Purpose
To investigate the clinical manifestations and visual prognosis of retinal artery occlusion resulting from cosmetic facial filler injections.
Design
Retrospective, noncomparative case series.
Methods
Setting . Institutional. Study Population . Twelve consecutive patients with retinal artery occlusion caused by cosmetic facial filler injections. Main Outcome Measures . Filler materials, injection sites, best-corrected visual acuities, fundus fluorescein angiography and optical coherence tomography findings, and associated ocular and systemic manifestations.
Results
Seven, 2, and 3 patients had ophthalmic, central retinal, and branch retinal artery occlusions, respectively. Injected materials included autologous fat (7 cases), hyaluronic acid (4 cases), and collagen (1 case), and injection sites were the glabellar region (7 cases), nasolabial fold (4 cases), or both (1 case). Injected autologous fat was associated with worse final best-corrected visual acuity than the other materials. All patients with ophthalmic artery occlusion had ocular pain and no improvement in best-corrected visual acuity. Optical coherence tomography revealed thinner and less vascular choroids in eyes with ophthalmic artery occlusion than in adjacent normal eyes. Concomitant brain infarction developed in 2 cases each of central retinal artery occlusion and ophthalmic artery occlusion. Phthisis developed in 1 case of ophthalmic artery occlusion.
Conclusions
Cosmetic filler injections into the glabellar region or nasolabial fold can cause retinal artery occlusion. Iatrogenic ophthalmic artery occlusion is associated with painful blindness, a thin choroid, brain infarction, and poor visual outcomes, particularly when autologous fat is used. Ophthalmic examination and systematic brain magnetic resonance imaging should be performed in patients with ocular pain after such injections.
Aesthetic soft-tissue augmentation of the face by filler injections is dramatically increasing in popularity. Although autologous fat injection for facial soft-tissue augmentation is considered safe, retinal artery occlusion in young, healthy patients has been reported after this procedure. In addition to autologous fat, the most popular fillers for cosmetic surgery are composed of partially cross-linked hyaluronic acid. Recently, 1 case of retinal artery occlusion as a complication of cosmetic injection of hyaluronic acid has been reported. Most cases of cosmetic facial filler injection-associated retinal artery occlusion result in blindness in the affected eye.
Despite the increasing number of cases of retinal artery occlusion resulting from cosmetic facial filler injections, the clinical features and visual outcomes of this condition and the causative surgical procedures are not well established. Adequate knowledge about this visually impairing iatrogenic complication is necessary to prevent the condition itself and subsequent blindness. Therefore, in this study, we aimed to investigate the clinical manifestations and visual prognosis of retinal artery occlusion resulting from cosmetic facial filler injections.
Methods
The electronic medical records of consecutive patients treated from January 2003 through January 2012 who met the following criteria were reviewed retrospectively: (1) nonarteritic retinal artery occlusion newly diagnosed by fundus fluorescein angiography; (2) no history of intraocular surgery or vascular interventions for retinal artery occlusion before symptom development; and (3) history of cosmetic facial filler injection immediately before retinal artery occlusion.
The collected data included information on underlying diseases, demographics, injection sites, injected substances, initial and final best-corrected visual acuities (BCVAs), associated ocular symptoms and systemic problems, duration of follow-up, and type of treatment (intra-arterial thrombolysis or conservative therapy). Findings of spectral-domain optical coherence tomography (SD OCT), fundus fluorescein angiography, and brain magnetic resonance imaging, including diffusion-weighted imaging, also were recorded. Choroidal thickness was measured in the fovea by SD OCT with an enhanced depth imaging protocol. Snellen visual acuities were converted to logarithm of the minimal angle of resolution measurements, and hand movements, light perception, and no light perception were designated as 4, 5, and 6, respectively.
In some patients, superselective intra-arterial thrombolysis with urokinase or mechanical disruption was attempted, after obtaining informed consent, within 24 hours from the symptom onset; the techniques were performed as described previously. Otherwise, the patients were managed by various conservative therapies including observation, anterior chamber paracentesis, ocular digital massage, and mannitol infusion.
