The evolution of endoscopic sinus surgery has led to a paradigm shift in the management of sinonasal and anterior skull base tumors in the past decade. Endoscopic resection is considered by many institutions to be the gold standard approach even for extensive pathology. Endoscopic tumor surgery should not imply less surgery but rather an alternative to external operations providing the same access and enabling equivalent or superior visualization for resection of tumors. It also avoids much of the potentially significant morbidity associated with external operations. Successful endoscopic tumor resection requires experience, an understanding of tumor behavior, and the development of a unique skill set. Tumor removal is often performed inside-out. Regions such as the anterolateral maxilla and frontal sinus require special access. Orientation of the surgeon is different to that of simple inflammatory disease. A structured approach to vascular control is important to ensure a workable surgical field. The final cavity and reconstruction need to be fashioned to ensure that reasonable sinonasal physiology and function are retained, including the lacrimal apparatus. The endoscopic cavity created after extensive surgery requires different care compared with the mucosal-preserving techniques of inflammatory disease. This article describes these key methodological differences that enable extended endoscopic surgery of the sinonasal tract and anterior skull base.
Endoscopic resections of benign neoplastic disease of the anterior skull base and paranasal sinuses is now widely practiced. Selected malignancies can also be successfully managed by an endoscopic approach. However, the approach should never dictate the surgery performed. Anatomic location and areas involved by a pathologic condition should always be the determining factor. Similarly, pathology such as inverted papilloma, should never imply a particular surgery (endoscopic medial maxillectomy or lateral rhinotomy). Although endoscopic resection has replaced many open approaches at our institutions, the authors still use a combination of techniques to remove extensive disease.
The endoscopic surgeon performing extended procedures should be equally comfortable performing a similar open procedure. Endoscopic surgery should not imply conservative surgery. If a pathologic lesion is considered irresectable via an open approach then it is axiomatic that this is true for the endoscopic option. There are a variety of open approaches that can be applied and they have been well described, however, they have a limited role in the management of benign disease. The midface degloving approach is perhaps 1 open approach that is still sometimes used to manage lesions for which an endoscopic approach may not suffice.
The authors believe the foundations of successful extended endoscopic surgery, whether for accessing a lateral frontal mucocele or removing malignant disease, relies on 5 important concepts: preoperative planning (surgery and equipment required), obtaining appropriate surgical access, micro- and macrovascular control; reconstruction of nasolacrimal physiology; and postoperative care of the large endoscopic cavity ( Table 1 ).
| Preoperative planning | Ensure that imaging, skill, equipment, and a predefined surgical plan are created |
| Surgical access | Accessing anterolateral disease of the maxilla and within the frontal sinus requires unconventional or combination techniques |
| Anatomic orientation | Preoperatively defining a structured approach to identify fixed anatomic landmarks |
| Vascular control | Microvascular management: preoperative reduction of associated inflammatory changes, anesthetic techniques, and intraoperative vasoconstriction Macrovascular control with a structured approach to the ethmoidal, sphenopalatine, internal maxillary, and carotid artery |
| Reconstruction | Ensuring a functional lacrimal system, the formation of a final cavity that will allow relatively normal nasal physiology Reconstruction of dura or periorbita |
| Postoperative management of the large cavity | Controlling adhesions, crusting, bacterial colonization and facilitating mucosalization |
Preoperative planning
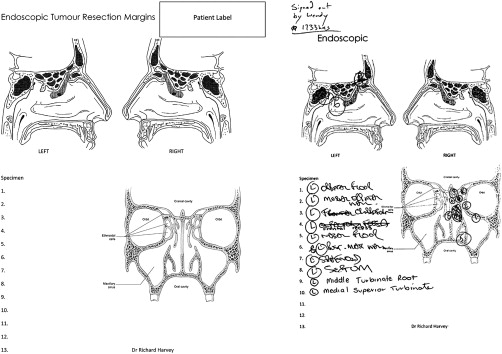
The philosophy of complete endoscopic resection can be retained without the need for traditional en bloc surgery. The limits of the area to be resected and bone removed can often be defined before surgery begins. An attempt should be made to define the surgical margins preoperatively. This ensures that a surgical plan is adhered to and will enhance total removal. The authors believe there needs to be a shift away from the patho-etiology focus of traditional teachings and emphasize the need to resect anatomic zones or regions, therefore tailoring surgery to the exact extent of disease and preserving normal structures. This is not pathology-specific surgery but site-specific surgery. The ability to gain good visualization and access to the anatomic region of the lesion is essential. Particularly in malignant disease, being able to accurately map resection margins is vital for intra- and postoperative decision making ( Fig. 1 ). Further resection of positive frozen section margins can be inaccurate if many (>10) biopsies are taken. Postoperatively, accurate surgical mapping aids radiation oncologists in defining treatment fields and assists focused endoscopic surveillance.
