Purpose
To investigate the effectiveness and safety of a new surgical technique of fovea-sparing internal limiting membrane (ILM) peeling for the treatment of foveal retinal detachments (RDs) in eyes with myopic traction maculopathy.
Design
Retrospective, consecutive, interventional case series.
Methods
Forty-five eyes of 45 consecutive patients who underwent vitrectomy and ILM peeling for the treatment of a foveal RD attributable to myopic traction maculopathy were studied. The patients were divided into 2 groups by the area of ILM peeled: complete macular ILM peeled group (30 eyes) and fovea-sparing ILM peeled group (15 eyes). A gas tamponade was used in all of the eyes. The main outcome measures were the rate of development of a full-thickness macular hole (MH) and the best-corrected visual acuity (BCVA). All of the patients were followed for more than 6 months.
Results
A full-thickness MH developed in 5 of 30 eyes (16.7%) in the complete ILM peeled group and in none of the 15 eyes in the fovea-sparing ILM peeled group. Postoperative OCT examination showed a contraction of the residual ILM on the fovea and reduction of the outer lamellar holes in the fovea-sparing ILM peeled group. The postoperative BCVA was significantly better than the preoperative BCVA in the fovea-sparing ILM peeled group ( P = .04), but not in the complete ILM peeled group.
Conclusions
Fovea-sparing ILM peeling results in better visual and anatomic outcomes for the treatment of foveal RD attributable to myopic traction maculopathy. These were accomplished by reducing the development of a full-thickness MH.
Myopic traction maculopathy is a major cause of visual impairment in eyes with pathologic myopia. Eyes with myopic traction maculopathy include those with vitreomacular traction, retinal thickening, macular retinoschisis (MRS), lamellar macular hole (lamellar MH), and foveal retinal detachment (RD). The pathogenesis of myopic traction maculopathy is varied; however, the inflexibility of the internal limiting membrane (ILM) is considered to be an important cause of the maculopathy. In addition, vitreomacular traction from a perifoveal posterior vitreous detachment, from the epiretinal membrane, and from remnants of the cortical vitreous layer may cause myopic traction maculopathy.
Earlier studies have reported on the progression of a MRS into more serious complications such as foveal RD or full-thickness MH during its natural course. Gaucher and associates reported that 6 of 18 eyes with MRS that did not undergo surgical intervention developed full-thickness MH during a mean follow-up of 34.7 months (range, 12 to 60 months). We also reported that 4 of 8 eyes with MRS progressed to foveal RD or full-thickness MH in a follow-up period of more than 2 years. Based on these natural course studies, the effectiveness of pars plana vitrectomy to treat myopic traction maculopathy has been evaluated, although its effectiveness has not been fully determined yet.
The development of a full-thickness MH is a serious complication in highly myopic eyes with a foveal RD after vitrectomy. Hirakata and associates reported that the risk of the postoperative development of a full-thickness MH is higher in highly myopic eyes with severe foveal RD than in eyes without a foveal RD. This is important because a full-thickness MH is associated not only with reduced vision but also with a risk of developing a MH retinal detachment in highly myopic eyes.
The mechanisms of why and how full-thickness MHs develop postoperatively in eyes with foveal RD have not been fully determined; however, we hypothesized that ILM peeling will increase the risk of developing a full-thickness MH. ILM peeling is a widely performed technique to treat foveal RDs, although some studies with a limited number of patients reported that a foveal RD can be treated by vitrectomy without ILM peeling. The mechanical traction on such a thinned central fovea by peeling the ILM off of the fovea could induce a break of the central foveal tissue.
These concerns prompted us to develop a new technique of ILM peeling for highly myopic eyes with a foveal RD, which we called fovea-sparing ILM peeling. Thus, the purpose of this study was to evaluate the safety and effectiveness of fovea-sparing ILM peeling in preventing the postoperative development of a full-thickness MH for the treatment of a foveal RD attributable to myopic traction maculopathy.
Patients and Methods
All of the patients who underwent the fovea-sparing ILM peeling were informed on the possible benefits and risks. The risks included retinal toxicity from the dye used to make the ILM more visible and a need for a second vitrectomy to remove the residual ILM. Other risks included those caused by vitrectomy itself, such as RD or endophthalmitis. All patients understood and agreed to have the surgery.
