Successful outcomes of endoscopic approaches to benign sinonasal tumors have launched interest in expanding its use for sinonasal malignancy. Because of the heterogeneity and rarity of sinonasal malignancy, evidence for clinical outcomes of endoscopic approaches versus traditional craniofacial resection is low. Using the Oxford Center for Evidence-based Medicine guidelines, we present the existing evidence comparing both techniques for a variety of sinonasal malignancies.
The following points list the level of evidence based on Oxford Center for Evidence-Based Medicine guidelines.
- •
Esthesioneuroblastoma—Endoscopic approaches may provide higher survival rates compared with traditional craniofacial open surgery. Level 2A.
- •
Sinonasal melanoma—Traditional craniofacial resection remains the gold standard, but endoscopic methods may provide similar rates of long-term survival for patients. Level 4.
- •
Nasopharyngeal carcinoma—Endoscopic approaches may provide optimistic results, but evidence comparing outcomes with traditional craniofacial resection is lacking. Level 4.
- •
Sinonasal adenocarcinoma (SNAC)—Endoscopic approaches may provide optimistic results, but evidence comparing outcomes with traditional craniofacial resection is lacking. Level 4.
- •
Sinonasal undifferentiated carcinoma (SNUC)—Two-year survival rates for endoscopic approaches are encouraging, but further prospective comparative data are necessary. Level 4.
Overview of sinonasal and skull base cancer
Initial interest in endonasal skull base surgery was first described by Caton and Paul in the late 19th century. Since that time, advances in anatomic knowledge, technology, and level of comfort with endoscopic techniques have allowed the use of combined and wholly endoscopic surgery for various sinonasal malignancies. Endoscopy of benign tumors allowed for decreased complication rates, reduction in brain retraction, and minimization of neurologic morbidity. Once surgeons were comfortable with resection of sinonasal and skull base benign tumors, attention shifted toward the use of endoscopic methods for sinonasal malignancy.
Although there has been a shift in interest away from traditional craniofacial resection (tCFR), use of endoscopy has not changed the principles of oncologic surgery. The primary goal is still complete resection of tumor with negative margins and minimization of morbidity. The use of endoscopy assists by providing superior visualization, higher magnification of vital structures, assurance of appropriate margins, avoidance of cosmetic deformity, and preservation of normal anatomy.
The endoscopic approach has encountered its own criticisms. Resection of the tumor often requires a piecemeal approach and may theoretically increase the chance of tumor seeding. Achievement of hemostasis, adequate visualization, and ability to perform reconstruction are additional barriers facing endoscopic approaches. Early results tend to be encouraging, however. A recent literature review found that endoscopy offers better quality of life outcomes than tCFR, and a second study found a decrease in morbidity when using the endoscopic approach compared with open tCFR. Although these studies are encouraging, further research is necessary when evaluating the endoscopic resection of malignant tumors.
Malignancies of the sinonasal tract and skull base encompass a heterogeneous, diverse group with respect to etiology, epidemiology, and histology, as classified by the World Health Organization. As such, treatment of disease must be specifically tailored to each disease process. Reporting on homogeneous skull base outcomes becomes difficult, especially because sinonasal malignancies are rare and thus outcomes often cannot be reported with sufficient power. Because squamous cell carcinoma is so heterogeneous in presentation and outcome, it has been excluded from this review.
Incidence and epidemiology of sinonasal and skull base cancer
Esthesioneuroblastoma
- •
Esthesioneuroblastoma, also known as olfactory neuroblastoma, is a rare tumor, constituting only 3% to 4% of all intranasal tumors.
- •
Esthesioneuroblastoma has a bimodal distribution, with peaks between ages 11 and 20 years and then ages 51 and 60 years.
The precise cause of esthesioneuroblastoma remains unclear, although the cell of origin is believed to be the specialized sensory neuroepithelial olfactory cells normally found in the upper part of the nasal cavity, which includes the superior nasal concha, the upper part of the septum, the roof of the nose, and the cribriform plate of the ethmoid.
Sinonasal Melanoma
- •
Mucosal melanoma accounted for only 1.3% of 85,000 cases of patients with melanoma during a 10-year period as reported by the National Cancer Data Base.
