Evaluation of the Vestibular System
Conrad Wall III
Richard F. Lewis
Steven D. Rauch
Portions of this chapter were adapted from Wall III C. The sinusoidal harmonic acceleration rotary chair test: theoretical and clinical basis. In: Arenberg IK, ed. Dizziness and Balance Disorders: An Interdisciplinary Approach to Diagnosis Treatment and Rehabilitation. Amsterdam/New York: Kugler Publications, 1993:299-313; and Wall III C. Vestibular function and anatomy. In: Bailey BJ, Pillsbury HC, eds. Head & Neck Surgery—Otolaryngology, vol. 2. Philadelphia: J.B. Lippincott, 1993:1462-1472.
A basic understanding of the vestibular system is essential to the otologist, who is often called upon to evaluate symptoms of dizziness. Such symptoms may or may not be manifestations of ear disease. The otologist’s first task is to determine if the patient’s symptoms are otologic. Symptoms that involve a prominent illusory feeling of motion of oneself or the environment are particularly suggestive of a vestibular abnormality and can include a sense of rotation (most commonly), linear motion, or tilting. Symptoms of imbalance and dysequilibrium can be vestibular in origin, particularly if they are associated with illusory movement of the visual world (oscillopsia), but can also result from many types of neurologic disorders such as Parkinson’s disease or cerebellar degeneration. Presyncopal symptoms, typically described as lightheadedness, are rarely due to vestibular dysfunction and usually result from insufficient cerebral perfusion. Finally, symptoms that are primarily cognitive, often described as a “foggy” or “remote” sensation, are unlikely to be vestibular and often result from anxiety, hyperventilation, or related disorders.
Only a limited number of vestibulopathies are managed surgically, and these surgical approaches can be divided into two categories: procedures that correct a specific pathologic abnormality and ablative procedures that eliminate fluctuations in vestibular function. The former category includes perilymph fistula surgery, canal plugging for superior canal dehiscence or intractable benign positional vertigo, endolymphatic shunting for Meniere’s disease, acoustic neuroma resection, and, possibly, microvascular decompression of the eighth cranial nerve. The latter category includes labyrinthectomy, vestibular (or ampullary) nerve section, and gentamicin labyrinthectomy. The indications for these different procedures are discussed elsewhere in this volume. It should be stressed that ablative procedures should only be considered when there is clear evidence of spontaneous fluctuations in vestibular function, because their purpose is to eliminate these fluctuations and thereby promote central compensation. Symptoms of vestibular insufficiency, such as transient dizziness and imbalance provoked by rapid head motion or visual stimulation, reflect physiologic activation of a static vestibular deficit and hence are not an indication for an ablative procedure.
This chapter is divided into three sections. First, we present an overview of the organization and function of the vestibular system, relating these features to common vestibular symptoms. We then summarize the methods used during the physical examination to assess the patient with vestibular symptomatology. Finally, we describe the different types of quantitative vestibular testing and indicate how vestibular testing can aid in diagnosis and surgical decision making.
ORGANIZATION AND FUNCTION OF THE VESTIBULAR SYSTEM
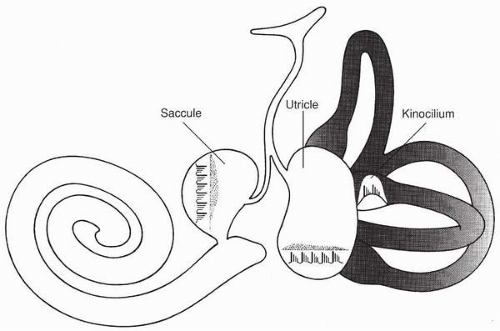
The vestibular system senses head motion and orientation (with respect to gravity) and provides information to the brain that is used to stabilize images on the retina and to maintain balance and spatial orientation. Because humans make complex motions in a three-dimensional world, five sensors in each inner ear are required to accurately measure these movements. The three semicircular canals (superior, posterior, and lateral) detect angular acceleration, whereas the two otolith organs (saccule and utricle) detect linear acceleration and gravity. Each sensor has its own bundle of nerve fibers that join to form one nerve before reaching the brain. Figure 5.1 shows the motion-detecting portion of a human left inner ear. Not shown are nerve fibers that attach to each of the five detectors and join together in a region near Scarpa’s ganglion (SG) to form the vestibular portion of the eighth nerve. Each semicircular canal responds maximally
to head rotations that are in the plane of the canal. The three canals are aligned so that they are approximately perpendicular to each other. The two otolith organs are approximately planar and are mutually perpendicular. Each otolith organ has a multitude of sensors that are maximally sensitive to linear accelerations in the plane of the organ. The right and left inner ear structures are arranged as mirror images of each other.