Endoscopic surgical access
There are 4 areas notorious for recurrence and present challenging access :
- 1.
Anterolateral maxilla
- 2.
Frontal sinus
- 3.
Supraorbital ethmoid cell
- 4.
Floor of a well-pneumatized maxillary sinus.
Many staging systems have been developed for benign pathologic conditions commonly managed endoscopically. Examples by Cannady and colleagues, Jameson and Kountakis, Krouse, and Woodworth and colleagues all touch on important aspects in the groupings of their patients. However, unlike malignant staging, it is fundamentally the completeness of surgical resection of the tumor that dictates the final outcome for benign disease. These staging systems reflect surgical complexity of access rather than intrinsic disease factors such as nodal or metastatic spread. Synchronous and metachronous malignant disease may occur but the effect of these events on outcome is unlikely to be reflected in these staging systems. Potentially, the difficult or higher-stage tumors are simply those lesions associated with more difficult access.
Predefining regions or zones that require endoscopic access and resection has become an important process in our institution ( Table 2 ). The limits of tissue removal may too easily align with surgeon comfort rather than anatomic boundaries defined by the presurgical clinical and radiological examination. The principles of en bloc resection, from its oncologic foundations in managing malignant disease, are often followed by some surgeons to ensure that the appropriate margins have been reached. With careful planning and preoperative evaluation of radiology, it is possible to define the zone of resection likely to be required. Table 2 outlines our current surgical approach to endoscopic resection.
| Anatomic Site | Pathology Involves | Surgical Access Consideration |
|---|---|---|
| Anterolateral maxilla and infratemporal fossa | Zone 2/3 | Appropriate angled instruments need to be available; 40° burrs and debriders are not angled enough for zone 3; 60–75° instruments are usually required |
| Zone 3 or 4 | Ancillary techniques required such as maxillary trephine, maxillotomy, or trans-septal access | |
| Zone 5 | An open approach may be better | |
| Frontal sinus | Medial quarter of orbital roof | Unilateral access with a Draf 2a or 2b |
| Medial half of orbital roof or lateral posterior and anterior walls | Draf 3 Possible trephine | |
| Orbital roof lateral to midpoint | External trephine or osteoplastic flap required | |
| Frontal recess | Draf 2b or 3 required as reconstruction of the recess with exposed bone requires greater intervention | |
| Supraorbital ethmoid | Anterior ethmoidal artery | A dehiscent anterior ethmoidal artery may be obscured on imaging because of a nearby pathologic lesion; control is required in approach |
| Orbitocranial cleft | The potential for dural or periorbital injury needs to be balanced with pathology and risk of recurrence | |
| Maxillary floor | Dental roots | Damage to roots likely or pathology may be of odontogenic nature with tooth extraction or endodontics required |
| Low maxilla relative to nasal floor | Angled instruments or ancillary access, such as maxillary trephination or modified medial maxillectomy required |
Accessing Anterolateral Disease
Five zones were developed and are used at the Medical University of South Carolina (MUSC) Rhinology and Skull Base and St Vincent’s Rhinology and Skull Base Divisions when planning surgical access in endoscopic tumor removal ( Fig. 2 A; Table 3 ).