- •
The incidence of mucosal melanoma differs between geographic and racial boundaries, being particularly common in Japan.
- •
Of those patients with mucosal melanoma, 55% of lesions were found in the head and neck.
- •
Mucosal melanoma of the head and neck region has a peak incidence in patients aged 60 to 80 years, with a mean age of presentation of 64.3 years.
The prognosis of patients with sinonasal melanoma is poor. Five-year survival rates range from 14% to 45%. The nasal cavity is the most common site of origin, followed by maxillary and ethmoid sinuses. Most patients with mucosal melanoma are asymptomatic, allowing for insidious growth before discovery. Although most patients present without metastasis, one-third of all patients will eventually develop regional or distant metastasis; median time to death after distant metastasis is 3 months.
Nasopharyngeal Carcinoma (NPC)
- •
In the United States, nasopharyngeal carcinoma (NPC) is rare, with an incidence of less than 1 per 100,000 person-years.
- •
NPC has a distinct geographic and ethnic variation, being highly endemic to the Cantonese living in the central region of Guangdong Province in southern China.
- •
The male-to-female ratio is 2:1.
- •
NPC has a bimodal age distribution, with the first peak occurring in late childhood and a second peak occurring between people aged 50 to 60 years.
- •
Risk factors for NPC include high levels of Epstein-Barr virus (EBV) antibody titers, family history of NPC, consumption of salt-preserved fish, cigarette smoking, and occupational exposure to formaldehyde and wood dust.
Other than dietary modification, however, no definitive preventative measures have been published. NPC is thought to arise from the epithelial lining of the nasopharynx. The World Health Organization classifies NPC into 3 different types based on degree of differentiation on histopathology ( Table 1 ).
| Stage | Histopathology |
|---|---|
| I | Keratinizing squamous cell carcinoma |
| II | Nonkeratinizing carcinoma |
| III | Basaloid squamous cell carcinoma |
Sinonasal Adenocarcinoma (SNAC)
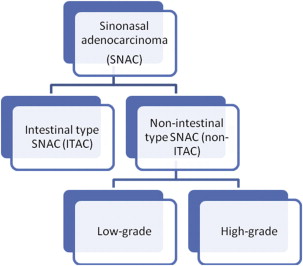
Sinonasal adenocarcinoma (SNAC) comprises 11.4% of all sinonasal tumors and refers to one of several types of tumors. SNAC may be further subdivided into intestinal-type adenocarcinoma (ITAC) and non–intestinal-type adenocarcinoma (non-ITAC), which can be further subdivided into low- and high-grade types ( Fig. 1 ).
Sinonasal ITAC
Sinonasal ITAC actually consists of a heterogeneous mix of tumors that may be further classified, as published by Barnes ( Table 2 ). Each subtype has its own epidemiology, outcomes, and clinically significant differences that are beyond the scope of this article. In general, the prognosis of SNAC is poor, with a 5-year survival between 20% and 50%.
- •
ITAC has been closely related to occupational exposure to wood and leather dust in many countries, sometimes presenting up to 40 years after exposure.
- •
Workers in the wood furniture–making industries have up to 500 times the risk of developing ITAC as those in the general population. This occupational exposure may also be the reason why ITAC affects males up to 3 times more often than females, with a mean age of presentation at 65 years old.
| Barnes | Klesinsasser and Schroede | 3-Year Cumulative Survival |
|---|---|---|
| Papillary | PTCC – I | 82% |
| Colonic | PTCC – II | 54% |
| Solid | PTCC – III | 36% |
| Mucinous | Alveolar goblet | 48% |
| Signet ring | 0% | |
| Mixed | Transitional | 71% |
The theory that ITAC is caused by particulate matter is further corroborated by evidence that the middle and lower turbinates are most affected. Definitive carcinogenic cause for ITAC, however, remains to be discovered.
Sinonasal Non-ITAC
Sinonasal non-ITAC is further subdivided into low-grade and high-grade subtypes, with distinguishing characteristics for each. High-grade non-ITACs are usually marked by increased cytologic atypia, necrosis of adjacent tissue, and higher degrees of mitotic activity.
- •
High-grade non-ITACs have a more rapid course, with a 3-year survival of 20%, whereas low-grade tumors have excellent prognosis, with 5-year survival of up to 85%.
