Head and Neck Neoplasia
Basic concepts
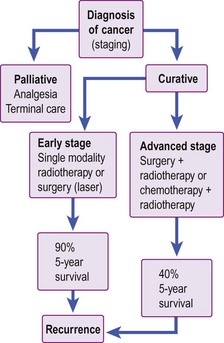
Management of head and neck cancer is dependent on histological diagnosis, staging and grading of the tumour. The patient’s wishes are equally important factors in determining therapy. Some patients may not be fit for aggressive curative treatment and others may refuse treatment. The head and neck oncologist uses surgery, radiotherapy and chemotherapy as treatment modalities. In general, early cancers are treated with single-modality therapy and advanced cancers require combined modality. A treatment algorithm for head and neck cancer is shown in Figure 4.1.
Aetiological factors
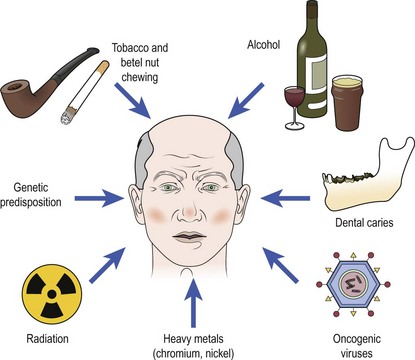
Cancer develops through a complex multifactorial process (Fig. 4.2). The majority of head and neck cancers result from exposure to carcinogens, mainly via tobacco. Chewing tobacco is also carcinogenic and associated with mouth cancer. Alcohol appears to act synergistically with smoking. Betel nut, which is widely chewed in the Indian subcontinent, is a strong carcinogen for mouth cancer, hence the very high incidence of oral cancer in this region. Exposure to ionizing radiation is implicated in thyroid cancer and sarcomas. Oncogenic viruses such as human papilloma virus (HPV) are known to induce tumours in squamous epithelium. HPV is contracted through oral sex and is thought to be the cause of the increase in incidence of oral and oesophageal cancers in younger patients. Epstein–Barr virus (EBV) is associated with nasopharyngeal cancer and Burkitt’s lymphoma. Heavy metals, such as nickel or chromium, and hardwood dust exposure are important occupational carcinogens. Severe chronic dental caries is thought to predispose to mouth cancer.
Premalignant conditions in head and neck cancer
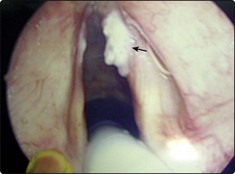
Clinical manifestations of premalignant conditions are leukoplakia (white patch) or erythroplasia (red patch) which may affect the mucosa (Figs 4.3 and 4.4). These often present as superficial lesions and should be biopsied to determine the grade of dysplasia.
Lichen planus
Erosive lichen planus of the oral cavity (Fig. 4.5) may progress to cancer. The common form of lichen planus, which is benign, is located in a symmetrical distribution on the buccal mucosa and tongue. The erosive variety appears in the floor of the mouth. Biopsy is mandatory to identify the type of lichen planus and to distinguish it from leukoplakia.
Principles of treatment
The treatment options in head and neck neoplasia include:
Radiotherapy
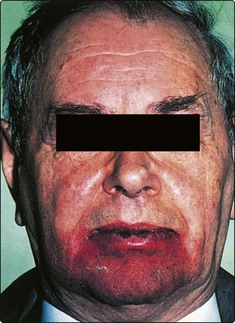
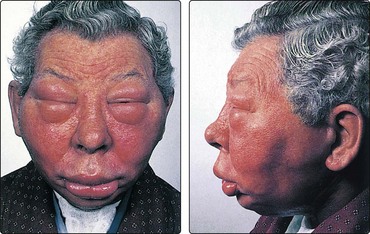
The majority of patients will develop radiation reactions in normal tissue. The skin will invariably show some evidence of treatment (Fig. 4.6). Mucous membrane reactions tend to occur very early, with erythema and ulceration, and may be so severe that nasogastric feeding is required. Fungal infections, particularly by Candida, often compound the mucositis and are not uncommon in the debilitated patient. Prophylactic care with antifungals and anti-inflammatory rinses may be required.