The cases of iatrogenic retinal artery occlusion were divided according to the affected arteries, as follows: (1) ophthalmic artery occlusion, (2) central retinal artery occlusion, and (3) branch retinal artery occlusion. Ophthalmic artery occlusion was defined as central retinal artery occlusion with evidence of choroidal ischemia and definite embolic occlusion of the ophthalmic artery on cerebral angiography. Central retinal artery occlusion applied to cases without evidence of choroidal ischemia and definite embolic occlusion of the ophthalmic artery on cerebral angiography.
Statistical analyses were performed by using SPSS software version 18.0 (IBM Inc, Chicago, Illinois, USA). The Mann–Whitney U test was used to compare nonparametric variables and BCVAs among the groups. The Wilcoxon signed-rank test was used to compare the initial and final BCVAs. A P value less than .05 was considered significant.
Results
Twelve consecutive patients with cosmetic facial filler injection-associated retinal artery occlusion were included in the study. Of these, 7, 2, and 3 patients had ophthalmic artery occlusion, central retinal artery occlusion, and branch retinal artery occlusion, respectively. All the patients had a history of sudden visual loss immediately after the injections. Further, all were women, and their mean age was 30.8 ± 12.8 years (range, 18 to 66 years). The mean follow-up duration was 17.1 ± 25.0 weeks. Almost all the patients were healthy, without underlying diseases; patient 1 had hypertension.
The clinical characteristics of the 12 patients with iatrogenic retinal artery occlusion are described in Table 1 . With respect to the injected substances, autologous fat was injected in 7 cases (6 cases of ophthalmic artery occlusion and 1 case of central retinal artery occlusion), hyaluronic acid was injected in 4 cases (1 case of ophthalmic artery occlusion and 3 cases of branch retinal artery occlusion), and collagen was injected in 1 case of central retinal artery occlusion. The injection sites included the glabellar region (7 cases, 58.3%), the nasolabial fold (4 cases, 33%), or both regions (1 case, 8.3%).
| No. | Age (y) | Sex | Diagnosis | Eye | Cosmetic Injection | Treatment | Time to Treatment or Visit | Ocular Pain | Associated Ocular Symptom | Initial BCVA | Final BCVA | Follow-up (day) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Substance | Site | ||||||||||||
| 1 | 66 | F | OAO | L | Autologous fat | L: glabella | IAT | Immediate | (+) | Ptosis, ophthalmoplegia | NLP | NLP | 5 |
| 2 | 40 | F | OAO | L | Autologous fat | L: Nasolabial | IAT | Immediate | (+) | Large XT, ophthalmoplegia, | NLP | NLP | 511 |
