Giant Breaks
 Giant retinal breaks are traditionally defined as breaks extending for greater than 90 degrees. Because of the propensity of the retina to fold over, surgical management of these detachments was very difficult until the advent of vitrectomy and intraocular gas. The next major advance occurred when Chang initiated the application of perfluorocarbon (PFO) liquids to giant break surgery (1). It is now relatively straightforward to achieve surgical success in most cases. The long-term success rate is determined by the incidence of proliferative vitreoretinopathy (PVR). Although vitreous dynamics, trauma, and hereditary peripheral retinal changes play a role, the exact pathogenesis of giant breaks remains unclear. The high incidence of associated PVR presumably relates to the exposure of vast areas of retinal pigment epithelium (RPE) and retinal glial cells to the vitreous matrix. RPE cells migrate along the vitreous and retinal surfaces. The exposed edge of retina presumably enables glial cells to migrate to the retinal surface as well. Vitreous is virtually never observed on the photoreceptor side of the retina in these cases. Inward folding of the retina is caused by hypocellular contraction of the vitreous, the inherent elasticity of the internal limiting membrane (ILM), and PVR. Although one can occasionally distinguish between giant breaks and giant disinsertions, this differentiation does not seem to play a role in management strategies or prognosis.
Giant retinal breaks are traditionally defined as breaks extending for greater than 90 degrees. Because of the propensity of the retina to fold over, surgical management of these detachments was very difficult until the advent of vitrectomy and intraocular gas. The next major advance occurred when Chang initiated the application of perfluorocarbon (PFO) liquids to giant break surgery (1). It is now relatively straightforward to achieve surgical success in most cases. The long-term success rate is determined by the incidence of proliferative vitreoretinopathy (PVR). Although vitreous dynamics, trauma, and hereditary peripheral retinal changes play a role, the exact pathogenesis of giant breaks remains unclear. The high incidence of associated PVR presumably relates to the exposure of vast areas of retinal pigment epithelium (RPE) and retinal glial cells to the vitreous matrix. RPE cells migrate along the vitreous and retinal surfaces. The exposed edge of retina presumably enables glial cells to migrate to the retinal surface as well. Vitreous is virtually never observed on the photoreceptor side of the retina in these cases. Inward folding of the retina is caused by hypocellular contraction of the vitreous, the inherent elasticity of the internal limiting membrane (ILM), and PVR. Although one can occasionally distinguish between giant breaks and giant disinsertions, this differentiation does not seem to play a role in management strategies or prognosis.CASE SELECTION
Quadrantic giant breaks can rarely be managed effectively with scleral buckling alone if there is minimal folding of the retina. Mild degrees of folding can be managed by adding expanding C3F8 gas to the scleral buckling modality. Most giant breaks with retinal folding are best managed with vitrectomy and PFO liquids. Giant breaks combined with PVR, vitreous to a wound, dislocated lenses, or vitreous hemorrhage are absolute indications for vitrectomy, regardless of the size of the break.
SURGICAL SEQUENCE AND TECHNIQUES
Patient Education
Patients should be psychologically prepared for 1 to 3 weeks in the face-down position after surgery, unless medium-term PFO liquids (2-3 weeks) are used instead of gas. Patients treated with silicone oil must be positioned as well if the break extends below the horizontal meridian.
Incisions
The authors use 25-gauge vitrectomy, laser, internal drainage of subretinal fluid (SRF), and air-silicone exchange (ASX) or air-gas exchange (AGX) in all giant break cases. Intraoperative use of perfluoron (PFO) allows adequate repositioning of the folded retina in large retinal tears. Medium-term PFO prevents slippage of the giant break but requires two procedures and cannot be used for superior giant breaks. The patient must lie on his or her side for nasal or temporal breaks and be seated, standing, or semireclining for inferior breaks with the medium-term PFO technique.
Management of the Lens
Phaco-vit and IOL insertion should be used if there is significant cataract preventing sufficient visualization. In the past, giant retinal tears were considered indications for pars plana lensectomy, but the authors do not find a need for lensectomy at this time with modern vitrectomy techniques.
Vitrectomy
Vitreous removal should be performed using very low suction force with proportional suction control and high cutting rates (5,000 cuts per minute) because of marked retinal
mobility. The vitreous is very rarely attached to the posterior edge of the giant break. The authors use 25-gauge technique for all giant break cases because the greater fluidic stability makes removal of vitreous near the highly mobile retina much safer.
mobility. The vitreous is very rarely attached to the posterior edge of the giant break. The authors use 25-gauge technique for all giant break cases because the greater fluidic stability makes removal of vitreous near the highly mobile retina much safer.
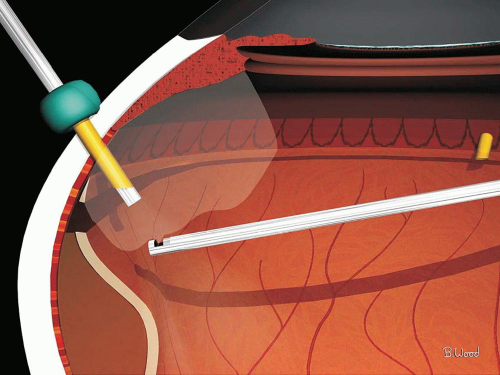
The vitreous must be trimmed to the anterior retinal surface and away from the anterior flap to prevent vitreous entrapment in the SRF drainage cannula and to prevent late vitreous traction from causing redetachment (Fig. 15.1). It is better to remove the detached nonpigmented pars plana epithelium anterior to the break during removal of the peripheral vitreous.
Fluid-Air-Gas Exchange
Internal drainage of SRF and fluid-air exchange can be performed without PFO liquids in selected cases with smaller breaks and little or no folding. Internal drainage of SRF must precede fluid-air exchange and continue during the exchange. A soft-tip extrusion cannula should be positioned just anterior to the edge of the giant break. The retina will be gently pulled into position as the SRF is drained. Rotating the eye toward the giant break enables drainage of the vitreous fluid simultaneous with the SRF and facilitates complete drainage of SRF and better repositioning of the retina.
Perfluorocarbon Liquids
PFO liquids permit removal of all SRF and position the retina in a nonfolded state near its original position, permitting laser retinopexy to both the retina and the RPE. PFO liquids are surface tension management agents similar to silicone oil, air, and gas. Silicone and gas float because their density is less than infusion fluid. PFO liquids are denser than infusion fluid and retina and migrate to the lowest part of the eye. Retina is less dense than PFO liquids and therefore floats to its original position, limited only by vitreoretinal traction and its inherent stiffness. Similarly, SRF is less dense than PFO liquids and floats up through the giant break and into the anterior vitreous cavity. The authors use PFO from Alcon for all cases.
PFO liquid should be injected on the anterior side of the retina (Fig. 15.2), near the optic nerve with a MedOne dual-bore 25-gauge viscous fluid injection cannula. Because the endoilluminator is plugging one sclerotomy and both PFO and balanced salt solution (BSS) are incompressible, BSS Plus must be allowed to egress through the dual-port cannula to prevent increasing the intraocular pressure. The PFO should be injected until the retina is unfolded and all SRF is gone. PFO must reach the pars plana when injection is complete and all SRF is gone (Fig. 15.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree