Purpose
To describe qualitative characteristics of drusen in eyes with nonadvanced age-related macular degeneration (AMD) using polarization-sensitive optical coherence tomography (OCT).
Design
Cross-sectional study.
Methods
Twenty-five eyes of 25 patients with early to intermediate (nonadvanced) AMD were imaged with polarization-sensitive OCT using macular volume scans. All individual drusen in each B-scan were manually delineated by experts certified by a reading center and graded for 6 different morphologic characteristics based on a defined classification scheme, including the presence of internal depolarizing structures and associated depolarizing foci. With the use of a custom-made software, the central B-scan of each individual druse was selected and used to analyze its location, diameter, and characteristics and assess the prevalence of the different features and relations between them.
Results
Using the macular volume scans, 6224 individual drusen could be identified, including their position within the retina, their characteristics, and their association with any pigmentary alterations. The most common drusen type was a convex-shaped druse with homogeneous medium internal reflectivity and no depolarizing contents (55.3% of drusen). A total of 30.5% of the drusen exhibited internal depolarizing material; 0.3% presented overlying hyperreflective foci, and in 54.5% the foci were also depolarizing. Significant correlations were found between the diameter of the drusen and their distribution throughout the retina, shape, homogeneity of internal reflectivity, presence of internal depolarizing characteristics, and presence of overlying foci ( P < .001 each). Significant relations were found between reflectivity, homogeneity, and polarization-sensitive internal characteristics ( P < .001).
Conclusions
Polarization-sensitive OCT reveals characteristic morphologic features of different druse types highlighting the pathophysiological spectrum of early to intermediate AMD.
The presence of drusen and pigmentary changes within the retina are a characteristic finding of early and intermediate age-related macular degeneration (AMD), the leading cause of irreversible blindness in developed countries. The increase of drusen size is widely recognized as an indicator for progression toward advanced stages of AMD, as well as the development of pigmentary changes, seen as hyperreflective foci in the inner retinal layers in spectral-domain optical coherence tomography (OCT) images. However, the progression rates of AMD disease can vary between individual patients, and drusen themselves show different growth patterns. Furthermore, studies underlined that drusen individually present a wide spectrum of different compositions and, consequently, different morphologic features in histologic sections. In vivo, drusen morphology was investigated using spectral-domain OCT imaging, and several distinct characteristics were identified. These different morphologic features, including the presence of hyperreflective foci, might represent ongoing biologic dynamics in the course of the disease that might lead to neurodegenerative processes and loss of visual function.
Polarization-sensitive spectral-domain OCT is a technology based on spectral-domain OCT. It provides the same high-resolution images as spectral-domain-based devices, which measure the intensity of the backscattered light. As additional information, polarization-sensitive OCT is able to identify the polarization state. An overview of this selective imaging technique has recently been presented.
Studies could show that most cellular parts of the retina preserve the polarization state of the incoming and reflected light, with the exception of melanin. Melanin is found mostly in retinal pigment epithelium (RPE) cell organelles, but was observed in other structures too, including pathologic alterations such as pigmentary changes and inside of drusen.
In previous work of our group, which outlined the performance of a drusen segmentation algorithm based on polarization-sensitive information, we also found that some drusen featured additional depolarizing characteristics that provoked “errors” in the automated delineation of the drusen contour, but that may in fact represent additional characteristics relevant for disease progression. The prognostic value of drusen-related morphologic features is completely unknown. Many proposals for staging disease activity have been made based on the appearance or imaging features of drusen observed using such aids as the scanning laser ophthalmoscope and, recently, spectral-domain OCT.
In this study, the characteristics of drusen and pigmentary changes in early and intermediate AMD using polarization-sensitive OCT were systematically investigated. Based on a previous attempt to classify drusen morphology seen in intensity-based spectral-domain OCT, additional polarization-sensitive features of drusen were characterized. The detected characteristics were correlated to known risk factors for disease progression such as drusen size or the presence of overlying pigmentary alterations, with the aim of gaining new insights into drusen composition and their role in AMD disease.
Methods
In this observational cross-sectional study, we evaluated the polarization-sensitive OCT volume scans of 25 eyes of 25 patients with drusen of AREDS (Age-Related Eye Disease Study) categories 2 and 3. All examinations were performed at the Department of Ophthalmology, Medical University of Vienna. The study protocol was approved by the ethics committee of the Medical University of Vienna and adhered to the Declaration of Helsinki (2008). In this study protocol, all examinations listed below were included, and the patients had to give their informed consent before inclusion to the study.