to head rotations that are in the plane of the canal. The three canals are aligned so that they are approximately perpendicular to each other. The two otolith organs are approximately planar and are mutually perpendicular. Each otolith organ has a multitude of sensors that are maximally sensitive to linear accelerations in the plane of the organ. The right and left inner ear structures are arranged as mirror images of each other.
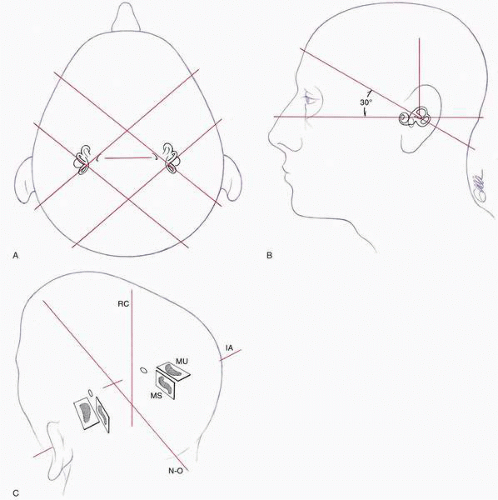
The geometrical layout of the six semicircular canals is shown in Figure 5.2A and B. Both lateral semicircular canals lie in the same plane, which is tilted approximately 30 degrees from the horizontal and runs parallel to a line drawn between the external auditory canal and the outer canthus of the eye. The four vertical canals lie in planes that are roughly at right angles to the plane of the horizontal canal pair. The superior vertical canal on one side is nearly in the same plane as the posterior vertical canal on the other side. Thus the functional canal pairs are the right and left lateral canals, the right superior and the left posterior canals, and the right posterior and left superior semicircular canals. The neural signals from these pairs of canals converge in a synergistic way in the nervous system, which allows the system to function even in the case of a complete unilateral lesion. The otolith organs are paired in a similar way (Fig. 5.2C). The right and left utricles are in approximately the same plane as the right and left lateral semicircular canals. The right and left saccules are in a plane that is approximately perpendicular to the plane of the utricle.
For both the canals and otolith organs, head acceleration causes a microscopic deflection of one or more microscopic masses in the inner ear. The deflection of the mass relative to its support structure is detected by sensory hair cells, which have their cell bodies attached to the support structure and their sensory hair bundles (stereocilia) connected to the mass. Motion of the head therefore causes deflection of these hair bundles, which in turn convert their microscopic displacements into electrical signals that are carried by nerve fibers to the brain. Inner ear disease or injury can break the chain of information transfer involving the masses, the hair cells, and the nerves. A malfunction of any element in this process will block the signal. Because there are many parallel transmission links, a significant fraction must be disabled for a true loss of useful sensory information to occur. Persons with this condition have severe vestibular hypofunction.
Semicircular Canals
In the semicircular canals the hair cells attach to the cupula, a gelatinous flap that completely seals one side of the widened region of the canal (the ampulla). The interior of the canal is filled by endolymph, a liquid with the density and viscosity of water. The membranous portion of the canal is attached to the temporal bone. When the head is turned, the membranous labyrinth moves with it, but the inertia of the endolymph tends to oppose the turning motion. This results in a pressure buildup across the cupula, which deflects it from its equilibrium position and bends the stereocilia of the hair cells, thereby transducing the head motion into a modulation of the firing rate of the vestibular nerve. For brief head movements, cupula distortion is proportional to head velocity, and the modulation of afferent activity in the vestibular nerve modulates with cupula distortion. Changes in the spontaneous firing rate of the vestibular nerve are
therefore proportional to head velocity. Hence it is not surprising that changes in afferent activity appear closely related to subjective sensations of angular velocity (rotation), and to the velocity of the reflexive eye movements (nystagmus). For long-duration stimuli, such as those experienced while flying, dancing, or in clinical testing, the dynamics introduced by cupula distortion and by the transduction and encoding process become significant and often limit human performance.