| 3 | 18 | F | OAO | R | Autologous fat | R: Nasolabial | IAT | Immediate | (+) | Ptosis, ET, ophthalmoplegia, | NLP | NLP | 430 |
| 4 | 32 | F | OAO | R | Hyaluronic acid | R: Nasolabial & glabella | IAT | Immediate | (+) | Ptosis, XT, ophthalmoplegia, Cornea edema | NLP | NLP | 3 |
| 5 | 24 | F | OAO | L | Autologous fat | L: Glabella | (−) | 1 wk | (+) | Ptosis, XT, ophthalmoplegia, RAPD, MCA infarction | NLP | NLP | 63 |
| 6 | 37 | F | OAO | R | Autologous fat | R: Glabella | ACP | Immediate | (+) | XT, ophthalmoplegia, RAPD | NLP | NLP | 3 |
| 7 | 19 | F | OAO | L | Autologous fat | L: Glabella | ACP | 2 hr | (+) | XT | NLP | NLP | 40 |
| 8 | 29 | F | CRAO | L | Collagen | L: Glabella | Massage, Mannitol | 1 hr | (−) | RAPD | CF | 0.3 | 51 |
| 9 | 26 | F | CRAO | L | Autologous fat | L: Glabella | ACP | 2 days | (−) | B: ACA, and L: MCA infarction | LP | LP | 16 |
| 10 | 26 | F | BRAO | L | Hyaluronic acid | L: Nasolabial | (−) | 2 wks | (−) | L: inferior VFD | 1 | 1 | 95 |
| 11 | 26 | F | BRAO | L | Hyaluronic acid | L: Glabella | Massage, ACP | 5 hrs | (−) | L: inferior VFD involving center | 0.7 | 0.15 | 202 |
| 12 | 26 | F | BRAO | R | Hyaluronic acid | R: Nasolabial | (−) | 3 wks | (−) | R: inferotemporal VFD | 1 | 1 | 14 |
Visual decline was the most severe in the patients with iatrogenic ophthalmic artery occlusion, followed by iatrogenic central retinal artery occlusion and iatrogenic branch retinal artery occlusion (final BCVAs: 6.00 ± 0.00 logMAR units, 2.76 ± 3.17 logMAR units, and 2.23 ± 3.28 logMAR units, respectively). Regarding the injected substances, autologous fat injection resulted in worse final BCVAs than hyaluronic acid or collagen injections (n = 12; 5.86 ± 0.38 logMAR units vs. 1.47 ± 2.56 logMAR units; P = .010).
Ophthalmic Artery Occlusion (n = 7)
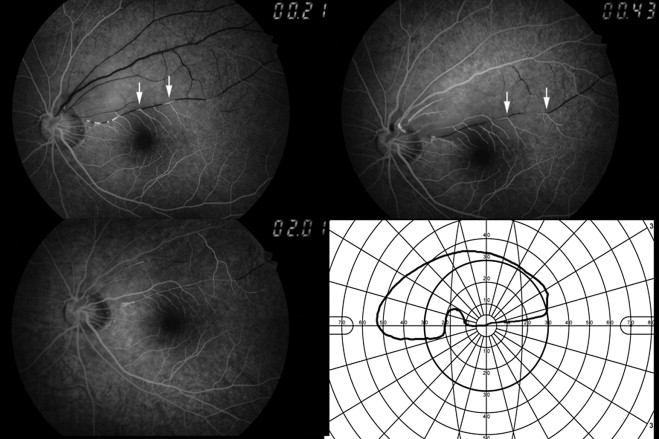
Iatrogenic ophthalmic artery occlusion was characterized by severe ocular pain in the affected eye immediately after the injection. Fundus fluorescein angiography showed no retinal perfusion and attenuated choroidal perfusion in the patients with this condition. Internal carotid angiography with transfemoral cerebral angiography showed occluded ophthalmic arteries and no choroidal flush ( Figure 1 ). Intra-arterial fat emboli were well visualized by SD OCT ( Figure 1 ). Further, the mean choroidal thickness in the affected eyes (cases 1, 3, 4, and 7; n = 4; mean ± standard deviation, 198.3 ± 49.4 μm) was less than that in the adjacent normal eyes (n = 4; mean ± standard deviation, 347.5 ± 74.3 μm; P = .014; Figure 2 ). Decreased vascularity in both the choriocapillaris and large choroidal vessels also was observed.
