Purpose
Venous air embolism (VAE) during pars plana vitrectomy (PPV) can occur owing to improper positioning of the infusion cannula in the suprachoroidal space and may lead to sudden compromise of cardiac circulation and death. This was an in vivo demonstration of fatal VAE during PPV to show that air can travel from the suprachoroidal space into the central circulation.
Design
Experimental in vivo surgical study on porcine eyes.
Methods
Experimental PPV under general anesthesia was performed on porcine eyes (Yorkshire species) at a University Surgical Training & Education Center. Infusion cannulas were placed into the suprachoroidal space and fluid–air exchange (FAE) was started with sequential increases in infusion air pressure. Vital signs of porcine animals were continuously monitored and recorded in real time during the PPV, including end-tidal carbon dioxide (ETCO 2 ), oxygen saturation (SaO 2 ), intra-arterial blood pressure, electrocardiography (EKG), and transesophageal echocardiography (TEE).
Results
Intracardiac air was detected on TEE less than 30 seconds after increasing air infusion pressure to 60 mm Hg. ETCO 2 declined precipitously, followed by hypotension and EKG changes. Oxygen desaturation was a late phenomenon. The animal died within 7 minutes of VAE. During autopsy, the heart was open under water and air escaped from the right ventricle.
Conclusion
This in vivo porcine model confirms that during the FAE in PPV, pressurized air from an infusion cannula malpositioned in the suprachoroidal space can transit through the eye to the central circulation, resulting in fatal VAE.
Pars plana vitrectomy (PPV) is generally considered to be a low-risk procedure with exceedingly remote risk of mortality. However, internationally there are sporadic reported cases of acute circulatory collapse and sudden death while fluid–air exchange (FAE) is performed during PPV. FAE is a frequent step during PPV, involving the simultaneous extraction of fluid and infusion of air under pressure into the vitreous cavity. The aim is to extrude subretinal fluid and either produce air tamponade or leave the vitreous cavity filled by air, gas, or silicone oil. Unrecognized intraoperative outward displacement of the trans-scleral infusion cannula (nonsutured or sutured) can result in intraoperative choroidal detachment or hypotony. When this occurs, it is hypothesized that air enters into the suprachoroidal space and choroidal circulation with subsequent propagation from the eye to the central venous circulation. A recent in vitro study confirmed the capacity for air infused into the suprachoroidal space to exit through the vortex veins. It has been postulated that once the opening pressure within these veins is surpassed, air may freely transit to the central venous circulation and heart. The aim of the current in vivo study is to confirm the hypothesis that VAE with acute cardiopulmonary failure can result from pneumatic choroidal effusion following a malpositioned scleral infusion cannula.
Methods
Setting
This study was approved by the Institutional Animal Care and Use Committee (IACUC #13-028) at the University of Miami (Miami, Florida).
Study Population
Two pigs (Yorkshire species) underwent isoflurane-based general anesthesia with endotracheal intubation and spontaneous ventilation. Because immediate fatality was the predicted outcome, bilateral surgery was permitted so as to minimize the number of animals used.
Operative Procedure
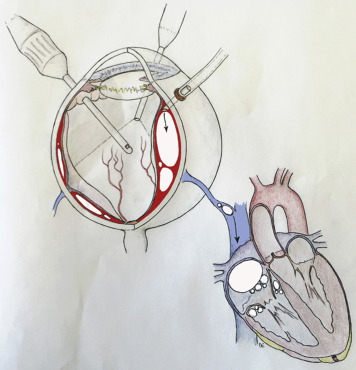
Twenty-three gauge PPV with 3 trocars placed 3 mm posterior to the surgical limbus, lensectomy, and cannulation of the suprachoroidal space were performed on a total of 3 eyes by 2 of the authors (H.W.F. and T.A.A.). Each eye was dilated using tropicamide 1% and atropine sulfate 1% drops. Globe exposure was obtained by placing a lid speculum and traction sutures. An infusion cannula was inserted through 1 of the trocar vitrectomy ports. In each instance, the surgeon performed a lensectomy and pars plana vitrectomy in the standard fashion (Versavit 2.0 generation 2.3 vitrectomy machine; Synergetics, St Louis, Missouri, USA). After routine placement of the pars plana trocar, the trocar was partially retracted through the eye wall and a light pipe was used to dissect into the suprachoroidal space under transpupilary view ( Figure 1 ). The light pipe was then removed, the infusion was attached to this trocar, and air infusion was initiated at 30 mm Hg. Infusion air pressure was incrementally increased from 30 mm Hg to 120 mm Hg.