therefore proportional to head velocity. Hence it is not surprising that changes in afferent activity appear closely related to subjective sensations of angular velocity (rotation), and to the velocity of the reflexive eye movements (nystagmus). For long-duration stimuli, such as those experienced while flying, dancing, or in clinical testing, the dynamics introduced by cupula distortion and by the transduction and encoding process become significant and often limit human performance.
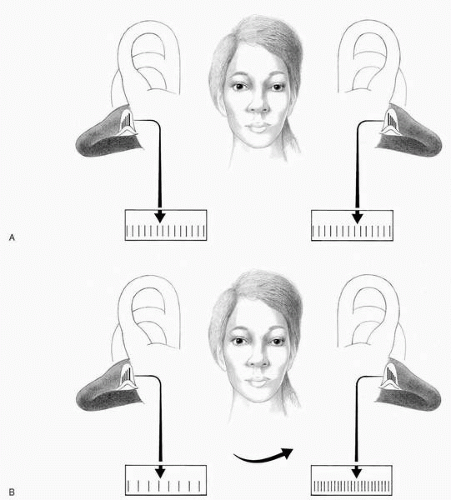
Pairs of canals in opposite ears combine into one functional “canal plane.” The six semicircular canals therefore combine into three functional canal planes, which are formed by the right and left lateral canals, the right superior and left posterior canals, and the left superior and right posterior canals. Angular rotation in any of these planes produces a maximum response from the two canals that are in that plane. The two canals in each plane operate in a pushpull manner such that a movement that maximally excites one member of a pair produces maximum inhibition in the other member of the pair (Fig. 5.3A and B).
Most vestibular afferents synapse on cells in the vestibular nucleus in the brainstem. The vestibular nucleus is involved
in the processing of both visual and vestibular information, and activity recorded from cells located there can differ markedly from afferent information received from the labyrinth. From the vestibular nucleus, multiple pathways have been identified that project to the cerebral cortex, the cerebellum, and the motor nuclei for the eye and skeletal muscles. The relationship among the vestibular system and the oculomotor and skeletal postural control systems is of particular interest in clinical evaluation.
in the processing of both visual and vestibular information, and activity recorded from cells located there can differ markedly from afferent information received from the labyrinth. From the vestibular nucleus, multiple pathways have been identified that project to the cerebral cortex, the cerebellum, and the motor nuclei for the eye and skeletal muscles. The relationship among the vestibular system and the oculomotor and skeletal postural control systems is of particular interest in clinical evaluation.
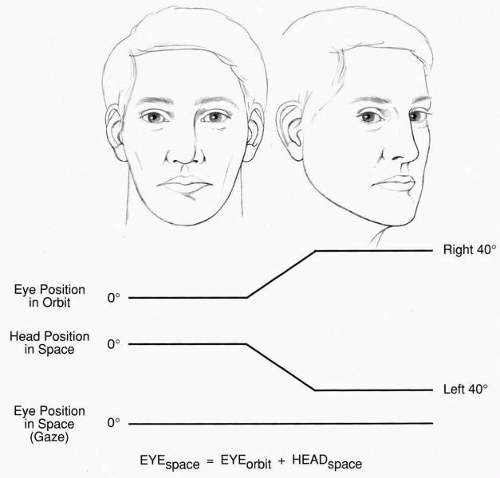
The vestibuloocular reflex (VOR) stabilizes the images of visual objects on the retina by producing eye movements that are compensatory to the head movement. Thus a motion of the head at 10 degrees per second to the right would produce an eye movement of 10 degrees per second to the left (Fig. 5.4). Measurement of reflexive eye movements resulting from rotation and caloric (thermal) stimulation of the semicircular canals is the primary clinical means of evaluating the status of the human vestibular system, because nerve recording
is not feasible. During rotation, vestibular information reaches the motor nuclei of the eye muscles to produce compensatory eye movements, which aid in retinal image stabilization. When angular motions are large, the oculomotor system generates quick movements that recenter the eyes, resulting in the slow-quick, slow-quick motions of the eye that are called nystagmus (Greek nystagmos, “head nodding while drowsy”). By convention, nystagmus is said to “beat” in the direction of the fast phase. Nystagmic eye movements can also be elicited by visual stimulation, such as by watching a field of moving stripes (optokinetic nystagmus).