Patients
Patients were selected according to the standard AREDS classification. Only eyes with drusen of the AREDS categories 2 and 3 were included in the study. Category 2 is defined as the presence of extensive small (<63 μm in diameter) or nonextensive intermediate drusen (between 63 μm and 125 μm) with or without pigment epithelial abnormalities in at least 1 eye. Category 3 requires extensive intermediate or large (≥125 μm) drusen and/or noncentral geographic atrophy in at least 1 eye. Eyes were examined ophthalmoscopically by an experienced retinologist and selected for study inclusion.
Patients presenting with ocular media opacity due to cornea or lens changes or other diseases potentially influencing scan quality such as macular edema were excluded. Patients with a history of ocular trauma or surgery other than uncomplicated cataract surgery were also excluded.
Imaging Protocol
Patients meeting the protocol criteria were informed about the study aims and procedures. After patients had given informed consent, they were included in the study and underwent a complete and standardized ophthalmic examination. The best-corrected visual acuity (BCVA) was obtained and mydriatic eye drops were administered. At maximum mydriasis, eyes were scanned with a conventional spectral-domain OCT (Spectralis; Heidelberg Engineering, Heidelberg, Germany) using a macular volume scan (97 × 1024 scan pattern covering an area of 20 × 20 degrees, with an averaging of 20 frames). Furthermore, eyes were scanned with the polarization-sensitive OCT using the 64 × 1024 volume scan pattern (ie, 64 B-scans consisting of 1024 A-scans) covering an area of 17.6 × 19.0 degree.
Technology of the Polarization-Sensitive Optical Coherence Tomography Device
The polarization-sensitive OCT images analyzed in this study were obtained using a prototype engineered by the Center for Medical Physics and Biomedical Engineering, Medical University of Vienna. To summarize, the system is able to retrieve the following parameters simultaneously: intensity of the backscattered light (as in standard spectral-domain OCT imaging), retardation (phase shift between 2 orthogonal linear polarization states caused by birefringence), fast axis orientation (birefringent axis orientation of the sample relative to the orientation of the instrument), and degree of polarization uniformity. A superluminescent diode (Superlum Diodes, Inc, Moscow, Russia) centered at 839 nm with a full width at half maximum bandwidth of 58 nm served as the light source. The laser power incident on the cornea was well below the laser safety standards. Scanning laser ophthalmoscope images scanned by the instrument and OCT B-scan images were recorded and displayed in real time to allow an optimized alignment of the eye under investigation. Three-dimensional (3D) datasets covering a scan field of 17.6 × 19.0 degrees (approximately 6.2 × 6.7 mm 2 ) with an imaging depth of 3.3 mm in air were recorded at an operating speed of 20 000 A-scans per second. One out of 3 sampling patterns (64 × 1024, 128 × 512, 256 × 256) could be selected. Only datasets recorded with the 64 × 1024 scan pattern were used in the study. Scans of unacceptable quality (eg, motion artifacts) were dismissed and repeated until satisfactory results were achieved.
Classification of Drusen
Two expert readers (F. Schlanitz and M. Platzer) independently graded the OCT images of each patient. Individual B-scans were reviewed and every druse observed in these images was manually segmented. Each detectable localized pigment epithelial elevation larger than 25 μm in diameter was regarded as a druse entity in accordance with the histopathologic definition of drusen and based on other studies that have identified drusen in OCT images. Drusen were further categorized as small (<63 μm in diameter), intermediate (between 63 and 125 μm), and large (between 125 and 350 μm). RPE elevations wider than 350 μm in diameter were classified as drusenoid pigment epithelial detachments according to the AREDS classification.
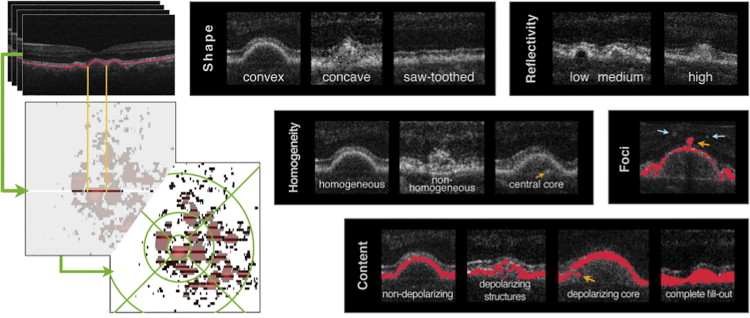
Segmentation and classification of the drusen was done using a custom-made Matlab program (Matlab 7.1; Mathworks Inc, Natick, Massachusetts, USA) with a graphical user interface. With the help of this program, every single druse in each B-scan was manually segmented and classified using the druse classification system introduced by Khanifar and associates. This classification encompasses the shape of the RPE elevation (convex, ie, dome-shaped; concave, ie, pointed; or saw-toothed), the reflectivity of the druse (low, medium, or high, in relation to the photoreceptor layer), the homogeneity of the druse’s content (homogeneous reflectivity, inhomogeneous with central core/focus of hyperreflectivity and inhomogeneous without a central core), and the presence or absence of hyperreflective foci above the druse.