Forty-five eyes of 45 consecutive patients who underwent vitrectomy with ILM peeling to treat a foveal RD attributable to myopic traction maculopathy were studied retrospectively. The surgeries were performed from December 6, 2005 to June 16, 2011 at the Tokyo Medical and Dental University.
Pathologic myopia was defined as a myopic refractive error (spherical equivalent) of >-8.00 diopters (D) or an axial length >26.5 mm. The presence of a foveal RD was confirmed by spectral-domain optical coherence tomography (SD-OCT; Cirrus; Carl Zeiss Meditec, Dublin, California, USA). The eyes with a preoperative full-thickness MH, myopic choroidal neovascularization, or macular atrophy that could affect the central vision were excluded. Also excluded were those with a history of ocular trauma and those with other retinal diseases that could affect the vision, such as diabetic retinopathy or retinal vein occlusion. Eyes with dense opacities of the media such as corneal opacities or dense cataracts were also excluded. All of the patients had follow-up periods of at least 6 months.
All patients had a complete ophthalmic evaluation, including manifest refraction and measurement of best-corrected visual acuity (BCVA).
Surgical Techniques
A standard 25-gauge 3-port pars plana vitrectomy was performed on all eyes under local anesthesia. First, the central vitreous core was removed, and then the posterior hyaloid was removed by active suction using a vitreous cutter or a back-flash needle. The ILM was stained with indocyanine green (ICG; 0.025% concentration) for 30 seconds, and peeled over the complete macular area in all of the patients from December 6, 2005 to September 10, 2009. This group was called the complete ILM peeled group.
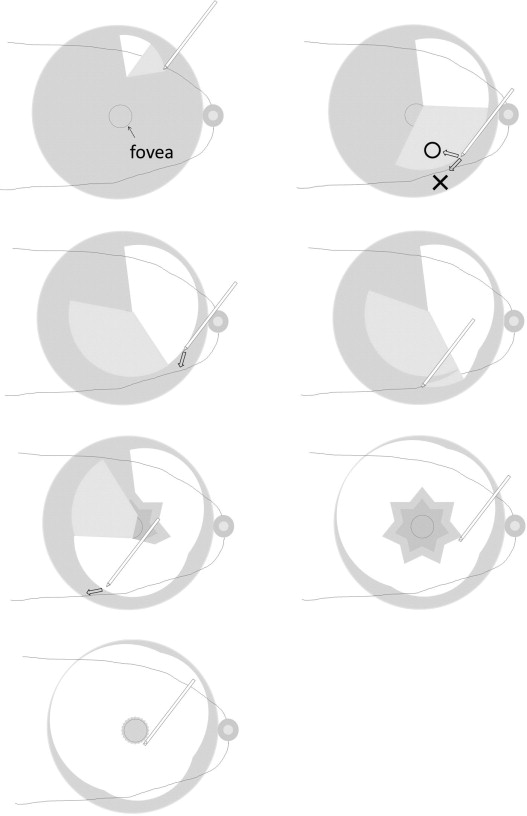
From October 15, 2009 to June 16, 2011, fovea-sparing ILM peeling was performed on all of the patients. For this procedure, the ILM was grasped with an ILM forceps and peeled off in a circular fashion ( Figure 1 ), but the ILM was not completely removed and was left attached to the fovea. After the ILM was peeled from the entire macula area except the foveal area (in a circular area with a diameter approximately that of the vertical extent of the optic disc), the peeled ILM was trimmed with a vitreous cutter. Finally, fluid-air exchange was performed, followed by an injection of 18% sulfur hexafluoride. The patients were instructed to maintain a prone position for at least 1 week postoperatively. The surgeries were performed by 3 surgeons (N.S., Y.S., and M.O.) at the Tokyo Medical and Dental University Hospital.
