To date, clinical application of image-guided surgery (IGS) to otology/neurotology has been limited, but a large potential market and numerous applications support use. Such applications include control of surgical instruments (eg, turning off a drill when close to an anatomic boundary), robotic surgery (eg, robotic mastoidectomy), and minimally invasive surgery (eg, percutaneous cochlear implantation).
If they haven’t already, systems for image-guided surgery (IGS) are coming to an operating room near you. IGS systems are already commonplace for sinus surgery and neurosurgery. The appeal of IGS systems is that they allow real-time tracking of current anatomic position on preoperative CT or MRI scans. (Note: IGS systems differ from real-time intraoperative imaging, such as CT/OR or MRI/OR suites, where surgically induced anatomic changes are visible.) Although IGS systems do not replace detailed anatomic knowledge, they have been shown to improve outcomes with inexperienced and experienced surgeons .
The transition of IGS from sinus surgery and neurosurgery to otology/neurotology has been stalled by the need for a compact system that has accuracy at a level suitable for the skull base—on the order of ≤1 mm. Commercially available systems do not achieve this level of accuracy without bone-implanted fiducial markers. Once this level of accuracy is achieved, however, the use of IGS in skull base surgery will have profound implications, including safety control (eg, turning off the drill when a critical boundary is reached), robotic surgery (eg, robotic milling of the mastoid), and minimally invasive surgery (eg, percutaneous cochlear implantation).
Before presenting these exciting applications of IGS in otology/neurotology, we first must understand the basics of IGS systems. This understanding is crucial in being able to appreciate the strengths and weaknesses of IGS. Contained herein is (1) a description of IGS systems focusing on the “accuracy” of such systems, (2) a review of the current commercially available systems, and (3) an overview of future applications of IGS in otology/neurotology.
How image-guided surgery systems work
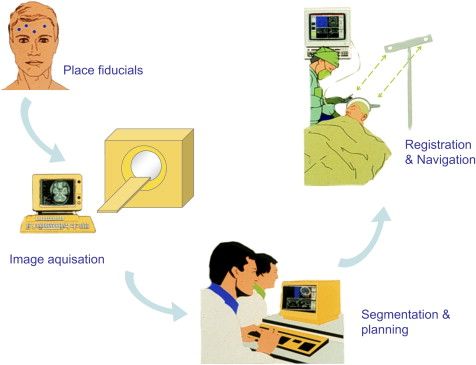
IGS systems are analogous to global positioning systems but on a much smaller, local scale. The typical set-up is depicted schematically in Fig. 1 . The systems consist of (1) a set of markers on a patient (called “fiducial markers” or simply “fiducials”), which are present during preoperative CT or MRI scanning, (2) a computer tracking system used in the operating room that aligns the markers in the CT or MRI to the current anatomy and tracks a patient’s fiducial markers within the operating room. For tracking, most systems (eg, BrainLAB, Feldkirchen, Germany; Medtronic, Minneapolis, Minnesota; and Stryker, Stryker Leibinger, Inc., Kalamazoo, Michigan) use infrared technology, whereas one system (GE Medical Systems, Lawrence, Massachusetts) uses electromagnetic field distortion technology. Infrared systems are limited by line of sight, whereas electromagnetic systems are distorted by metal instruments within the surgical field.
Fiducial markers
The key to IGS systems are the fiducial markers. The familiar computer axiom that holds that “garbage in equals garbage out” is applicable to IGS systems because the only items visible to the IGS system are the fiducials. Tracking of unknown anatomy depends on actively matching fiducial markers in the preoperative scan to those within the operating room. This matching requires an accurate determination of the position of each fiducial, a process that is termed fiducial “localization.” Without excellent fiducial localization, all anatomic point localization is compromised. Fiducial markers range from neurosurgical N-frames (rarely used given less cumbersome choices), bone-implanted screws, proprietary head-frames (eg, GE Instatrack head frame), skin-affixed adhesive markers, contours of surfaces obtained by laser scanning, and dental-affixed mouthpieces. The requirements for excellent fiducials are that (1) they are repeatedly positioned in exactly the same location relative to patient anatomy during radiographic imaging and in the operating room (a flaw for all non–bone-affixed systems), (2) they surround the anatomic region of interest, (3) a sizeable number of markers is used, and (4) they can be accurately localized.