- •
Anatomic location of non-ITAC also differs, with high-grade tumors mainly presenting in the maxillary sinus, whereas low-grade ITAC present most commonly in the nasal cavity, followed by the ethmoid and maxillary sinuses.
Sinonasal Undifferentiated Carcinoma (SNUC)
Sinonasal undifferentiated carcinoma (SNUC) is a recently recognized, rapidly progressive pathologic entity.
- •
First described in 1986, its median survival time was first reported at 4 months at the time of diagnosis. Since then, survival time has advanced to a still-dismal 1 year from the time of diagnosis.
- •
The cause of SNUC remains unknown, especially because SNUC has no association with the EBV.
- •
Median age of SNUC at diagnosis has been reported to be 50 to 57 years, with an age range of 20 to 84 years.
- •
Poor prognostic factors include dural invasion and orbital involvement at the time of diagnosis.
Incidence and epidemiology of sinonasal and skull base cancer
Esthesioneuroblastoma
- •
Esthesioneuroblastoma, also known as olfactory neuroblastoma, is a rare tumor, constituting only 3% to 4% of all intranasal tumors.
- •
Esthesioneuroblastoma has a bimodal distribution, with peaks between ages 11 and 20 years and then ages 51 and 60 years.
The precise cause of esthesioneuroblastoma remains unclear, although the cell of origin is believed to be the specialized sensory neuroepithelial olfactory cells normally found in the upper part of the nasal cavity, which includes the superior nasal concha, the upper part of the septum, the roof of the nose, and the cribriform plate of the ethmoid.
Sinonasal Melanoma
- •
Mucosal melanoma accounted for only 1.3% of 85,000 cases of patients with melanoma during a 10-year period as reported by the National Cancer Data Base.
- •
The incidence of mucosal melanoma differs between geographic and racial boundaries, being particularly common in Japan.
- •
Of those patients with mucosal melanoma, 55% of lesions were found in the head and neck.
- •
Mucosal melanoma of the head and neck region has a peak incidence in patients aged 60 to 80 years, with a mean age of presentation of 64.3 years.
The prognosis of patients with sinonasal melanoma is poor. Five-year survival rates range from 14% to 45%. The nasal cavity is the most common site of origin, followed by maxillary and ethmoid sinuses. Most patients with mucosal melanoma are asymptomatic, allowing for insidious growth before discovery. Although most patients present without metastasis, one-third of all patients will eventually develop regional or distant metastasis; median time to death after distant metastasis is 3 months.
Nasopharyngeal Carcinoma (NPC)
- •
In the United States, nasopharyngeal carcinoma (NPC) is rare, with an incidence of less than 1 per 100,000 person-years.
- •
NPC has a distinct geographic and ethnic variation, being highly endemic to the Cantonese living in the central region of Guangdong Province in southern China.
- •
The male-to-female ratio is 2:1.
- •
NPC has a bimodal age distribution, with the first peak occurring in late childhood and a second peak occurring between people aged 50 to 60 years.
- •
Risk factors for NPC include high levels of Epstein-Barr virus (EBV) antibody titers, family history of NPC, consumption of salt-preserved fish, cigarette smoking, and occupational exposure to formaldehyde and wood dust.
Other than dietary modification, however, no definitive preventative measures have been published. NPC is thought to arise from the epithelial lining of the nasopharynx. The World Health Organization classifies NPC into 3 different types based on degree of differentiation on histopathology ( Table 1 ).
| Stage | Histopathology |
|---|---|
| I | Keratinizing squamous cell carcinoma |
| II | Nonkeratinizing carcinoma |
| III | Basaloid squamous cell carcinoma |
Sinonasal Adenocarcinoma (SNAC)
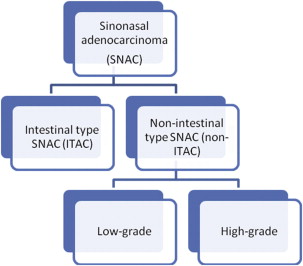
Sinonasal adenocarcinoma (SNAC) comprises 11.4% of all sinonasal tumors and refers to one of several types of tumors. SNAC may be further subdivided into intestinal-type adenocarcinoma (ITAC) and non–intestinal-type adenocarcinoma (non-ITAC), which can be further subdivided into low- and high-grade types ( Fig. 1 ).