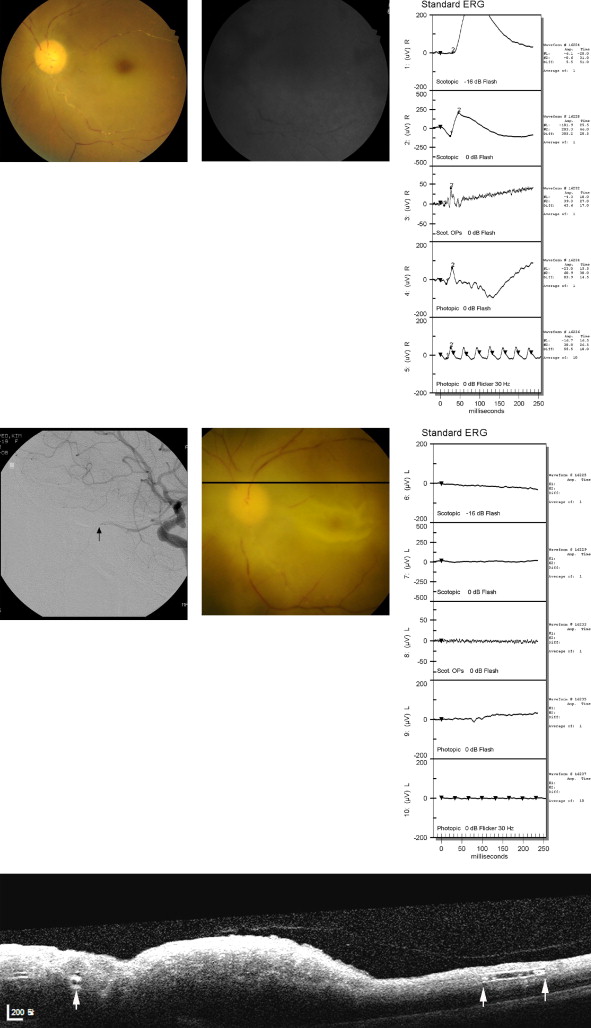

One of the 7 patients experienced combined brain infarction by fat embolism after autologous fat injection ( Figure 3 ). Associated initial ocular problems in 7 patients included ophthalmoplegia (6 cases), horizontal strabismus (6 cases, including 5 of exotropia and 1 of esotropia), ptosis (4 cases), iris atrophy (1 case), and cornea edema (1 case). Two patients showed skin necrosis at the glabellar region after hyaluronic acid or autologous fat injection. At the final follow-up, most associated ocular problems improved, including ophthalmoplegia and ptosis; however, 5 patients still had exotropia and 1 patient had iris atrophy. Further, phthisis bulbi developed in Patient 3, which progressed by the final follow-up. Follow-up fundus fluorescein angiography indicated improved choroidal perfusion in all the patients, although retinal arterial perfusion did not improve.

Intra-arterial mechanical and chemical thrombolysis with urokinase was attempted immediately after visual loss in 4 patients, but the ophthalmic arteries were not recanalized and the BCVAs did not improve (initial and final BCVAs: no light perception; P = 1.000). Intraoperative angiography indicated that the ophthalmic arteries were severely occluded by the injected substances ( Figure 1 ). Therefore, these patients had poor visual outcome. The BCVAs (no light perception) of the 7 patients with iatrogenic ophthalmic artery occlusion showed no change during the mean follow-up duration of 14.0 ± 22.1 weeks ( P = 1.000, Wilcoxon signed-rank test).
Central Retinal Artery Occlusion (n = 2)
The initial presentation of iatrogenic central retinal artery occlusion was decreased vision without ocular pain. Patient 8 noted blindness immediately after the glabellar injection, and patient 9 noted blindness 1 day after the injection, which incidentally affected the normal eye. Fundus fluorescein angiography showed no retinal perfusion, but intact choroidal perfusion, in both the patients. No associated initial ocular problems were detected, except for a relative afferent pupillary defect. The initial and final BCVAs of these patients were 3.50 ± 2.12 logMAR units and 2.76 ± 3.17 logMAR units, respectively. One patient (Patient 9) experienced combined brain infarction by fat embolism after autologous fat injection.
Branch Retinal Artery Occlusion (n = 3)
The initial presentation of iatrogenic branch retinal artery occlusion was also decreased vision without ocular pain. All patients had occluded superior branch arteries (2 cases of supero-temporal branch retinal artery occlusion and 1 case of supero-nasal branch retinal artery occlusion) and reported an inferior visual field defect in the affected eye ( Figure 4 ). Fundus fluorescein angiography showed filling defects in the branch retinal arteries and retrograde retinal artery filling ( Figure 4 ). The initial and final BCVAs of these patients were 2.05 ± 3.42 logMAR units and 2.23 ± 3.28 logMAR units, respectively.