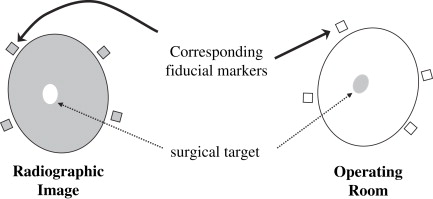
Why are fiducial markers the key? Fiducial markers are the only things visible to the IGS system. Everything else depends on them. Once a CT or MRI scan is loaded into the IGS computer, the operator finds the same fiducial markers on the patient in the operating room, and the computer’s job is to align/superimpose the fiducial markers from the CT or MRI scan to those found in the operating room. To the extent that the anatomy is rigid, fiducial alignment ensures that the anatomy, including surgical targets, is also aligned. This process is called “registration.” This important process deserves a precise definition: Registration is the alignment of anatomic points from the radiographic scan (eg, CT or MRI) with their true positions in the operating room. This process is schematically illustrated in Figs. 2–4 .


Error within image-guided surgery systems
As one can imagine, error is inherent to the process. Although not often discussed in brochures or advertisements, an engineering standard does exist in analysis of IGS. This analysis assigns error to each step of the process, as shown in Fig. 4 . First is “fiducial localization error” (FLE), which is the error in identifying the positions of the fiducial markers in the radiographic images (FLE rad ) and in the operating room (FLE OR ). Contributions to FLE rad include the resolution of the CT or MRI scan, image distortion of the scan, and noise in the scan. Components of FLE OR include human error in identifying the fiducial markers and error inherent in the tracking system. Overall, FLE represents the error in finding the fiducial markers. In an ideal world, the location of fiducial markers could be determined perfectly; given the imperfections of the real world, however, this rarely happens. Thus FLE is rarely zero. When fiducial locations are imperfectly determined, alignment of the markers from the radiographic study to the operating room is also imperfect. The resultant error in aligning fiducial markers is termed “fiducial registration error” (FRE) and is graphically depicted in Fig. 4 . To minimize this error, a mathematical best-fit algorithm is used to minimize the differences between the corresponding image and patient fiducials. (Most systems use a strategy that minimizes the sum of the squares of the distances between fiducial markers). The FRE or a derivative of it is the number typically displayed on IGS systems after registration as an indication of the goodness of fit.
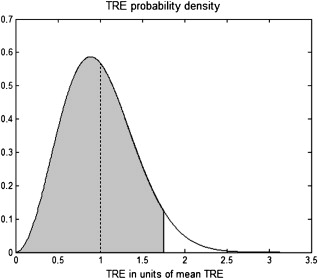
Only after registration is done can IGS tracking begin. Once tracking is initiated, the surgeon identifies a point of anatomic interest. The difference between where the IGS system says the anatomy is located and its true position is termed “target registration error” (TRE)—the accuracy of the system. TRE and FRE each statistically depend on FLE via relationships that are beyond the scope of this article. (The interested reader is directed to Fitzpatrick and colleagues .) An important point to remember is that TRE for a system is not well described by a single number but rather a statistical distribution. When one states that the accuracy of a system is 1 mm, what is actually being implied is that the average accuracy of the system is 1 mm, but the accuracy may in fact be higher or lower at any particular time. (The statistical distribution is a chi-squared distribution with 3 degrees of freedom [ Fig. 5 ]). When comparing systems, the TRE within the anatomic region of interest should be compared.