To classify the polarization-sensitive information, this classification system was expanded to include 2 additional categories: depolarizing structures within the druse (absence of depolarizing material, single depolarizing core within the druse, inhomogeneous depolarizing structures within the druse, and a complete fill-out of the druse with depolarizing material) and the presence or absence of depolarizing foci above the druse ( Figure 1 ). These details can only be obtained using the detection mode of a polarization-sensitive OCT. A summary of the categories and grading is shown in Table 1 .
| Classification | Description |
|---|---|
| Shape | |
| Convex | Dome-shaped RPE elevation |
| Concave | Pointed RPE elevation |
| Saw-toothed | Small, jagged elevations of RPE |
| Reflectivity | |
| Low | Isoreflective or hyporeflective relative to the photoreceptor layer |
| Medium | Hyperreflective relative to the photoreceptor layer and hyporeflective relative to the RPE |
| High | Isoreflective or hyperreflective relative to the RPE |
| Homogeneity | |
| Homogeneous | Relatively uniform internal reflectivity |
| Nonhomogeneous with a central core | Varying internal reflectivity with a distinct single focus of hyperreflectivity |
| Nonhomogeneous without a central core | |
| Hyperreflective foci | |
| The presence or absence of hyperreflective points within the neurosensory retina overlying areas of RPE elevations | |
| Depolarizing structures within the druse | |
| Absence of depolarizing material | |
| Depolarizing core | Single depolarizing focus within the druse |
| Depolarizing material | Varying, inhomogeneous distribution of depolarizing material within the druse |
| Complete fill-out | If the complete druse content produces a depolarizing signal |
| Depolarizing foci | |
| The presence or absence of depolarizing points within the neurosensory retina overlying areas of RPE elevations | |
Data Analysis and Statistical Methods
Statistical analysis was carried out using PASW Statistics 18.0 (SPSS Inc, Chicago, Illinois, USA) and Matlab (Matlab 7.1; Mathworks Inc).
The manually outlined location, diameter, height, and the 6 characteristics of druse morphology identified were allocated to a matrix. Using this matrix, the Matlab program displayed a map for each eye representing the location and extent of the drusen. Using this map, the central slice of each delineated druse was selected and its characteristics were transferred into SPSS for further statistical analysis ( Figure 1 , bottom left images). In addition, graders indicated the location of each druse within the standard AREDS grading grid. This grid consists of a central circle centered at the fovea with 1000 μm diameter (zone 1), and a second circle with 3000 μm and a third with 6000 μm diameter (zone 2 and 3, respectively). The rate of agreement on the classification of drusen characteristics between the 2 graders was assessed by calculating the percentage of agreement. The prevalence of each characteristic, and the druse diameter and distribution within the AREDS grid, were compared using the Kruskal-Wallis test with subsequent Mann-Whitney U tests. Owing to the large number of different factors, the results were corrected for multiple testing using the Shaffer correction. A corrected P value below 5% was considered significant.
Results
Number and Size of Drusen
Twenty-five eyes of 25 patients presenting with AREDS categories 2 and 3 were examined. The patients’ mean age was 72 years (standard deviation [SD] ±6, range 60–85), and 14 were women. The mean BCVA was 0.9 (SD ±0.17, range 0.6–1.25), and 5 patients were pseudophakic. In total, 8729 RPE elevations were found and analyzed in the single B-scans. The mean druse area per eye was 6.0 mm 2 . Using the 3D drusen maps, 6224 single drusen were identified and their central slice was further analyzed. The mean number of drusen <350 μm in diameter per eye was 237 (SD ±136, range 25–645) with a mean diameter of 114 μm (SD ±69 μm, range 29–345 μm). Of all drusen, 25.2% were small, 41.6% intermediate, and 32.2% large. Drusenoid pigment epithelial detachments with a diameter ≥350 μm were found in 23 eyes, with a mean number of 12 individual drusenoid pigment epithelial detachments per eye (SD ±13, range 0–53). Therefore, a total of 291 individual drusenoid pigment epithelial detachments were detected, with a mean diameter of 504 μm (SD ±163 μm, range 351–1370 μm).