| MUSC Zone | Anatomic Region | Surgery Techniques | Instrumentation |
|---|---|---|---|
| Zone 1 | Tumor limited to septum, turbinates, middle meatus, ethmoid, frontal, sphenoid sinuses, medial orbital wall (inverted papilloma, hemangioma, chondroma) | Surgery includes turbinectomy and septectomy | Basic endoscopic sinus surgery instrumentation |
| Zone 2 | Tumor extends to involve maxillary sinus medial to the inferior orbital nerve (ION), limited posterior wall or maxillary floor (inverted papilloma, juvenile nasopharyngeal angiofibroma) | Middle meatal antrostomy, frontal recess surgery (Draf 1–3, trephine, or osteoplastic), sphenoid, ethmoid surgery. Some sinus surgery to include sphenopalatine artery management or modified endoscopic medial maxillectomy needed for tumor surveillance | Angled instrumentation and bipolar diathermy/endoscopic clip applicators. Maxillary trephination may be used. Rongeurs or chisel required for bone removal |
| Zone 3 | Tumor involves nasolacrimal duct, medial buttress, or maxilla lateral to ION and up to the zygomatic recess (inverted papilloma, juvenile nasopharyngeal angiofibroma) | Requires dacrocystorhinostomy, possible trans-septal approach, possible endoscopic Denker maxillotomy, or open approach (sublabial Caldwell-Luc type approach) | Angled instrumentation has limitations in access. Standard endoscopic sinus surgery instruments via trans-septal approach or maxillary trephine may be required |
| Zone 4 | Tumor involves anterior maxillary wall with minimal extension into premaxillary soft tissue | Surgery requires trans-septal approach, endoscopic Denker maxillotomy or premaxillary endoscopic sinus surgery approach. Sublabial open type approach Open lateral rhinotomy/midface degloving | Endoscopic sinus surgery instruments via trans-septal approach or maxillary trephine may be required Angled ipsilateral endoscopic instruments of little utility |
| Zone 5 | Tumor involves premaxillary tissue or skin | Surgery requires open approach | Open surgical instrumentation |
Zone 1 : tumor is limited to
- •
Septum
- •
Turbinates
- •
Middle meatus
- •
Ethmoid
- •
Frontal
- •
Sphenoid sinuses
- •
Medial orbital wall.
Surgery may include turbinectomies, septectomy, middle meatal antrostomy (MMA), frontal, sphenoid, ethmoid surgery. Basic endoscopic sinus surgery instrumentation is required (see Fig. 2 B).
Zone 2 : tumor extends to involve
- •
Maxillary sinus medial to the inferior orbital nerve (ION)
- •
Limited posterior wall or
- •
Maxillary floor.
MMA or modified endoscopic medial maxillectomy (MMM) is needed for tumor surveillance. Sinus surgery to include MMA ± MMM and sphenopalatine artery management and some angled instrumentation is needed (see Fig. 2 C).
Zone 3 : tumor involves
- •
Maxilla lateral to ION and up to the zygomatic recess
- •
Nasolacrimal duct or medial buttress may need resection.
Surgery may require dacrocystorhinostomy (DCR), possible trans-septal approach, trephine, total medial maxillectomy (TMM) or maxillotomy, medial buttress removal. Traditional open approaches are described for tumors in this location (sublabial Caldwell-Luc type approach, open lateral rhinotomy, and midface degloving). Angled instrumentation is mandatory for ipsilateral surgery (see Fig. 2 D).
Zone 4 : Tumor involves
- •
Anterior maxillary wall without extension into premaxillary soft tissue.
Surgery requires trans-septal dissection with direct drilling to the anterior maxillary wall (mucosal side) or 1 of the previously described external approaches (see Fig. 2 E).
Zone 5 : tumor involves premaxillary tissue and/or skin.
Surgery requires open approach (see Fig. 2 F).
Modified medial maxillectomy
This technique is widely used to manage access to the maxilla, infratemporal fossa, maxillary artery, and maxillary sinus floor. It is technically the same as that described as a salvage procedure for chronic maxillary sinusitis ( Fig. 3 ). A modified medial maxillectomy also ensures dependent drainage for a final cavity that may not have normal mucocillary function. In additional, it provides excellent access for postoperative care and surveillance.
Trans-septal Access
Our current technique involves the creation of a large posterior based septal flap in the contralateral nasal cavity. This mucoperichondrial/periosteal flap is pedicled posteriorly on the septal branch of the sphenopalatine artery. The anterior incision commences at the hemitransfixion, or mucosquamous junction ( Fig. 4 C). The lateral incision starts well lateral on the nasal floor near the inferior meatus (see Fig. 4 A). Foreshortening of the flap after elevation occurs and additional width is important for adequate reconstruction. The superomedial incision is made high, under the nasal dorsum (see Fig. 4 B). The flap is then raised back to the middle turbinate and reflected between septum and middle turbinate to prevent injury during the subsequent tumor removal (see Fig. 4 D). The ipsilateral mucosa over this area is raised as an inverted-U flap with a random blood supply based inferiorly from the nasal floor (see Fig. 4 E). Beginning at the head of the inferior turbinate, a window of septal cartilage is removed posteriorly (see Fig. 4 F). An area of 1.5×2 cm is removed to allows the endoscope and instrument to work comfortably through the septum. This approach is ideal for zone 3 or 4 pathologic conditions.
