In 1951, Dr. Lars Leksell from Sweden conceived of what is now known as gamma knife radiosurgery (GKRS). Since Leksell first treated a patient who had a vestibular schwannoma in 1967, there has been a year-to-year increase in the number of patients treated with the gamma knife for vestibular schwannoma. This article outlines the technique of GKRS and discusses the current results of its use to treat vestibular schwannomas. Other topics discussed include tumor control, treatment of recurrent/residual and cystic vestibular schwannomas, and the results of treatment of neurofibromatosis type 2.
In 1951, Dr. Lars Leksell from Sweden conceived of what is now known as gamma knife radiosurgery (GKRS). The Leksell Gamma Knife (Elekta, Norcross, Georgia) uses a focused array of 201 intersecting beams of cobalt-60 gamma radiation to treat lesions within the brain. The gamma knife is so named because of its accuracy in delivering an exact field of radiation to the target. The combined intensity of radiation at the focus (or isocenter) is extremely high whereas the intensity only a short distance from the isocenter is very low. This enables a high dose of radiation to be delivered to the lesion while sparing the adjacent healthy brain tissue.
Leksell first used the gamma knife in 1969 to treat a patient who had a vestibular schwannoma. Gamma knife radiosurgery has grown considerably in the United States since the first gamma knife unit was installed in North America at the University of Pittsburgh in 1987. Currently, there are more than 50 gamma knife centers in the United States and 249 centers worldwide. Based on a worldwide survey in December 2006 by the Leksell Gamma Knife Society, 397,672 lesions have been treated with GKRS since the introduction of the gamma knife (202 of 249 gamma knife centers reporting). Slightly more than 9% (36,180) of the lesions treated were vestibular schwannomas. A similar survey in December 2004 by the Leksell Gamma Knife Society reported 28,306 cases of patients who had vestibular schwannoma had been treated worldwide (181 out of 213 centers reporting).
Based on these data, it seems that there is a steady, growing demand for GKRS as treatment of vestibular schwannomas. This may be due, in part, to improved patient outcomes and an expanding body of knowledge of long-term tumor control. Prior to 1992 high doses (typically 16 Gy or greater to the tumor margin) resulted in significant rates of facial weakness (21%) and facial numbness (27%) after GKRS. Since then, dose reduction (typically 12–13 Gy to the tumor margin), the introduction of MRI scans, and more sophisticated dose planning software and equipment have improved outcomes considerably. This article outlines the technique of GKRS and discusses the current results of the use of this technique to treat vestibular schwannomas using marginal doses of 12 to 13 Gy or less.
Stereotaxy
The aim of the stereotactic technique as it pertains to the gamma knife is to relate the location of structures or lesions within the boundaries of a head frame to a 3-D Cartesian axis system. This is done initially by fixing a rigid titanium head frame to the head ( Fig. 1 ). The borders of the frame then constitute the Cartesian axes, whereas the cranium serves as a platform to support the frame. The way in which a point within the frame is defined in terms of the Cartesian axes is depicted in Fig. 2 . By convention, the X axis runs from side to side, the Y axis runs from behind forwards, and the Z axis runs from above downwards. The common zero point is above and behind the right ear. It is the frame and not the head that is used to localize. This is helpful because there may be times when it is necessary to place the frame eccentrically or to rotate the frame with respect to the head.


Reference points relative to the titanium head frame must be visible on radiographic imaging. This is accomplished by means of plastic plates that are attached to each side of the head frame. Embedded in the walls of the plastic plates are three metal rods or strips (CT), or three hollow channels filled with a copper-containing liquid (MRI). These rods or channels are radiopaque, creating fiducial lines. Of the three rods or channels, two are parallel and vertical. The third rod or channel is oriented at a 45° angle to the other two. This creates three fiducial lines in the configuration of a backwards “N”. In this way, on each image slice, three sets of dots are identifiable ( Fig. 3 ). As one moves through an imaging set, only the middle dot moves sequentially. Determination of the separation of the two fixed dots in relation to the moving middle dot makes calculation of the Z coordinate for each slice a simple geometric exercise. Thus, a stereotactic space is created.

The gamma knife machine
There have been several generations of the Leksell Gamma Knife machine. The Leksell Gamma Knife 4B and 4C models are the machines used most commonly at present. The basic construction of the model 4 is described here.