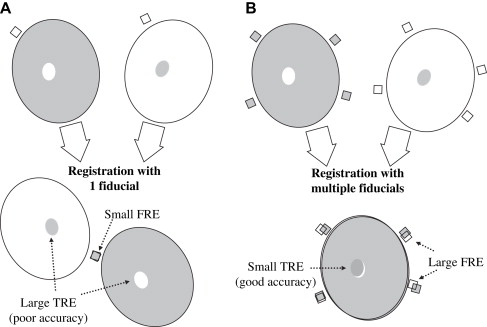
A common misconception is that lower FRE means a more accurate registration, which is not necessarily true. Although most systems have a threshold below which FRE must fall to proceed with IGS, lowering FRE further below this threshold does not mean higher registration accuracy. Some authors have called for removal of fiducial points from the registration to lower FRE . This approach is dangerously flawed. Although FRE tends statistically to decrease with fewer fiducials, error in target alignment (TRE) tends to increase . Because FRE can be observed directly, it is tempting to removal fiducials to see a reassuringly smaller error value displayed on the IGS screen, but the chances are great that removing them will increase the error that counts—the error in hitting the target (ie, TRE). Many examples can be given to illustrate this effect, but the simplest is the case of one fiducial. When only one fiducial is used, FRE may be easily reduced to zero, but as is depicted in Fig. 6 , a zero fiducial registration error clearly does not mean a more accurate registration. When more markers are used, because of the uncertainty in their localization (FLE), FRE tends to rise but TRE likely decreases, which results in better accuracy. For clinical use, more fiducial markers are better, even if it means a larger FRE.
For laser scanning systems, the analysis described in the preceding paragraphs is as follows:
- •
A three-dimensional surface model is constructed from the radiographic data, and multiple points are captured from the surface of the patient in the operating room using a scanning laser.
- •
The collection of these anatomic points (fiducials) is compared with the surface generated from the radiographic data and aligned such that the distance from the collection of points to the surface is minimized. This concept is similar to using multiple fiducial markers.
- •
A larger FRE may result from more anatomic points captured during laser scanning. This larger FRE does not mean that the TRE would be higher; rather the TRE would be expected to be lower. More laser scans are better even if it means a larger FRE.
Commercially available image-guided surgery systems
Although no IGS systems are marketed for lateral skull base surgery, many are approved by the US Food and Drug Administration (FDA) and currently are used for sinus surgery and neurosurgery. An in-depth review of the accuracy of such systems was performed for a prior publication and is repeated in this article with permission from the publisher.
The four leading commercial IGS systems used for sinus surgery are (in alphabetical order):
BrainLAB system (BrainLAB, Feldkirchen, Germany)
InstaTrak System (GE Medical Systems, Lawrence, Massachusetts)
LandmarX and StealthStation system (Medtronic, Minneapolis, Minnesota)
StrykerImage Guidance System (Stryker Leibinger, Kalamazoo, Michigan)
For each of these systems, the literature was reviewed to find the most relevant article reporting accuracy of the system. Each company was contacted to determine whether the cited study was the most up-to-date regarding error analysis.
BrainLAB
For the BrainLAB system, no error studies could be identified specifically for sinus surgery, but such work has been done for neurosurgical applications, which use similar fiducials and registration methods. In a study performed at the University of Regensburg, Germany, error analysis for 36 patients undergoing intracranial surgery was performed . FRE using skin-affixed fiducial markers was reported as 1.10 ± 0.53 mm; using laser skin contouring, FRE was reported as 1.36 ± 0.34 mm. TRE was calculated by comparing a skin-affixed marker on the patient with that location in the corresponding radiographic image; for the skin-affixed marker registration, TRE was reported as 1.31 ± 0.87, and for laser skin contouring, TRE was reported as 2.77 ± 1.64 mm.
InstaTrak
For the InstaTrak System, a multicenter, multisurgeon study was performed and published in Laryngoscope in 1997 . In this study, registration was performed either with six skin-affixed markers or a proprietary headset. TRE was measured using two skin-affixed targets placed on the lateral right and left supraorbital rims. FRE was not reported. For the skin-affixed fiducial registration, a TRE of 1.97 mm with a 95% CI, of 1.75 to 2.23 and a maximum value of 6.09 mm was reported. For the headset registration, a TRE of 2.28 mm with a 95% CI, of 2.02 to 2.53 and a maximum value of 5.08 mm was reported.
LandmarX
For the LandmarX system, Metson and colleagues performed a prospective study of 34 physicians performing 754 sinus cases over a 2.5-year period. Using five anatomic key points as fiducials (these points are undefined), they reported “mean accuracy of anatomical localization at the start of surgery was 1.69 ± 0.38 mm (range, 1.53 ± 0.41 mm to 1.79 ± 0.53 mm).” Although the specific methods are not given, this study seems to report FLE—the error associated with repeated identification of the fiducials—and not TRE. Hence the question mark in Table 1 .