Maxillary Trephination
The development of specialized instrument sets for maxillary trephination ( Fig. 5 ) has greatly assisted the ease with which an additional port for endoscope or instrument can be deployed. Robinson and colleagues have help to redefine the landmarks for the placement of these trephines. The safest entry point for a canine fossa puncture was where a vertical line drawn through the midpupillary line was bisected by a horizontal line drawn through the floor of the pyriform aperture. The placement of the trephine can assist access to the maxillary floor, retraction for infratemporal tumors, and early access for maxillary artery ligation and control. This is an excellent adjunct to lateral infratemporal fossa or lateral maxillary lesion. However, for those pathologic conditions involving the anterior wall itself, the trephine does not improve surgical access and will come through tumor in its approach.
Maxillotomy
Endoscopic maxillotomy or endoscopic Denker maxillotomy has been described and can provide similar access to the trans-septal approach. This procedure involves the removal of the medial buttress via osteotomies ( Fig. 6 ). A premaxillary plane is raised and the entire medial buttress is removed. The lacrimal apparatus is disrupted as with a total medial maxillectomy. However, the additional bone removal disrupts the anterior superior alveolar nerve, potentially transecting the canine root and may lead to loss of lateral support of the alar cartilage to the piriform aperture. When performed via a direct nasal or endoscopic route, the resulting alar retraction and collapse is never as severe compared with similar lateral rhinotomy approaches but can still occur. The authors prefer the trans-septal approach for most lateral pathologic conditions but maxillotomy is a good option if the medial buttress bone is directly involved in pathology.
Frontal Sinus
The coronal incision/osteoplastic flap and browline incision/frontal trephine are 2 important open adjuncts that are used to manage frontal sinus extension. Trans-facial incisions are rarely used. Blepharoplasty incision or orbital crease approaches have been described recently.
Lateral frontal sinus and trephination
The modified endoscopic Lothrop procedure (MELP, Draf 3, frontal drillout) is an established means of access to the frontal sinus. Its use in inflammatory sinus disease and as access for treatment of cerebrospinal fluid leak and benign neoplasms is well documented. In the treatment of benign lesions, particularly inverted papilloma, drilling of bone at the site of attachment rather than the use of scraping techniques may reduce the risk of recurrence. Therefore, to adequately treat these lesions, access is required such that an angled drill can be used under vision with bone contact.
The ability to contact the bone under vision with the head of a 70° diamond burr defines good access. Post Draf 3, lateral endoscopic access to the anterior and posterior walls of the frontal sinus is excellent for 95% of anatomy (Timperley D and Harvey RJ, unpublished data, 2010). Access to the orbital roof was limited (10.3 ± 4.6 mm from medial orbital wall). Access to the orbital roof is reliable in the medial orbital quarter only. For a frontal sinus pneumatized beyond the midorbital point, only 10% of lateral orbital roofs were contacted. For lesions between these points, the anterior-posterior distance between the olfactory fossa and the outer periostium of the nasofrontal beak may help to define which lesions are amenable to endoscopic access. Access correlated with this distance between the olfactory fossa and outer periostium of the nasofrontal beak (r = 0.6, P <.01) (Timperley D and Harvey RJ, unpublished data, 2010).
Disease of the frontal sinus is often not accessible for a total resection via a trans-nasal only approach even when a Draf 3 has been performed. Other adjunctive procedures may be necessary. The frontal trephine and osteoplastic flap form the basis of achieving additional access. Understanding the need for these in the preoperative assessment is key. They are easy to perform but the need for them should be defined preoperatively and not discovered as unexpectedly necessary during the surgery. Use of magnetic resonance imaging and computed tomography (CT) help in this assessment.
Frontal trephine is an excellent adjunct for lesions lateral to the midorbital point. The formation of a small 1- to 2-cm incision and bone window allows dissection instrument and endoscope to facilitate dissection ( Fig. 7 ). Frontal trephine can also be used to allow an above and below visualization and dissection technique. The midorbital exit point for the supraorbital neurovascular pedicle and awareness of the supratrochlear nerve bundles is important to ensure safe dissection.