The Leksell Gamma Knife 4C unit ( Fig. 4 ) consists of a thick-cast, hemispheric steel shell containing a dome-shaped core of 201 cylindric cobalt-60 sources, each 1 mm in diameter and 20 mm in length. These sources are radially aligned toward a common focal point. The steel shell is equipped with two thick mechanical doors through which the head of the patient is introduced. Each cobalt-60 source undergoes a primary collimation within the casting. A second collimation is performed through a helmet in which the patient’s head is positioned. The collimator helmet bears 201 collimators that are designed to align with the corresponding primary collimator. The collimator helmet is fixed to a movable bed on which the patient lies. With the patient’s head in the Leksell head frame, the head frame is likewise fixed to the bed. The frame is placed inside the concavity of the collimator helmet so that the targeted lesion is at the center of the helmet. When the primary collimator and the collimator helmet are aligned, it is possible for the gamma rays to converge on the target.
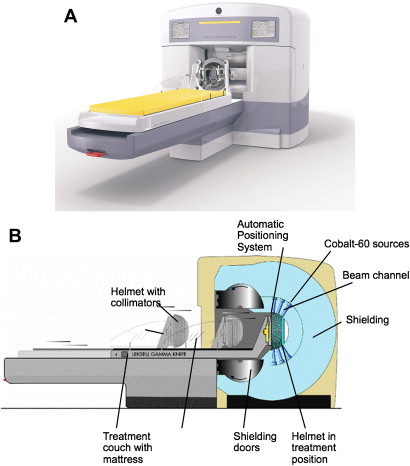
Four collimator helmet sizes are available corresponding to different aperture sizes (4, 8, 14, and 18 mm). Helmet sizes are chosen based on the prescribed treatment plan (discussed later). More than one size of helmet may be used throughout the course of a treatment.
The only movements in the Leksell Gamma Knife system are that of the bed, which draws patients in and out, and that of the doors at the mouth of the machine, which open prior to movement of the bed. When the treatment is over, the bed automatically moves out and the doors close.
The gamma knife machine
There have been several generations of the Leksell Gamma Knife machine. The Leksell Gamma Knife 4B and 4C models are the machines used most commonly at present. The basic construction of the model 4 is described here.
The Leksell Gamma Knife 4C unit ( Fig. 4 ) consists of a thick-cast, hemispheric steel shell containing a dome-shaped core of 201 cylindric cobalt-60 sources, each 1 mm in diameter and 20 mm in length. These sources are radially aligned toward a common focal point. The steel shell is equipped with two thick mechanical doors through which the head of the patient is introduced. Each cobalt-60 source undergoes a primary collimation within the casting. A second collimation is performed through a helmet in which the patient’s head is positioned. The collimator helmet bears 201 collimators that are designed to align with the corresponding primary collimator. The collimator helmet is fixed to a movable bed on which the patient lies. With the patient’s head in the Leksell head frame, the head frame is likewise fixed to the bed. The frame is placed inside the concavity of the collimator helmet so that the targeted lesion is at the center of the helmet. When the primary collimator and the collimator helmet are aligned, it is possible for the gamma rays to converge on the target.
Four collimator helmet sizes are available corresponding to different aperture sizes (4, 8, 14, and 18 mm). Helmet sizes are chosen based on the prescribed treatment plan (discussed later). More than one size of helmet may be used throughout the course of a treatment.
The only movements in the Leksell Gamma Knife system are that of the bed, which draws patients in and out, and that of the doors at the mouth of the machine, which open prior to movement of the bed. When the treatment is over, the bed automatically moves out and the doors close.
Indications/treatment goals
The goals of any form of treatment for vestibular schwannoma should be long-term tumor control, preservation of cranial nerve function, and maintenance of a high quality of life. The aim of any form of treatment for vestibular schwannoma is to prevent the functional consequences due to growth of the untreated tumor rather than improvement of preoperative symptoms. GKRS attempts to achieve this goal by stopping tumor growth. With this in mind, the indications for GKRS have expanded over the years as more centers have gained experience with this technique. Common indications for GKRS for vestibular schwannoma are listed in Table 1 . It is recommended that patients who have tumors larger than 3 cm in diameter not undergo GKRS because of the high probability of radiation damage that may occur to the surrounding brainstem. In addition, patients who have signs of intracranial hypertension or brainstem compression should not undergo GKRS. These patients need rapid decompression of their tumor and for this reason require microsurgical removal.
| 1. Small- to medium-sized tumor (tumor <3 cm in maximum diameter) |
| 2. Elderly/medically infirm patient |
| 3. Recurrent/residual tumor |
| 4. Patient choice |
Technique
Pre-gamma Knife Evaluation
Prior to undergoing GKRS, patients are evaluated with a thorough neurotologic history and physical examination, high-resolution MRI with gadolinium, and audiometric evaluation to include pure-tone air/bone and word recognition score testing. Hearing is graded with the American Academy of Otolaryngology–Head and Neck Surgery 1995 guidelines or the Gardner-Robertson classification system ( Table 2 ). Facial nerve function is assessed most commonly using the House-Brackmann (H-B) grading system.
