of scleritis and episcleritis in a Hawaiian population and describe variations by age, sex, and race.
Design
Retrospective, population-based cohort study.
Methods
All electronic medical records for enrollees in Kaiser Permanente Hawaii (n = 217 061) from January 1, 2006 to December 31, 2007 were searched for International Classification of Diseases, 9th Edition (ICD-9) codes associated with ocular inflammation. Chart review was conducted to verify a clinical diagnosis of scleritis or episcleritis. Confirmed cases were used to calculate incidence rates per 100 000 person-years. Ninety-five percent confidence intervals (CI) were calculated for each incidence rate, including age-, sex-, and race-specific rates, using bias-corrected Poisson regression. To assess for confounding, a multivariate analysis adjusting for age, sex, and race was also performed.
Results
Of 217 061 eligible patients, 17 incident scleritis cases and 93 incident episcleritis cases were confirmed. The overall incidence rates of scleritis and episcleritis were 4.1 (95% CI: 2.6-6.6) and 21.7 (95% CI: 17.7-26.5) cases per 100 000 person-years, respectively. Women were overrepresented among scleritis patients ( P = .049). Pacific Islanders were the most underrepresented racial group among cases of scleritis and episcleritis ( P = .006, P = .001). Blacks had the highest incidence of scleritis ( P = .004).
Conclusions
These results provide a population-based estimate of the incidence of scleritis and episcleritis in a diverse population and highlight differences in patients’ demographic characteristics. Differences in incidence by sex and race raise questions about genetic and environmental influences on the development of these conditions.
Scleritis and episcleritis are ocular inflammatory diseases with different implications for visual outcomes and systemic disease risk. Episcleritis has been classically described as having a self-limited course and posing no threat to vision, whereas scleritis may result in ocular complications, be more commonly associated with systemic diseases and increased mortality, and require systemic immunosuppressive therapy. To date, studies of these diseases have been limited to retrospective case series from tertiary eye care centers, which are susceptible to referral bias. One study, published in 1974, found that patients with scleritis made up 0.08% of referrals to a hospital ophthalmology department. Two more recent studies, both from tertiary eye care centers, found that 2.6%-8.7% of referrals to ocular inflammatory disease specialists suffered from scleritis and 1.4% from episcleritis. Given the clinical importance of scleritis and episcleritis, the limitations of existing incidence data, and the absence of population-based reports, there is a need for a population-based study characterizing their epidemiology.
There are several advantages to considering Kaiser Permanente Hawaii as a source of data for a population-based study. Kaiser serves approximately 16% of Hawaii’s total population, with 18 clinics throughout the state. Furthermore, the population served is racially diverse and includes all age groups. Additionally, patient encounters are documented in a readily accessible electronic medical records system.
This epidemiologic study seeks to ascertain the incidence of scleritis and episcleritis among Kaiser Permanente Hawaii members and to describe demographic variations in incidence by age, sex, and race.
Methods
Institutional Review Board (IRB)/Ethics Committee approval was prospectively obtained at Kaiser Permanente Hawaii and the University of California, San Francisco for all aspects of this study involving retrospective review of patient data. All work was Health Insurance Portability and Accountability Act compliant. Patient encounters documented between January 1, 2006 and December 31, 2007 in the electronic medical records of Kaiser Permanente Hawaii enrollees (n = 217 061) were retrospectively queried using diagnosis codes from the International Classification of Diseases, 9th edition (ICD-9), listed in the Supplemental Table (available at AJO.com ), corresponding to ocular inflammatory conditions. Since the larger Pacific Ocular Inflammation Study is interested in the epidemiology of ocular inflammatory diseases, including uveitis, herpetic eye disease, scleritis, and episcleritis, the ICD-9 codes initially chosen were broad. Subsequently, a uveitis and cornea fellowship–trained ophthalmologist verified all patient diagnoses based on documented clinical exams. The main outcome measure of this study was a new clinical diagnosis of scleritis or episcleritis during the study period, and only confirmed cases were included in incidence calculations. Demographic data, including age, sex, and self-reported race, were collected and compared between incident cases and the general Kaiser Permanente Hawaii membership using Fisher exact test. Overall incidence rates and incidence rates across demographic groups were calculated.
Incidence rates were calculated per 100 000 person-years by dividing the confirmed incident cases by the total person-years of follow-up and multiplying by 100 000. Given the constant fluctuation in membership of the Kaiser Permanente Hawaii health system, we used quarterly population data to calculate the total number of person-years of follow-up. Incidence rates were reported for the overall study period (January 1, 2006-December 31, 2007) and also within each year to evaluate the consistency of the rates. We separately calculated population-based rates for scleritis and for episcleritis, and stratified them by age and sex. Age was stratified into the following groups: 0-14, 15-24, 25-44, 45-64, and 65+ years of age, based on patient age at the middle of the study period, January 1, 2007. When calculating age- and sex-specific incidence rates, the total number of person-years was adjusted to reflect quarterly membership data within each group. Since race data were available only for a portion of incident cases and Kaiser Permanente Hawaii members, incidence analyses by race reflect the demographics of the subset of patients who self-reported their race.