Terminal care
Some patients have no prospect of cure owing to advanced disease or residual or recurrent disease. The dying phase is usually protracted. In order to be able to deal with such situations in a humane manner, the concept of terminal care has evolved. This provides physical and psychological support for patients in the terminal stage of their life (see p. 116).
Basic concepts
 Head and neck malignancy uncommonly produces distant metastases.
Head and neck malignancy uncommonly produces distant metastases.
 Tobacco and alcohol are the major aetiological factors in development of head and neck malignancy.
Tobacco and alcohol are the major aetiological factors in development of head and neck malignancy.
 Any neck mass should only be biopsied after a full examination of the upper air and food passages has been performed to exclude a primary neoplastic process.
Any neck mass should only be biopsied after a full examination of the upper air and food passages has been performed to exclude a primary neoplastic process.
 The use of radiotherapy is limited by sensitivity of the surrounding normal tissues, particularly the lens of the eye and the spinal cord.
The use of radiotherapy is limited by sensitivity of the surrounding normal tissues, particularly the lens of the eye and the spinal cord.
 Severe radiation reactions may necessitate a temporary halt to the course of radiotherapy.
Severe radiation reactions may necessitate a temporary halt to the course of radiotherapy.
 Chemotherapeutic agents appear to enhance the effect of radiotherapy, but their role has not yet been fully evaluated.
Chemotherapeutic agents appear to enhance the effect of radiotherapy, but their role has not yet been fully evaluated.
Neck lumps – introduction
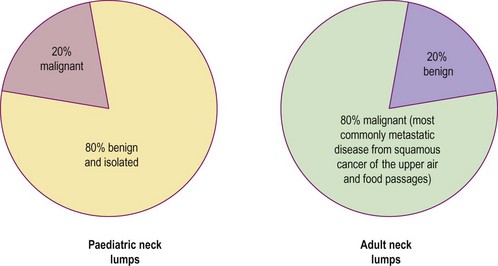
It is useful to consider separately the diagnosis of neck lumps in children and adults. The ‘80 : 20 rule’ applies to malignant and benign causes of neck masses (Fig. 4.7). In the adult it must be remembered that metastatic neck disease may occur from structures below the clavicle (Table 4.1).
Table 4.1 Infraclavicular sites of malignancy that may cause neck lumps by metastatic spread
| Lung | Kidney |
| Breast | Prostate |
| Stomach | Uterus |
| Pancreas |
Clinical history and examination
In addition to a routine history, specific questions must be posed. The ‘20 : 40 rule’ is useful in considering the diagnostic possibilities of a neck lump (Table 4.2).
Table 4.2 The ‘20 : 40 rule’ applied to neck lumps
| Age (years) | Possible causes of neck lump |
|---|---|
| Less than 20 | Inflammatory neck nodes (e.g. due to tonsillitis) |
| Congenital lesions (e.g. thyroglossal cysts, brachial cyst, midline dermoid, cystic hygroma) | |
| Lymphoma | |
| 20–40 | Salivary gland pathology (calculus, infection, tumour) |
| Thyroid pathology (tumour, thyroiditis, goitre, lymphoma) | |
| Chronic infection (tuberculosis, HIV) | |
| Greater than 40 | Primary or secondary malignant disease |
The primary head and neck sites of malignancy may give rise to very specific symptoms including:
Earache may be referred from neoplastic lesions in the upper food passages (see Fig. 1.28, p. 13). Referred otalgia is a poor prognostic sign in head and neck neoplasia.
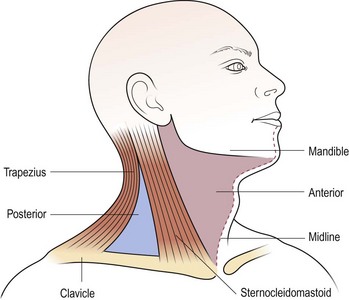
It is important to perform a thorough examination of the head and neck, especially the upper aerodigestive tract, as well as looking for other lumps, e.g. in the liver, spleen or axillae. The scalp should be carefully examined, as a primary malignancy in this site is commonly overlooked as a cause of metastatic neck disease. The precise features of the lump should be noted and, if laterally sited, its position in the triangles of the neck accurately described (Fig. 4.8). This approach is useful as an aid to remembering structures located in the triangles which may give rise to pathology. A mass in the midline is most frequently of thyroid origin. Nasopharyngeal carcinoma may present as unilateral or bilateral metastatic nodes in the posterior triangle of the neck. An isolated mass in the supraclavicular region is likely to be metastatic disease from sites below the clavicle (Table 4.1).
