Purpose
To investigate the hypothesis that adult corneal endothelial cells can migrate after Descemet membrane endothelial keratoplasty (DMEK).
Design
Prospective observational study.
Methods
Five patients with Fuchs endothelial dystrophy were examined 1 year after uneventful DMEK. These patients had been selected on the basis of slightly decentered grafts and/or large descemetorrhexis showing areas of denuded corneal stroma, which were covered by neither the patients’ Descemet membrane (DM) nor the graft. These areas were investigated by in vivo confocal laser scanning microscopy using a specially designed Heidelberg Retina Tomograph II and Rostock cornea module equipped with custom-made software. Source data (frame rate 30 Hz, 384 × 384 pixels, 400 × 400 μm) were used to create large-scale maps of the scanned area in automatic real-time composite mode. In each case an on-line mapping with maximum size up to 3.2 × 3.2 mm (3072 × 3072 pixels) was performed.
Results
Corneal stroma overlying areas devoid of DM was transparent. In vivo confocal laser scanning microscopy of stroma devoid of DM revealed a monolayer of endothelial cells in all patients observed. The morphologic pattern of these cells was similar to that of endothelial cells on DM grafts but different from the morphology of the patients’ own endothelium, suggesting migration of donor endothelial cells from DMEK grafts.
Conclusions
The results strongly support the hypothesis that adult corneal endothelial cells are able to migrate in the human eye. Furthermore, we provide evidence to support the hypothesis that grafted endothelium migrates onto the host tissue, repopulating the corneal stroma with a regular endothelial phenotype.
After nearly a century of penetrating keratoplasty (PK), lamellar techniques for selective replacement of corneal structures have recently been considerably improved. Since 1998 various concepts for posterior lamellar keratoplasty have been developed to allow replacement of diseased corneal endothelium while maintaining the structural integrity of the host cornea. These techniques induce only negligible refractive changes and at the same time offer faster visual rehabilitation along with improved surface topography in comparison to standard PK.
When comparing different techniques for replacement of the host endothelium, procedures that result in minimal alteration of the posterior surface of the cornea might have an advantage over procedures that are associated with introduction of a relatively thick graft. The quality of the posterior corneal surface might be adversely affected by the addition of a posterior stromal lamella, which can lead to increased higher-order aberrations. Recently, Descemet membrane endothelial keratoplasty (DMEK) was described, allowing transplantation of isolated endothelium–Descemet membrane layer (EDM) without adherent corneal stroma. Initial results with this technique are equivalent or even superior to that of other lamellar techniques, possibly because there is minimal alteration of the posterior surface of the cornea.
While DMEK offers several distinct advantages and renders excellent short-term results, it has been associated with a significant decline in endothelial cells, especially during the early postoperative period. As in other forms of posterior lamellar surgery, it is currently not possible to guarantee long-term endothelial function after DMEK in a given patient. The further development of procedures for endothelial replacement as well as strategies for enhancement of endothelial viability after surgery would be facilitated if there were a greater knowledge about basic principles of endothelial function in the adult eye. In this respect, one of the important questions is if endothelial cells after lamellar surgery, such as DMEK, are able to migrate from the graft onto the recipient’s ocular tissues. In the absence of an experimental model investigating cell migration in humans, the description of postoperative causes complicated by graft dehiscence has lately sparked considerable controversy about the issue of cell migration following DMEK surgery.
Balachandran and associates have described 2 patients with nearly complete graft detachment after DMEK developing spontaneous corneal clearance 3 to 9 months postoperatively. These observations led the authors to suggest that endothelial cell migration onto the denuded recipient’s corneal stroma from either the donor or the recipient may result in restoration of the endothelial cell layer and explain recovery of corneal transparency. Although these findings challenged the established concept that complete graft attachment is required for corneal function, it raised the interesting question whether endothelial cell migration can occur after DMEK and whether repopulation may arise from either donor or remaining recipient endothelial cells. Subsequently, several other cases providing evidence of endothelialization of the recipient’s posterior stroma in the presence of a detached graft have been described. The concept of endothelial migration has also been supported by a histopathologic report examining the donor lenticule after failed Descemet stripping automated endothelial keratoplasty (DSAEK) and demonstrating de novo formation of DM along the lateral wound edge indicative of endothelial migration.
The process of Descemet stripping often results in irregular removal of large portions of the Descemet membrane (DM) in the far periphery of the cornea. Since exact graft centration in DMEK is quite challenging, a significant proportion of patients have slightly decentered grafts that overlap with the patient’s DM on one side and the patient’s denuded stroma on the other side. These areas of denuded stroma provide an excellent model to study the migration of endothelial cells in vivo. Since these areas are localized in the far periphery of the cornea, they are inaccessible to standard techniques for visualization of endothelial cells. Furthermore, the reproducible mapping of landmarks on the inner surface of the cornea, such as the edge of the EDM graft or the margin of the donor DM, has not been possible so far.
The occasional occurrence of graft decentration in recipient eyes after DMEK offers the unique possibility to study potential processes of endothelial cell migration onto the denuded areas of recipient stroma in vivo. By using high-resolution confocal microscopy, it should be possible to distinguish between host and donor endothelial cell migration. Therefore, the purpose of this prospective observational study was to investigate the hypothesis that corneal endothelial cell migration occurs after DMEK onto the denuded stroma of the recipient. We describe the use of a custom-designed in vivo confocal laser scanning microscope for the Heidelberg retina tomograph (HRT) to visualize and quantify endothelial cells in the periphery of the cornea in relation to defined landmarks. Using this technique, we provide evidence supporting the hypothesis that endothelial cells from an EDM graft can migrate onto the host’s corneal stroma.