Frontal recess
Access is not the only concern. Reconstruction of the frontal recess may be necessary if the pathologic lesion has been removed from within the frontal sinus. A combination of maximal widening of the frontal recess (Draf 2a, b or 3), mucosal preservation, and possible sialastic sheet stenting for 7 to 21 days postoperatively may be appropriate in this circumstance. In addition, inadvertent frontal recess obstruction may occur if the surgery is performed adjacent to frontal recess. A Draf 2a is routinely performed for most endoscopic resections. This ensures correct localization of the frontal recess, posterior table, and aids postoperative care.
Supraorbital Ethmoid Cell
The supraorbital ethmoid (SOE) cell presents a unique surgical problem for the treating rhinologist. Any anterior approach (open or endoscopic) will have great difficulty in removing disease from the increasingly narrow orbitocranial cleft of the SOE, formed between the orbit roof and anterior cranial fossa, as dissection proceeds posterior. Instrumentation may simply not fit into this cleft. Even with removal of orbital bone (the medial wall and roof) and ethmoid roof, the cleft of dura and periorbita is still restrictive ( Fig. 8 ). Only a subcranial or frontal craniotomy approach allows elevation of the anterior cranial fossa dura and removal of the superior bone; the disease in this cleft can then be addressed. Identification of disease in this area preoperatively is important to balance the approach-related morbidity and need for completeness of resection.
Dental Roots
The adult maxillary sinus pneumatizes below the nasal floor in most adults. The bone between dental roots and sinus mucosa is on average only 2 mm for the second premolar tooth. Significant morbidity can arise from aggressive drilling in this area. Identifying the maxillary dental relationship is important for preoperative counseling. A modified medial maxillectomy (see Fig. 3 ) facilitates access, postoperative care, and follow-up for pathologic conditions in the maxillary sinus floor.
Endoscopic surgical access
There are 4 areas notorious for recurrence and present challenging access :
- 1.
Anterolateral maxilla
- 2.
Frontal sinus
- 3.
Supraorbital ethmoid cell
- 4.
Floor of a well-pneumatized maxillary sinus.
Many staging systems have been developed for benign pathologic conditions commonly managed endoscopically. Examples by Cannady and colleagues, Jameson and Kountakis, Krouse, and Woodworth and colleagues all touch on important aspects in the groupings of their patients. However, unlike malignant staging, it is fundamentally the completeness of surgical resection of the tumor that dictates the final outcome for benign disease. These staging systems reflect surgical complexity of access rather than intrinsic disease factors such as nodal or metastatic spread. Synchronous and metachronous malignant disease may occur but the effect of these events on outcome is unlikely to be reflected in these staging systems. Potentially, the difficult or higher-stage tumors are simply those lesions associated with more difficult access.
Predefining regions or zones that require endoscopic access and resection has become an important process in our institution ( Table 2 ). The limits of tissue removal may too easily align with surgeon comfort rather than anatomic boundaries defined by the presurgical clinical and radiological examination. The principles of en bloc resection, from its oncologic foundations in managing malignant disease, are often followed by some surgeons to ensure that the appropriate margins have been reached. With careful planning and preoperative evaluation of radiology, it is possible to define the zone of resection likely to be required. Table 2 outlines our current surgical approach to endoscopic resection.
| Anatomic Site | Pathology Involves | Surgical Access Consideration |
|---|---|---|
| Anterolateral maxilla and infratemporal fossa | Zone 2/3 | Appropriate angled instruments need to be available; 40° burrs and debriders are not angled enough for zone 3; 60–75° instruments are usually required |
| Zone 3 or 4 | Ancillary techniques required such as maxillary trephine, maxillotomy, or trans-septal access | |
| Zone 5 | An open approach may be better | |
| Frontal sinus | Medial quarter of orbital roof | Unilateral access with a Draf 2a or 2b |
| Medial half of orbital roof or lateral posterior and anterior walls | Draf 3 Possible trephine | |
| Orbital roof lateral to midpoint | External trephine or osteoplastic flap required | |
| Frontal recess | Draf 2b or 3 required as reconstruction of the recess with exposed bone requires greater intervention | |
| Supraorbital ethmoid | Anterior ethmoidal artery | A dehiscent anterior ethmoidal artery may be obscured on imaging because of a nearby pathologic lesion; control is required in approach |
| Orbitocranial cleft | The potential for dural or periorbital injury needs to be balanced with pathology and risk of recurrence | |
| Maxillary floor | Dental roots | Damage to roots likely or pathology may be of odontogenic nature with tooth extraction or endodontics required |
| Low maxilla relative to nasal floor | Angled instruments or ancillary access, such as maxillary trephination or modified medial maxillectomy required |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