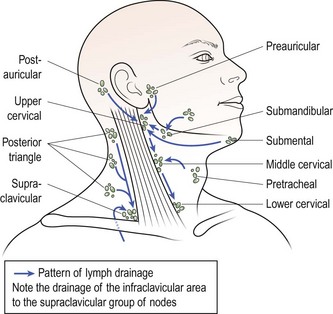
Multiple neck lumps are most likely to be lymph nodes. There are over 100 lymph nodes on each side of the neck, although they tend to be confined to relatively discrete areas rather than evenly distributed (Fig. 4.9).
Investigations
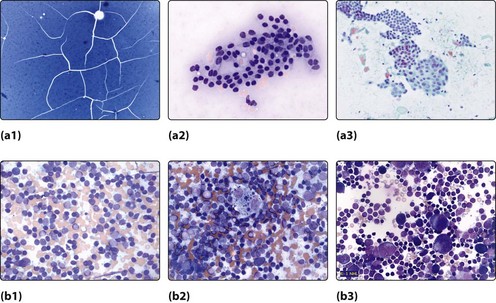
An MDT approach will allow clinical examination, a radiological assessment, usually an ultrasound, followed by Fine Needle Aspiration Cytology (FNAC). The cytologist will then identify the specimen and decide its nature (Fig. 4.10):
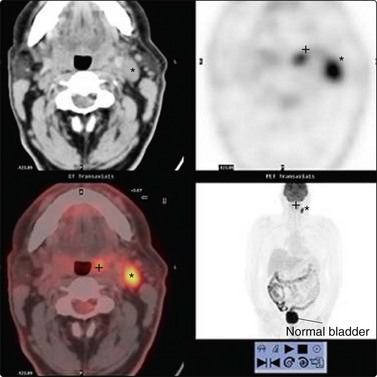
This will direct the management to further and more sophisticated investigations such as CT, MRI or PET scanning (Fig. 4.26, p. 97). In some cases an examination of the upper air and food passages may be required prior to making a definitive diagnosis and formulating a treatment plan.
Biopsy of a neck lump
Neck lumps – introduction
 Never biopsy a neck lump without a prior thorough ENT examination of the upper air and food passages.
Never biopsy a neck lump without a prior thorough ENT examination of the upper air and food passages.
 Remember the 80 : 20 percentage and the 20 : 40 age rules in the diagnosis of neck lumps.
Remember the 80 : 20 percentage and the 20 : 40 age rules in the diagnosis of neck lumps.
 Do not forget infraclavicular sites for metastatic neck lumps, particularly adenocarcinoma.
Do not forget infraclavicular sites for metastatic neck lumps, particularly adenocarcinoma.
 Palpate the salivary and thyroid glands and listen for any overlying vascular bruits.
Palpate the salivary and thyroid glands and listen for any overlying vascular bruits.
 Multiple neck lumps are almost certainly lymph nodes.
Multiple neck lumps are almost certainly lymph nodes.
 Fine-needle aspiration cytology may assist in diagnosis.
Fine-needle aspiration cytology may assist in diagnosis.
 Avoid incisional biopsy of a neck lump; if malignant disease is present there is a risk of implantation.
Avoid incisional biopsy of a neck lump; if malignant disease is present there is a risk of implantation.
 It is normal for children to have easily palpable lymph nodes in the neck.
It is normal for children to have easily palpable lymph nodes in the neck.
 Do not overlook HIV infection as a cause of lymphadenopathy.
Do not overlook HIV infection as a cause of lymphadenopathy.