Methods
Five patients (2 men and 3 women, aged 43 to 75 years) with Fuchs endothelial dystrophy underwent uneventful DMEK between May and July 2009 using the technique originally described by Melles, with some modifications concerning graft preparation, configuration, and insertion. One day before surgery a Nd:YAG laser iridotomy was performed. EDMs were stripped of the donor cornea immediately prior to transplantation using a submerged bimanual technique in which the peripheral EDM was lifted by blunt dissection with a round knife following incision with a razor blade. The central edge was then grasped with 2 forceps and removed by simultaneous centripetal movement of the 2 forceps followed by trephination with an 8-mm trephine. To ensure orientation of the graft, 3 marks were introduced as previously described. Following complete detachment, the EDM roll was transferred into a standard intraocular lens injector cartridge (Acri.Tec GmbH, Hennigsdorf, Germany), inserted through a 2.5-mm corneal tunnel, unfolded by the help of air bubbles and attached to the stroma by filling the anterior chamber completely with air for 30 minutes. Upon completion of the surgery, air was reduced to about 50% of the anterior chamber volume. Our patients experienced neither intraoperative nor postoperative complications.
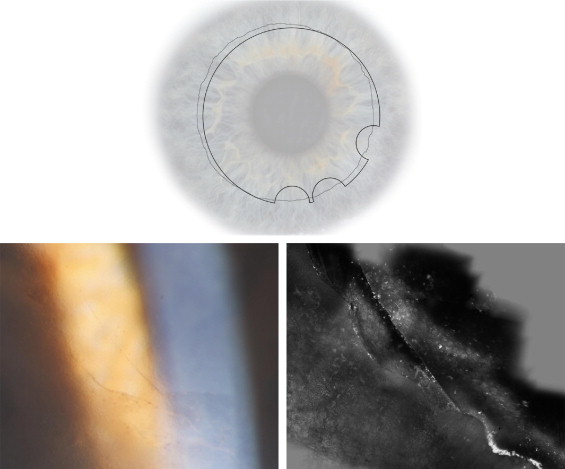
The 5 patients had been selected from a larger group of DMEK patients because of slightly decentered grafts and/or large descemetorrhexis ( Figure , Top). Therefore all patients showed areas of denuded corneal stroma, which was covered by neither the patients’ DM nor the graft ( Figure , Top, and Bottom left). These areas were investigated by in vivo confocal laser scanning microscopy in June 2010.
For in vivo confocal laser scanning microscopy the Heidelberg Retina Tomograph II (HRT II) and the Rostock cornea module (RCM) equipped with a water immersion objective (63×/0.95 W, 670 nm, ∞/0; Zeiss, Jena, Germany) and source data (frame rate 30 Hz, 384 × 384 pixels, 400 × 400 μm) were used to create large-scale maps of the scanned area in automatic real-time composite mode. In each case an on-line mapping with maximum size up to 3.2 × 3.2 mm (3072 × 3072 pixels) was performed by the same examiner. At the beginning of the investigation, the eye was anesthetized by applying topical proparacaine 0.5% eye drops (Ursapharm, Saarbruecken, Germany). The ocular surface was lubricated with a thin layer of Vidisic gel (Bausch & Lomb/Dr Mann Pharma, Berlin, Germany) prior to touching the patient’s cornea with the instrument. Digital images for storage were obtained using a water immersion objective (63×/0.95 W, 670 nm, ∞/0; Zeiss, Jena, Germany) with an adjustable focus plane. The HRT II/RCM provides image segments measuring 400 × 400 μm. Images from all corneal layers were captured in areas devoid of DM. The device’s z-scan depth function permitted automatic image acquisition of up to 30 images per second.
All patients underwent slit-lamp examination for evaluating corneal transparency. To investigate the density of the corneal endothelial cells on the graft compared to the endothelial cell layer covering the denuded corneal stroma, confocal images were evaluated by semi-quantitative measurements. Endothelial cells were counted in 3 representative areas of both the EDM graft and the denuded corneal stroma using superimposed circles of 20 mm diameter. For statistical analysis, Statistica software for Windows (StatSoft, Tulsa, Oklahoma, USA) was used. The Wilcoxon rank sum test was used to compare endothelial cell counts of both areas, P values < .05 or less were considered statistically significant.
Results
Corneal Transparency
Both the corneal epithelium and stroma in areas devoid of patients’ DM and/or grafted DM were completely unremarkable (throughout the entire area of the cornea). Upon slit-lamp examination, epithelium and stroma were clear and had the same appearance as neighboring areas overlying patients’ or grafted DM ( Figure , Top, and Bottom left).
Evidence of Migration of Corneal Endothelial Cells
As shown in the Figure , the border line between the recipients’ endothelial cell layer and the grafted endothelial cell layer could be identified using in vivo confocal laser scanning microscopy. In all patients the posterior stromal surface devoid of DM was completely covered with endothelial cells ( Figure , Bottom right). The visualization of the morphology of the endothelial cell layer revealed clear differences between the recipients’ and the grafted cells. In areas of the patients’ own, pathologically altered DM, small, scattered, irregularly shaped endothelial cells were observed. In contrast, regularly arranged, polygonal endothelial cells forming a typical honeycomb pattern could be detected in areas of transplanted DM. The endothelial cells covering the patients’ denuded corneal stroma closely resembled that of the EDM graft by appearing as regular, polygonal cells forming a honeycomb pattern. Semi-quantitative endothelial cell counts in both the EDM graft and the endothelial layer covering the denuded corneal stroma showed no significant differences. Together, these in vivo observations suggest migration of endothelial cells from the donor EDM graft onto the recipient’s corneal stroma after DMEK.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