Statistical Analyses
Statistical analyses were performed with SPSS for Windows version 11.5 (SPSS Inc, Chicago, Illinois, USA). The significance of the differences in age, axial length, follow-up period, and preoperative and postoperative BCVAs between the 2 groups was determined by Mann-Whitney U tests. The significance of differences in the lens status, sex distribution, surgeon distribution, and rate of developing a full-thickness MH postoperatively was determined by Fisher exact probability tests. The significance of differences between preoperative and postoperative BCVA in each group was determined by paired t tests. A P value <.05 was considered statistically significant.
Results
Demographics of Patients
The demographics of the 45 eyes of 45 patients are shown in Table 1 . There were 30 eyes of 30 patients in the complete ILM peeled group and 15 eyes of 15 patients in the fovea-sparing ILM peeled group. The differences in the age, sex distribution, axial length, and preoperative lens status between the 2 groups were not significant. Because of the difference in when the 2 types of surgeries were begun, the average follow-up period was significantly shorter in the fovea-sparing ILM peeled group than that in the complete ILM peeled group. The distribution of surgeons for the 2 types of surgeries was not significantly different ( Table 2 ). The number of eyes with simultaneous lens removal and insertion of an intraocular lens was 19 of 30 (63.3%) in the complete ILM peeled group and 8 of 15 (53.3%) in the fovea-sparing ILM peeled group. This difference in the percentages was not significant. Only 1 patient in the complete ILM peeled group did not receive simultaneous lens removal because this patient was younger than 50 years and had no cataract.
| Complete Macular ILM Peeling (30 Eyes) | Fovea-Sparing ILM Peeling (15 Eyes) | P Value | |
|---|---|---|---|
| Age (y), mean ± SD | 63.2 ± 12.0 | 65.8 ± 7.1 | .81 a |
| Sex (male/female) | 5/25 | 5/10 | .26 b |
| Axial length (mm), mean ± SD | 29.1 ± 1.8 | 29.1 ± 1.1 | .86 a |
| Lens status, phakia/pseudophakia/aphakia | 20/9/1 | 8/7/0 | .56 b |
| Follow-up (mo), mean ± SD | 47.5 ± 18.5 | 11.3 ± 5.3 | <.001 a |
| CMIP Group (n = 30) | FSIP Group (n = 15) | P Value | |
|---|---|---|---|
| Surgeon, N.S./Y.S./M.O. | 8/20/2 | 2/12/1 | .75 a |
| Surgery combined with PEIOL, no. (%) | 19 (63.3%) | 8 (53.3%) | .54 a |
| Preoperative BCVA in logMAR, mean ± SD | 0.74 ± 0.5 c , d | 0.65 ± 0.5 e , f | .46 b |
| (Average Snellen visual acuity) | (0.18) | (0.22) | |
| Postoperatove BCVA in logMAR, mean ± SD | 0.58 ± 0.6 c | 0.34 ± 0.4 e | .23 b |
| (Average Snellen visual acuity) | (0.26) | (0.45) | |
| BCVA in logMAR on last visit, mean ± SD | 0.60 ± 0.6 d | 0.35 ± 0.4 f | .24 b |
| (Average Snellen visual acuity) | (0.25) | (0.44) | |
| Visual improvement in logMAR, mean ± SD | 0.16 ± 0.3 | 0.31 ± 0.2 | .24 b |
| Improved, >0.2 logMAR | 16 | 11 | .31 a |
| Stable | 10 | 4 | |
| Worsened, <-0.2 logMAR | 4 | 0 | |
| Postoperative FTMH with or without RD, no. (%) | 5 (16.7%) | 0 (0%) | .15 a |
c P = .07 (Mann-Whitney U test).
d P = .08 (Mann-Whitney U test).
e P = .04 (Mann-Whitney U test).
Anatomic Results
A full-thickness MH developed postoperatively in 5 of the 30 eyes in the complete ILM peeled group (16.7%; Figure 2 , Table 3 ) and in none of the 15 eyes in the fovea-sparing ILM peeled group (P = .15, Fisher exact probability tests). Three of the 5 eyes developed a RD around the full-thickness MH and underwent surgical treatment. The BCVA (in logarithm of the minimal angle of resolution [logMAR] units) was reduced or unchanged in the 5 eyes that developed a full-thickness MH.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