We calculated 95% confidence intervals (CI) for each incidence rate and compared age-, sex-, and race-specific incidence rates using bias-corrected Poisson regression. This method is designed to yield small positive incidence estimates even when zero counts are observed for a given number of person-years of observation. Univariate and multivariate analyses were conducted using age category, sex, and racial classification. Relative rates were estimated by using bias-corrected Poisson regression, with the logarithm of the number of person-years at risk as the offset. Approximate confidence intervals were constructed using the estimated standard errors. Likelihood ratio tests were used to assess the statistical significance of race. A P value less than .05 was considered statistically significant. STATA 11.0 (StataCorp, College Station, Texas, USA) and R statistical software (The R Foundation for Statistical Computing, Vienna, Austria) were used for performing all analyses.
Results
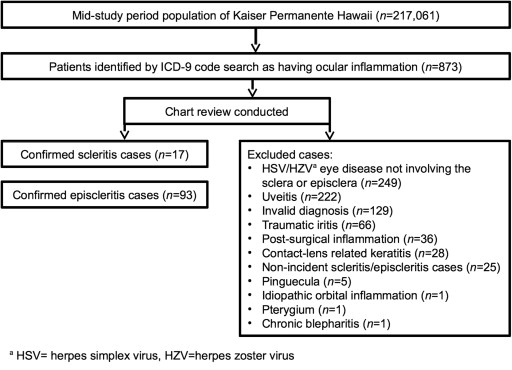
Kaiser Permanente Hawaii had a total mid–study period population of 217 061 people, which corresponds to a person-time estimate of 433 794.2 person-years for the study period. From this population, 873 patient records were identified on the basis of ICD-9 diagnosis code search ( Supplemental Table , available at AJO.com ). Based on individual review of these medical records, there were 17 confirmed scleritis cases and 93 confirmed episcleritis cases ( Figure ). Notable reasons for exclusion include diagnoses of herpes simplex virus/herpes zoster virus (HSV/HZV) eye disease not involving the sclera or episclera, uveitis, invalid diagnoses, traumatic or postsurgical inflammation, contact lens–related keratitis, nonincident cases of scleritis or episcleritis, pinguecula, and pterygia.
Demographic characteristics of scleritis and episcleritis cases and the general Kaiser Permanente Hawaii population were compared ( Table 1 ). Statistically significant differences by sex and race were noted. Women were overrepresented among scleritis patients ( P = .0498). Additionally, Pacific Islanders were the most underrepresented racial group among cases of scleritis and episcleritis compared to the general Kaiser Permanente Hawaii membership ( P = .006, P = .001). Blacks made up a significantly higher proportion of scleritis cases compared to the Kaiser Permanente Hawaii population ( P = .03).
| Kaiser Permanente Members a | Confirmed Scleritis Cases | P Value b | Confirmed Episcleritis Cases | P Value b | |
|---|---|---|---|---|---|
| Total | 217 061 | 17 | 93 | ||
| Female | 110 701 (51%) | 13 (76.5%) | .0498 | 56 (60.2%) | .08 |
| Age category (y) | |||||
| 0-14 | 40 057 (18%) | 0 | .06 | 5 (5.4%) | .0004 |
| 15-24 | 28 047 (13%) | 0 | .15 | 9 (9.7%) | .44 |
| 25-44 | 58 376 (27%) | 6 (35.3%) | .42 | 34 (36.6%) | .046 |
| 45-64 | 63 914 (29%) | 7 (41.2%) | .29 | 38 (40.9%) | .02 |
| ≥65 | 26 667 (12%) | 4 (23.5%) | .15 | 7 (7.5%) | .20 |
| Race c | N = 114 505 (53%) | N = 16 (94.1%) | N = 67 (72.0%) | ||
| Alaskan/Native American | 1463 (1%) | 0 | 1.00 | 0 | .64 |
| Asian | 46 024 (40%) | 9 (52.9%) | .33 | 27 (29.0%) | .03 |
| Black | 1758 (2%) | 2 (11.8%) | .03 | 0 | .41 |
| Pacific Islander | 31 083 (27%) | 0 | .006 | 11 (11.8%) | .001 |
| White | 30 603 (27%) | 5 (29.4%) | .79 | 29 (31.2%) | .35 |
| Other | 3574 (3%) | 0 | 1.00 | 0 | .12 |
a Demographic information as of the midpoint of the study period, January 1, 2007.
b Fisher exact test, comparing cases to Kaiser Permanente Hawaii members.
c Comparisons by race were made between self-reporters in each racial group vs all others.