Sinonasal ITAC
Sinonasal ITAC actually consists of a heterogeneous mix of tumors that may be further classified, as published by Barnes ( Table 2 ). Each subtype has its own epidemiology, outcomes, and clinically significant differences that are beyond the scope of this article. In general, the prognosis of SNAC is poor, with a 5-year survival between 20% and 50%.
- •
ITAC has been closely related to occupational exposure to wood and leather dust in many countries, sometimes presenting up to 40 years after exposure.
- •
Workers in the wood furniture–making industries have up to 500 times the risk of developing ITAC as those in the general population. This occupational exposure may also be the reason why ITAC affects males up to 3 times more often than females, with a mean age of presentation at 65 years old.
| Barnes | Klesinsasser and Schroede | 3-Year Cumulative Survival |
|---|---|---|
| Papillary | PTCC – I | 82% |
| Colonic | PTCC – II | 54% |
| Solid | PTCC – III | 36% |
| Mucinous | Alveolar goblet | 48% |
| Signet ring | 0% | |
| Mixed | Transitional | 71% |
The theory that ITAC is caused by particulate matter is further corroborated by evidence that the middle and lower turbinates are most affected. Definitive carcinogenic cause for ITAC, however, remains to be discovered.
Sinonasal Non-ITAC
Sinonasal non-ITAC is further subdivided into low-grade and high-grade subtypes, with distinguishing characteristics for each. High-grade non-ITACs are usually marked by increased cytologic atypia, necrosis of adjacent tissue, and higher degrees of mitotic activity.
- •
High-grade non-ITACs have a more rapid course, with a 3-year survival of 20%, whereas low-grade tumors have excellent prognosis, with 5-year survival of up to 85%.
- •
Anatomic location of non-ITAC also differs, with high-grade tumors mainly presenting in the maxillary sinus, whereas low-grade ITAC present most commonly in the nasal cavity, followed by the ethmoid and maxillary sinuses.
Sinonasal Undifferentiated Carcinoma (SNUC)
Sinonasal undifferentiated carcinoma (SNUC) is a recently recognized, rapidly progressive pathologic entity.
- •
First described in 1986, its median survival time was first reported at 4 months at the time of diagnosis. Since then, survival time has advanced to a still-dismal 1 year from the time of diagnosis.
- •
The cause of SNUC remains unknown, especially because SNUC has no association with the EBV.
- •
Median age of SNUC at diagnosis has been reported to be 50 to 57 years, with an age range of 20 to 84 years.
- •
Poor prognostic factors include dural invasion and orbital involvement at the time of diagnosis.
Evidence-based clinical assessment and diagnostic testing
Esthesioneuroblastoma Staging
There is no current consensus on the most accurate staging method of esthesioneuroblastoma. Staging was first proposed in 1976 by Kadish and colleagues and has since been modified by Morita and colleagues to divide the malignancy into 4 subtypes based on metastasis ( Table 3 ). Other staging methods requiring various procedures have been previously described. Biller and colleagues proposed a staging system that required craniotomy, Dulguerov and Calcaterra described a staging system that required imaging ( Table 4 ), and Hyams described a staging system requiring histopathologic specimens. Other authors have argued that combining 1 or more of these staging systems can yield better predictions for patient outcomes than any one of those staging systems alone.
| Stage | Extension |
|---|---|
| A | Tumor limited to the nasal cavity |
| B | Tumor involving the nasal and paranasal sinuses |
| C | Tumor extending beyond the nasal and paranasal sinuses, including involvement of the cribriform plate, base of the skull, orbit cavity, or intracranial cavity |
| D | Tumor with metastasis to cervical nodes or distant sites |
| Type | Extension |
|---|---|
| T1 | Tumor involving the nasal cavity and/or paranasal sinuses (excluding the sphenoid sinus), sparing the most superior ethmoidal cells |
| T2 | Tumor involving the nasal cavity and/or paranasal sinuses (including the sphenoid sinus) with extension to, or erosion of, the cribriform plate |
| T3 | Tumor extending into the orbit or protruding into the anterior cranial fossa, without dural invasion |
| T4 | Tumor involving the brain |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