| Class | Pure Tone Average (dB) | Speech Discrimination (%) |
|---|---|---|
| 1—Good | 0–30 | 70–100 |
| 2—Serviceable | 31–50 | 50–69 |
| 3—Nonserviceable | 50–90 | 5–49 |
| 4—Poor | 91 maximum | 1–4 |
| 5—None | Nontestable | 0 |
After the initial evaluation, gamma knife treatment consists of four main steps: (1) placement of a head frame; (2) an imaging study; (3) treatment/dose planning; and (4) radiation delivery.
Several specialists are typically involved in the gamma knife treatment process. These specialties include a radiation oncologist, a physicist, and a neurosurgeon or neurotologist. Most commonly, the neurosurgeon or neurotologist places the head frame while three specialists—a radiation oncologist, physicist, and neurosurgeon or neurotologist—all are involved in the treatment planning.
Placement of Head Frame/Imaging Study
The gamma knife procedure begins with a patient’s head undergoing rigid fixation in an MRI-compatible Leksell stereotactic head frame. Fixation is performed with various size pins in a bifrontal and bicoronal fashion after application of a local anesthetic. An oral sedative often is given prior to placement of the head frame. The frame is placed in an attempt to locate the tumor as close to the center of the frame as possible. This ensures proper positioning of the head frame and the targeted lesion in or near the center of the collimator helmet.
Plastic plates with radiopaque lines for fiducial marking are attached to the head frame. High-resolution MRI then are obtained after double-dose gadolinium is given. Double-dose gadolinium is given to maximize contrast between tumor and surrounding tissue. Volume acquisition studies require 1- to 1.5-mm axial slice thicknesses that subsequently are reformatted in coronal and sagittal projections. At the author’s treating facility, T1 and T2 constructive interference in steady state magnetic resonance sequences are obtained. The T1 images define the tumor margins whereas the constructive interference in steady state sequences help to define cranial nerves.
Treatment Planning/Radiation Delivery
The imaging study is downloaded into the treatment software in order to begin treatment planning. The goal of GKRS treatment planning is to provide the maximum, safe amount of radiation to a tumor without damaging surrounding structures. Typical parameters considered by a gamma knife team are the number and position of isocenters, their collimator sizes, their relative weights, and the prescription isodose. The plan of radiation delivery is designed to closely adhere, or conform, to the shape of the tumor with a sharp falloff of radiation at the edge of the tumor. A high degree of conformity of the prescription isodose to the target volume, while ensuring that tumor is completely encompassed, is one of the prerequisites for complication-free lesion control with good tumor control. These parameters and goals are described more fully later.
The center of the radiosurgery beam is called the isocenter. Treatment planning consists of placing these beams, or shots, over the target volume. The isocenter radiation distribution tends to be circular or elliptic in shape. A typical radiosurgical treatment can be conceived of as trying to fill an irregular-shaped volume (the tumor) with “balls” of different sizes. Thus, the Leksell Gamma Knife has 4-, 8-, 14-, and 18-mm “balls” (corresponding to the different-sized collimator helmets) with which dose plans can be created. The goal is to maximally fill the treatment volume with these shots. Because most tumors are not truly spherical, the dose from a single beam of radiation will not match the shape of the tumor. By overlapping multiple isocenters of varying sizes, the dose distribution can be fashioned to produce a conformal treatment plan. The “weight” of each isocenter can be adjusted, if necessary, to further conform to the tumor volume.
The amount of radiation given is called the prescribed isodose. The distribution of the isodose around the tumor can be demonstrated visually through circumferential lines that extend outward from the target. These lines are the isodose curves (or isodose lines) of radiation distribution ( Fig. 5 ). The isodose lines are expressed in percentages. Assuming the center, or near center, of the target receives 100% radiation, the isodose lines are constructed with a 10% decrement: 90%, 80%, 70%, and so forth.
The prescription isodose is defined most commonly as the amount of radiation delivered to the 50% isodose line. Most gamma knife plans prescribe the 50% isodose to the margin of the tumor. This is because there is a steep falloff in radiation dosage at the edge of the 50% isodose line, which ensures radiation sparing of surrounding structures. Gamma knife prescription isodoses typically are 12 to 13 Gy to the margin of the tumor. This also may be expressed as 12 to 13 Gy prescribed to the 50% isodose line.