Neck lumps – paediatric conditions
In the paediatric age group (less than 20 years of age), the majority of neck lumps encountered are benign. They are commonly located anterior to the sternomastoid muscle in the anterior triangle of the neck. An isolated neck lump located in the posterior triangle has a high likelihood of being malignant. The ‘80 : 20 rule’ is useful in assessing the diagnostic possibilities (see Fig. 4.7, p. 90).
Midline neck lumps
Thyroglossal cyst
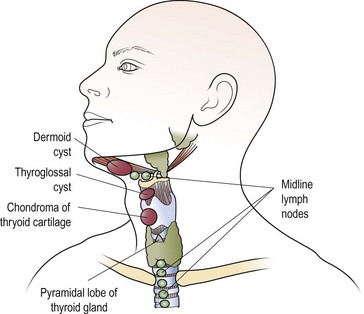
The most common midline mass (Fig. 4.11) in children is a congenital cyst of the thyroglossal duct. Embryologically, the cyst can arise at any site along the route of the thyroglossal duct, extending from the tongue (foramen caecum) to the thyroid gland.
The thyroglossal cyst is most commonly located below the hyoid bone, and moves on both swallowing and tongue protrusion (Figs 4.11 and 4.12). Most cysts are asymptomatic, apart from the presence of a lump, but infection will be associated with pain and swelling. Treatment is by excision, which should include the central portion of the body of the hyoid bone to prevent recurrences. A wedge of tongue muscle is resected with the thyroglossal duct behind the hyoid.
Lateral neck lumps (Table 4.3)
Inflammatory conditions
Table 4.3 Causes of lateral neck lumps in children
| Infective | Cervical lymphadenitis |
| Mumps | |
| Tuberculosis | |
| Congenital | Branchial cysts |
| Chemodectoma | |
| Cystic hygroma | |
| Haemangioma | |
| Neoplastic | |
| Primary | Lymphoma |
| Neuroblastoma | |
| Parotid malignancy | |
| Rhabdomyosarcoma | |
| Secondary | Metastases – nasopharyngeal |
Mumps
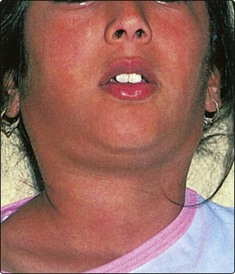
Enlargement of the parotid glands, due to the mumps virus, is extremely common. It is usually a bilateral disease, but unilateral cases can occur (Fig. 4.13). The child has constitutional symptoms of malaise and pyrexia. Rare cases may be complicated by orchitis and encephalitis. Treatment is symptomatic.
Tuberculosis
Tuberculosis of the cervical lymph nodes is uncommon. Tuberculous nodes are multiple and coalesce, and may form a discharging sinus (Fig. 4.14). Most cases have associated pulmonary tuberculosis. Node biopsy is sometimes required for histological confirmation of diagnosis. Treatment is by combination chemotherapy.
Congenital conditions
Most solitary lateral neck masses in the paediatric age group are congenital in origin.
Branchial arch cysts
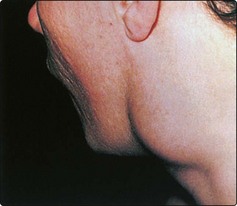
Branchial arch anomalies giving rise to branchial cysts are uncommon. First branchial arch cysts are rare and located anterior to the tragus. True branchial cysts are more frequently encountered and invariably located in the anterior triangle just in front of the sternomastoid (Fig. 4.15). The aetiology is believed to be cystic degeneration in a lymph node. Most of these cysts are lined by lymphoid tissue so that pain and swelling may be experienced with upper respiratory infections. Where a second arch fistula is present a tract may extend to the pharynx, and this must be excised together with the cyst. All brachial arch cysts presenting in patients over 40 years of age should be considered as a possible undiagnosed squamous cell carcinoma.
Cystic hygromas
Cystic hygromas are anomalies of the lymph channels and present as lateral neck swellings. They are soft and irregular, and usually present at birth (Fig. 4.16). Typically, the hygroma enlarges during crying and the Valsalva manoeuvre. They transilluminate brilliantly. Most cystic hygromas have to be removed owing to continued enlargement, particularly as they may encroach onto the major airways. Excision is difficult, as this benign lesion encompasses structures such as the carotid arteries and facial nerve.
Neoplasia
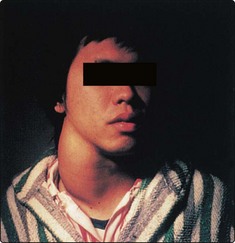
Lymphoma of the Hodgkin’s variety is common. It may present as a unilateral isolated lump in the neck (Fig. 4.17). After histological confirmation, a full evaluation will be required to stage the disease. Treatment is usually radiotherapy in localized disease and chemotherapy with drug combinations in systemic lymphoma.
Rarer primary neoplasia include malignant parotid disease, rhabdomyosarcomas and neuroblastomas.
Neck lumps – paediatric conditions
 80% of neck lumps in children are benign and are located in the anterior triangle of the neck.
80% of neck lumps in children are benign and are located in the anterior triangle of the neck.
 20% of neck lumps in children are malignant and are usually located in the posterior triangle of the neck.
20% of neck lumps in children are malignant and are usually located in the posterior triangle of the neck.
 The most common midline lump in children is the thyroglossal cyst. It moves on swallowing and with tongue protrusion.
The most common midline lump in children is the thyroglossal cyst. It moves on swallowing and with tongue protrusion.
 The most common cause of multiple lateral neck lumps in children is cervical lymphadenopathy secondary to infection.
The most common cause of multiple lateral neck lumps in children is cervical lymphadenopathy secondary to infection.
 The most common isolated lateral neck lump in children is the branchial cyst.
The most common isolated lateral neck lump in children is the branchial cyst.
Neck lumps – adult conditions
Midline neck lumps
Thyroid masses
It is important to determine whether there is a goitre (diffuse bilateral thyroid enlargement) or a nodular (single) mass within the thyroid (Figs 4.18 and 4.19). Symptoms and signs of hyper- (overactive) and hypo- (underactive) thyroid disease should be sought (Table 4.4). Clinical examination should determine the size and nature of the thyroid mass. Thyroid enlargement may result in compression of either the trachea, causing stridor, or oesophagus, causing dysphagia. Common disorders to affect the thyroid gland include thyroiditis, multinodular goitre, follicular adenoma, thyroid carcinoma and lymphoma.
Table 4.4 Symptoms and signs of thyroid disease
| Disease | Symptoms | Signs |
|---|---|---|
| Hyperthyroidism | Palpitations | Tachycardia (AF) |
| Weight loss | Exophthalmos | |
| Agitation | Tremor | |
| Sweating | ||
| Hypothyroidism | Tiredness | Bradycardia |
| Weight gain | Loss of eyebrow hair | |
| Poor concentration |
Investigations
Blood tests should determine thyroid status; a thyroid-stimulating hormone (TSH) test is the first-line investigation. Autoimmune thyroid antibodies should be measured along with thyroglobulin. FNAC should be undertaken to determine the cellular nature of any thyroid nodule. Ultrasound scanning is the first imaging of choice; it will determine whether the thyroid swelling is cystic or solid and will demonstrate whether multiple nodules are present. Ultrasound and FNAC can be combined to increase diagnostic yield. CT scanning is only indicated when tracheal compression or retrosternal extension is suspected (Fig. 4.20).
Lateral neck lumps
Neoplasia
Any neck lump appearing for the first time in an adult over 40 years of age should be treated as metastatic cancer until proven otherwise (Table 4.5). Secondary neck disease from malignancy in the upper aerodigestive tract is very common. The patient frequently gives a long history of alcohol and tobacco abuse. The possibility of a supraclavicular neck mass being metastatic disease from sites below the clavicle should not be overlooked (see Table 4.1, p. 90).