Main Outcome Measures
Vital parameters were constantly monitored and recorded, including end-tidal carbon dioxide (ETCO 2 ), transmucosal oral pulse oximetry, intra-arterial carotid catheter (inserted via cut-down), electrocardiography (EKG), and transesophageal echocardiography (TEE; GE Vivid Q; GE Healthcare, Princeton, New Jersey, USA) using a GE 6T RS (2.9–6.7 MHz) transducer for detection of intracardiac air. The TEE was positioned at the mid-esophageal level in order to obtain a 4-chamber view. The ability to detect intracardiac air was confirmed preoperatively by the appearance of air bubbles in the right atrium and right ventricle following intravenous injection of agitated saline.
Results
All eyes underwent PPV with lensectomy and subsequent attempt at pneumatic choroidal detachment. In the first procedure (Porcine 1, left eye), after the air infusion was initiated, air pressure was raised in step-wise fashion from 30 to 90 mm Hg. Intracardiac air was not detected at any pressure. Extensive bleeding was noted, so the procedure was abandoned. In the second eye (Porcine 1, right eye), a choroidal detachment was created when air pressure was raised to 120 mm Hg. Again, intracardiac air was not detected.
After PPV with lensectomy in the first eye of another animal (Porcine 2, left eye), the light pipe was used through a partially retracted standard pars plana trocar to dissect into the suprachoroidal space. Once the space was identified through standard transpupilary observation through the operating microscope, the air infusion was placed through this trocar at 30 mm Hg. Progressive pneumatic choroidal detachment was observed. Less than 30 seconds after the air pressure was increased from 30 to 60 mm Hg, TEE revealed massive air emboli in the right-sided cavities with concomitant reduction in right ventricular function ( Figure 2 and Digital Video 1 ; Supplemental Material available at AJO.com ). This was followed by severe right ventricular dilation and leftward displacement of the intraventricular septum, indicative of biventricular interdependence and pulmonary hypertension. ETCO 2 declined precipitously, followed by hypotension and EKG changes; however, oxygen desaturation was a late phenomenon ( Figure 3 and Table ). As the right ventricle encountered increased resistance to outflow through the pulmonary vasculature, the left ventricle became emptied and pulseless electrical activity ensued. The interval from detection of intracardiac air to death was 7 minutes. Postmortem autopsy revealed air in the central venous system ( Figure 4 and Digital Video 2 ; Supplemental Material available at AJO.com ). The mediastinum was submerged in a water bath and profuse effusion of air occurred upon incision into the myocardium ( Figure 5 and Digital Video 3 ; Supplemental Material available at AJO.com ).
| Parameter | Time (min) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Heart rate (bpm) | 85 | 85 | 85 | 85 | 86 | 214 a | 90 | 92 | 96 |
| ART-S | 67 | 68 | 64 | 64 | 60 | 48 | 39 | 105 b | 63 |
| ART-D | 28 | 29 | 27 | 26 | 23 | 17 | 1 | 50 b | 9 |
| ART-M | 43 | 43 | 41 | 40 | 36 | 28 | 19 | 18 | 15 |
| ETCO 2 (mm Hg) | 51 | 51 | 36 | 30 | 22 | 18 | 14 | 0 | 8 |
| SPO 2 (mm Hg) | 99 | 99 | 98 | 98 | 98 | 97 | 97 | 96 | 31 |
| Temperature (F) | 97.7 | 97.7 | 97.7 | 97.7 | 97.7 | 97.3 | 97.2 | 97.2 | 97 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