Morphology of Drusen
The prevalence of each of the 6 morphologic druse characteristics is shown in Table 2 . A convex contour was seen in 88.9% of all drusen and 96.2% of all drusenoid pigment epithelial detachments. Regarding the internal reflectivity, 90.5% of the drusen and 95.9% of the drusenoid pigment epithelial detachments exhibited a medium reflectivity. The internal reflectivity was homogeneous in 79.5% of the drusen and 69.4% of the drusenoid pigment epithelial detachments. The most common internal depolarizing characteristic was a nonhomogeneous distribution of depolarizing structures, which was present in 17.8% of all drusen and 19.6% of all drusenoid pigment epithelial detachments. A total of 68.5% of all drusen and 72.9% of all drusenoid pigment epithelial detachments showed no internal depolarizing signal. Hyperreflective foci were present in 16 single drusen (0.3%) and 12 drusenoid pigment epithelial detachments (4.1%). Overlying depolarizing foci were observed in 9 drusen (0.2%) and 10 drusenoid pigment epithelial detachments (3.4%). By combining the drusen characteristics, different “types” of drusen can be generated, as described by Khanifar and associates. The most common drusen type observed in this study was convex shaped, with medium, homogeneous internal reflectivity and nondepolarizing contents, and no overlying foci (55.3% of drusen and 53.6% of drusenoid pigment epithelial detachments). The most common type with internal depolarizing characteristics was convex shaped, with medium and homogeneous internal reflectivity, and patchy depolarizing contents (8.7% of drusen and 7.3% of drusenoid pigment epithelial detachments).
| Drusen Morphology | Small | Intermediate | Large | Drusenoid Pigment Epithelial Detachments | ||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | |
| Shape | ||||||||
| Concave | 170 | 11.4% | 253 | 10.3% | 118 | 6.0% | 4 | 1.4% |
| Convex | 1299 | 87.0% | 2165 | 87.7% | 1809 | 91.7% | 280 | 96.2% |
| Saw-toothed | 0 | 0.0% | 10 | 0.4% | 29 | 1.5% | 6 | 2.1% |
| Not classifiable | 24 | 1.6% | 40 | 1.6% | 16 | 0.8% | 1 | 0.3% |
| Reflectivity | ||||||||
| Low | 21 | 1.4% | 25 | 1.0% | 28 | 1.4% | 5 | 1.7% |
| Medium | 1348 | 90.3% | 2226 | 90.2% | 1798 | 91.2% | 279 | 95.9% |
| High | 96 | 6.4% | 187 | 7.6% | 110 | 5.6% | 2 | 0.7% |
| Not classifiable | 28 | 1.9% | 30 | 1.2% | 36 | 1.8% | 5 | 1.7% |
| Homogeneity | ||||||||
| Homogenous | 1323 | 88.6% | 2008 | 81.4% | 1386 | 70.3% | 202 | 69.4% |
| Nonhomogenous + core | 51 | 3.4% | 180 | 7.3% | 253 | 12.8% | 30 | 10.3% |
| Nonhomogenous | 88 | 5.9% | 242 | 9.8% | 292 | 14.8% | 53 | 18.2% |
| Not classifiable | 31 | 2.1% | 38 | 1.5% | 41 | 2.1% | 6 | 2.1% |
| Depolarizing contents | ||||||||
| Nondepolarizing | 1224 | 82.0% | 1716 | 69.5% | 1123 | 56.9% | 212 | 72.9% |
| Nonhomogenous + core | 44 | 2.9% | 144 | 5.8% | 246 | 12.5% | 18 | 6.2% |
| Nonhomogenous depolarizing | 125 | 8.4% | 422 | 17.1% | 507 | 25.7% | 57 | 19.6% |
| Complete fill-out | 98 | 6.6% | 166 | 6.7% | 61 | 3.1% | 1 | 0.3% |
| Not classifiable | 2 | 0.1% | 20 | 0.8% | 35 | 1.8% | 3 | 1.0% |
| Hyperreflective foci | ||||||||
| Absence | 1492 | 99.9% | 2463 | 99.8% | 1962 | 99.5% | 279 | 95.9% |
| Presence | 1 | 0.1% | 5 | 0.2% | 10 | 0.5% | 12 | 4.1% |
| Depolarizing foci | ||||||||
| Absence | 1493 | 100.0% | 2462 | 99.8% | 1968 | 99.8% | 281 | 96.6% |
| Presence | 0 | 0.0% | 5 | 0.2% | 4 | 0.2% | 10 | 3.4% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