Table 4.5 Causes of a lateral neck lump in adults
| Type | Condition |
|---|---|
| Neoplasia | Primary cancer |
| Lymphoma | |
| Neurogenic (schwannoma, chemodectoma) | |
| Metastatic cancer | |
| Lymph-node metastasis from head and neck sites | |
| Infection | Glandular fever |
| HIV | |
| Tuberculosis | |
| Parotitis (mumps) | |
| Autoimmune | Sjögren’s syndrome |
| Miscellaneous | Sarcoidosis |
| Branchial cyst | |
| Normal variants | Transverse process of 2nd cervical vertebra (C2) |
| Elongated styloid process | |
| Normal or cervical rib | |
| Tortuous, atherosclerotic carotid artery |
Unilateral painless parotid masses are likely to be neoplastic, the most common lesion being the benign pleomorphic adenoma. Malignant parotid tumours may cause pain and facial weakness owing to involvement of the facial nerve (p. 113). Hodgkin’s and non-Hodgkin’s lymphoma may initially present as an isolated lateral neck lump. However, disease progression leads to multiple matted neck lumps.
Inflammatory conditions
Acute parotitis, either bacterial or viral, may cause neck swelling (Fig. 4.21). The diagnosis is usually straightforward, provided the full anatomical extent of the parotid is appreciated, including the deep lobe which may enlarge into the oropharynx. An infection of the parapharyngeal space of the neck, usually from dental or oropharyngeal infections, may produce a significant neck swelling in association with a mass in the throat (Fig. 4.22).
Miscellaneous lateral lumps
HIV infection
The primary infection with HIV may produce prodromal symptoms similar to glandular fever (p. 86). Persistent lymphadenopathy syndrome (PLS) is seen in the chronic stage of infection with HIV, with lymph nodes in the neck being commonly enlarged. HIV infection may also present as a cystic swelling in the parotid gland, a ‘lymphoepithelial cyst’.
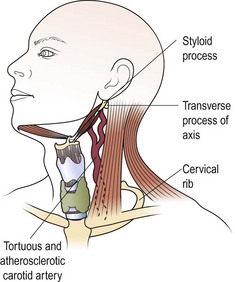
Normal variants
Certain normal bony and cartilaginous structures in the neck may be palpable in some patients and mistaken for lumps (Fig. 4.23). The lateral process of the axis (C2) is often palpable and tender if slight pressure is applied. These features may only be demonstrated on one side of the neck. The styloid process may be elongated and ossified, and therefore palpable as it runs just anterior from the mastoid to the mandible. Normal ribs and, occasionally, an asymptomatic cervical rib may be palpated deep in the supraclavicular fossa. A tortuous atherosclerotic carotid artery in a thin elderly person may be mistaken for a neck mass. It may not be pulsatile, but a bruit is usually audible on auscultation.
Neck lumps – adult conditions
 Thyroid lesions are the most common cause of midline lumps in adults.
Thyroid lesions are the most common cause of midline lumps in adults.
 The most common lateral neck lump in adults is metastatic malignant disease, usually squamous cell carcinoma from a primary site in the head and neck.
The most common lateral neck lump in adults is metastatic malignant disease, usually squamous cell carcinoma from a primary site in the head and neck.
 The symptoms and signs of acute infection with HIV mimic the clinical features of glandular fever.
The symptoms and signs of acute infection with HIV mimic the clinical features of glandular fever.
Neck lumps – management of malignant lumps
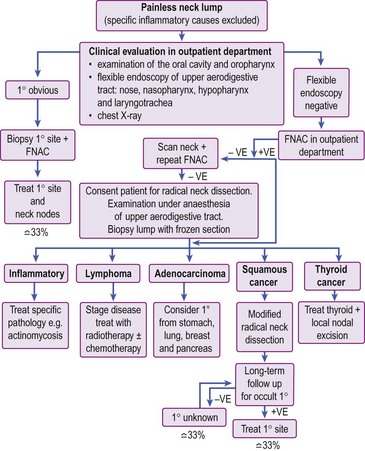
The general management of such patients is outlined in Figure 4.24. A full ear, nose and throat (ENT) evaluation will include inspection, radiology and possible biopsy of primary sites in the head and neck. If the primary sites are clear, FNAC may assist in the diagnosis. Otherwise, the mass must be biopsied by excision as incisional biopsies carry the risk of implantation of malignant cells in skin.