Factors taken into account when determining a prescription isodose include the size and location of the tumor, the hearing level, and the tumor status (primary versus recurrent/residual). In general, 12 Gy is given when the tumor of medium size or the hearing is serviceable. When the tumor is small, the hearing is nonserviceable, and the tumor is recurrent/residual, 13 Gy is typically considered.
Finally, the gamma knife planning software is capable of mapping the location of the maximal dose, or hot spot, in the stereotactic space. A gamma knife team attempts to keep the hot spot well away from the facial nerve and, if necessary, the cochlear nerve.
Using the Leksell Gamma Knife 4C unit, the actual time of radiation delivery varies from approximately 45 to 120 minutes. At the conclusion of the procedure, the head frame is removed and patients receive intravenous steroids (typically 40 mg methylprednisolone). Patients are observed for a short period and are discharged the same day unless immediate complications (rare) develop, such as vomiting, dizziness or headache.
Follow-up
Patients are followed with serial contrast-enhanced MRI studies, which typically are obtained at 6 months, 12 months, 2 years, 4 years, 8 years, and 16 years. Initial radiographic follow-up often demonstrates loss of central enhancement along with slight tumor enlargement and capsular thickening. Audiometric testing is performed at the time of their MRI follow-up for patients who have preserved hearing. Patients typically return to their pretreatment level of functioning or employment within 3 to 10 days post treatment.
Results/complications
Tumor Control
Currently there is no consensus as to the definition of tumor control after radiosurgery. One nonstandardized means to describe tumor control is tumor shrinkage or no tumor growth, also known as radiologic control. A widely accepted definition of tumor growth is that of Flickinger and colleagues, who describe tumor growth as a 1-mm increase in tumor diameter in any two directions or 2-mm in one direction. Another definition of growth is a greater than 10% increase in tumor volume whereas another is an increase of 100% of the initial volume at 2 years post treatment.
Clinical, rather than radiologic, tumor control is another means of defining the outcome of GKRS. Clinical tumor control means, “the absence of the need for further microsurgical or radiosurgical intervention.” Patients who require microsurgical or radiosurgical treatment after radiosurgery are patients who have documented progression of tumor growth or worsening symptoms, such as ataxia.
Tumor expansion after vestibular schwannoma radiosurgery does not necessarily mean a lack of tumor control, however. Transient tumor swelling occurs in as many as 80% of cases after GKRS. The swelling typically peaks between 6 to 7 months but may continue for 1 to 3 years after treatment. In one study, the mean increase in tumor volume was 120% of the initial tumor volume. Pollock and Myrseth and colleagues have noted that some schwannomas may enlarge after GKRS and continue to remain stable in size. In a study by Pollock, 8 of 28 (29%) of tumors enlarged after GKRS and remained stable in size for a maximum follow-up period of 8.2 years (median 56 months).
Transient tumor swelling, or growth that plateaus after radiosurgery, may lead to unnecessary microsurgery or revision radiosurgery. In order to differentiate true tumor growth from tumor expansion, the tumor size must be mapped with serial MRI scans. Hasegawa and colleagues also have suggested that magnetic resonance spectroscopy, single photon emission tomography, or positron emission tomography may help determine if tumors are actively growing or showing signs of temporary expansion.
Tumor regression is a favorable prognostic sign of tumor control. Tumors that shrink rarely show signs of growth. In addition, the chance for tumor growth is extremely low for stable tumors 4 years post GKRS. Continuous monitoring after 4 years is necessary, however, because there has been at least one report of a patient developing an expanding cyst at the tumor margin 60 months after GKRS.
Some factors associated with continued tumor growth for unilateral vestibular schwannoma after gamma knife treatment have been imaging/targeting error, tumor biology, and large tumor volume and cystic tumor (the latter two factors are discussed later). Spatial distortion is known to occur with MRI. These distortions are most pronounced at soft tissue-bone interfaces, such as that in the internal auditory canal. As a means to accommodate this distortion and to prevent imaging/targeting error, some centers combine CT and MRI. Another possible cause for MRI error is that gadolinium may not enhance the lateral most extent of the intracanalicular portion of a vestibular schwannoma.
There has been no difference, however, in tumor control rates between patients receiving current doses of 12 to 13 Gy to the tumor margin and those patients who have received higher doses.
Table 3 provides a summary of tumor control rates from various, worldwide treatment centers. Inclusion criteria for the table were the following: minimum 100 patients reported, mean marginal dose of 13.5 Gy or less, and an average of 3 years of follow-up or longer. In a study by Myrseth and colleagues, tumor size was reported as the maximal tumor diameter, including the intracanalicular portion (17.5% were 0–10 mm; 66% were 11–20 mm; and 16.5% were 21–30 mm).