The overall incidence rates of scleritis and episcleritis were 4.1 (95% CI: 2.6-6.6) and 21.7 (95% CI: 17.7-26.5) per 100 000 person-years, respectively. Separate incidence calculations for each year in the study period yielded similar rates (not reported).
Incidence rates by age and sex subgroup are also reported in Table 2 . The incidence rate of scleritis increases with age; however, variations in incidence by age category were not statistically significant. Additionally, we found that only adults had scleritis, whereas episcleritis affected all age groups. The median age at diagnosis was 56 years for scleritis (interquartile range [IQR]: 42-60) and 45 years for episcleritis (IQR: 32-54). Of scleritis cases, 76.5% (13/17) were female; of episcleritis cases, 60.2% (56/93) were female. Incidence rates varied by sex. For scleritis, female subjects had an incidence of 6.4 (95% CI: 3.8-10.8) per 100 000 person-years and male subjects had an incidence of 2.3 (95% CI: 1.0-5.6) per 100 000 person-years. For episcleritis, female subjects had an incidence of 26.0 (95% CI: 20.1-33.7) per 100 000 person-years and male subjects had an incidence of 17.7 (95% CI: 12.9-24.3) per 100 000 person-years.
| Age (y) | Scleritis | Episcleritis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||||||||
| N | Rate a | (95% CI) b | N | Rate a | (95% CI) b | N | Rate a | (95% CI) b | N | Rate a | (95% CI) b | |
| Total | 13 | 6.4 | (3.8-10.8) | 4 | 2.3 | (1.0-5.6) | 56 | 26.0 | (20.1-33.7) | 37 | 17.7 | (12.9-24.3) |
| 0-14 | 0 | 2.6 | (0.4-18.2) | 0 | 2.4 | (0.3-17.3) | 2 | 7.7 | (2.5-23.8) | 3 | 9.8 | (3.7-26.0) |
| 15-24 | 0 | 3.6 | (0.5-25.9) | 0 | 3.5 | (0.5-25.1) | 1 | 7.3 | (1.8-29.1) | 8 | 31.8 | (16.6-61.2) |
| 25-44 | 4 | 8.5 | (3.6-20.5) | 2 | 5.2 | (1.7-16.0) | 20 | 35.9 | (23.4-55.1) | 14 | 25.8 | (15.5-42.8) |
| 45-64 | 6 | 10.9 | (5.2-22.8) | 1 | 3.2 | (0.8-12.6) | 28 | 45.0 | (31.3-64.7) | 10 | 17.4 | (9.6-31.3) |
| ≥65 | 3 | 13.5 | (5.1-36.1) | 1 | 8.3 | (2.1-33.3) | 5 | 20.3 | (9.1-45.2) | 2 | 12.5 | (4.0-38.8) |
a Incidence rates are reported per 100 000 person-years.
b Range in parentheses indicates 95% confidence interval (CI).
Estimations of incidence were also made by racial subgroup ( Table 3 ). Notably, Pacific Islanders had the lowest incidence of scleritis, 1.6 (95% CI: 0.2-11.3) cases per 100 000 person-years, and the lowest incidence of episcleritis, 19.1 (95% CI: 10.8-33.6) cases per 100 000 person-years. Blacks had the highest incidence of scleritis, 83.9 (95% CI: 27.1-260.2) cases per 100 000 person-years. Whites had the highest incidence of episcleritis, 48.6 (95% CI: 34.0-69.5) cases per 100 000 person-years.
| Race | Scleritis Incidence | Episcleritis Incidence | ||
|---|---|---|---|---|
| Rate a | (95% CI) b | Rate a | (95% CI) b | |
| Overall | 4.1 | (2.6-6.6) | 21.7 | (17.7-26.5) |
| Alaskan/Native American | 33.6 | (4.7-238.5) | 33.6 | (4.7-238.5) |
| Asian | 10.8 | (5.8-20.0) | 30.2 | (20.9-43.7) |
| Black | 83.9 | (27.1-260.2) | 28.0 | (3.9-198.6) |
| Pacific Islander | 1.6 | (0.2-11.3) | 19.1 | (10.8-33.6) |
| White | 9.7 | (4.4-21.6) | 48.6 | (34.0-69.5) |
a Incidence rates are reported per 100 000 person-years.
b Range in parentheses indicates 95% confidence interval (CI).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