Metastatic cervical nodes
Metastatic cervical nodes are clinically assessed and then classified according to the UICC/AJC criteria (Table 4.6). Since the classification is clinically based, it is subject to observer variation. It is also not feasible to decide whether a palpable node contains metastatic cancer or is merely enlarged due to infection. The implication in the classification is that prognosis deteriorates from N1 through to N3 stages. More recently, it appears that the level of metastatic disease in the neck is a better prognostic indicator. Inferiorly placed neck disease has the worst prognosis, with supraclavicular node involvement having the least favourable 5-year survival.
Table 4.6 Classification of regional lymph nodes affected by metastatic carcinoma
| Classification (UICC/AJC) | Clinical assessment |
|---|---|
| N0 | No regional nodes palpable |
| N1 | Mobile ipsilateral nodes |
| N2 | Mobile contralateral or bilateral nodes |
| N3 | Fixed nodes |
UICC: International Union Against Cancer; AJC: American Joint Committee for Cancer Staging.
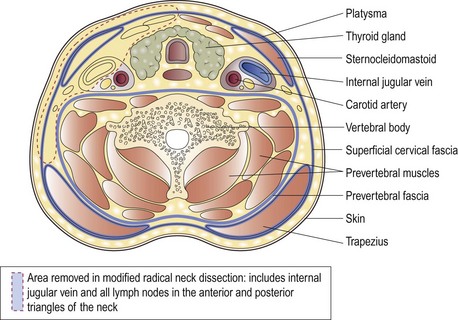
The treatment of metastatic cervical nodes depends to a large degree on whether the primary disease in the head or neck, or in distant sites, has been identified. As a rule, surgery in the form of a modified radical neck dissection is advocated for metastatic neck disease (Fig. 4.25). Radiotherapy may be employed in occult and small nodal metastases, and in palliation of fungating lesions.
N0: clinically negative neck nodes
Impalpable lymph nodes involved in metastatic disease are called occult nodes. There are certain sites in the head and neck, with a rich and frequently decussating lymphatic supply, from which metastatic nodal disease is highly probable (Table 4.7). Although it would be logical therefore to consider performing an elective modified radical neck dissection in occult neck disease, such a policy shows little benefit. It appears that in selected patients, prophylactic radiotherapy markedly diminishes the incidence of recurrent neck disease with little increase in morbidity.
Table 4.7 Sites of primary carcinoma with a high incidence of occult nodes
N1: palpable ipsilateral neck nodes
N1 metastatic disease is subclassified into whether the primary site is known or unknown.
N1 with no known primary site (occult primary)
The histological appearance of the lymph node may give a clue to where the primary malignant site may be located (Table 4.8). Metastatic supraclavicular nodes are likely to have been involved from infraclavicular primary malignant sites.
Table 4.8 The occult primary: how the histology of a malignant node may assist in determining the primary site
| Histology of metastatic neck node | Probable primary malignant sites |
|---|---|
| Squamous cell carcinoma | Head and neck sites: nasopharynx, tonsil, tongue base, supraglottic larynx, floor of mouth, piriform fossa, postcricoid region |
| Adenocarcinoma | Infraclavicular sites: bronchus, stomach, breast, intestine, kidney, prostate, uterus |
| Head and neck sites: ethmoid sinuses and thyroid gland | |
| Undifferentiated or anaplastic carcinoma | Exclude lymphoma by immunocytochemistry |
| Consider the above sites of carcinoma |
The occult primary in the head and neck is a rare entity. However, if after thorough clinical examination the primary lesion cannot be identified, positron emission tomography (PET) scanning can be useful in identifying the site (Fig. 4.26).
N2: bilateral neck nodes
The appearance of bilateral malignant metastatic neck nodes is a very poor prognostic sign. Such an event is more likely in primary tumours of the tongue base and hypopharynx. Serious thought should be given as to whether such patients require active treatment or active palliation. It is feasible to perform bilateral neck dissection as a single rather than staged procedure, preserving one jugular vein. Tying a single internal jugular vein results in a rise in intracranial pressure which is raised even further on tying the second side (Fig. 4.27). Morbidity and mortality related to the huge increase in intracranial pressure may be prevented by modification of the classic radical dissection, and drug intervention.