is not feasible. During rotation, vestibular information reaches the motor nuclei of the eye muscles to produce compensatory eye movements, which aid in retinal image stabilization. When angular motions are large, the oculomotor system generates quick movements that recenter the eyes, resulting in the slow-quick, slow-quick motions of the eye that are called nystagmus (Greek nystagmos, “head nodding while drowsy”). By convention, nystagmus is said to “beat” in the direction of the fast phase. Nystagmic eye movements can also be elicited by visual stimulation, such as by watching a field of moving stripes (optokinetic nystagmus).
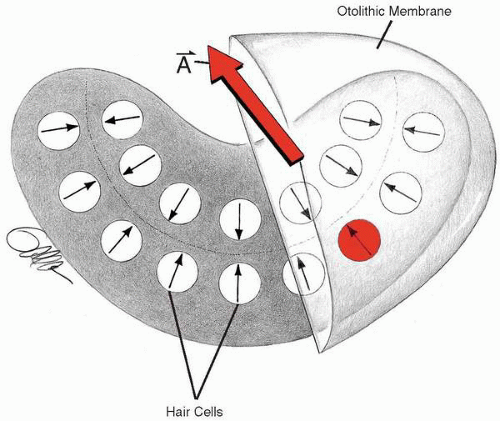
Otolith Organs
In the otolith organs (utricle and saccule), calcium carbonate crystals known as otoconia are embedded in a gelatinous supporting substrate called the otolithic membrane. Both linear acceleration and changes in the orientation of the head, with respect to gravity, shift the otolith membrane and distort the stereocilia of the hair cells that connect to the membrane. The arrangement of sensory hair cells in one otolith organ tends to be laid out in a roughly planar organization. These basic features are illustrated in a simplified diagram of an otolith organ, shown in Figure 5.5. In the diagram each of the sensory hair cells has a polarization vector with a small arrow indicating its direction of maximal excitation in the plane. The large arrow at the top of the otolithic mass represents a linear acceleration that deflects the otolith mass in the direction of the arrow. Thus the hair cells that have polarization vectors aligned with that arrow and in the same direction are excited maximally, whereas hair cells having polarization vectors that are at right angles to the acceleration are not stimulated at all. It is from an array of these hair cells that the brain is able to estimate the magnitude and direction of a linear acceleration. The right and left otolith organs, like semicircular canals, exhibit a mirror symmetry around the sagittal plane.
Utricular and saccular afferents project primarily to the inferior and medial vestibular nuclei. Secondary fibers then
carry the otolith information rostrally to ocular motor nuclei, cerebral cortex, and cerebellum and caudally to the spinal levels. Stimulation of the otoliths is known to produce compensatory eye movements. In the absence of rotational cues from the canals, lateral or vertical acceleration causes the eyes to deviate in a direction opposite to the acceleration (referred to as the linear VOR). In addition, head tilts around the nasooccipital axis produce a static torsional motion of the eyes in the opposite direction. These movements, called ocular counterrolling, have been used as an index of otolithic response.
carry the otolith information rostrally to ocular motor nuclei, cerebral cortex, and cerebellum and caudally to the spinal levels. Stimulation of the otoliths is known to produce compensatory eye movements. In the absence of rotational cues from the canals, lateral or vertical acceleration causes the eyes to deviate in a direction opposite to the acceleration (referred to as the linear VOR). In addition, head tilts around the nasooccipital axis produce a static torsional motion of the eyes in the opposite direction. These movements, called ocular counterrolling, have been used as an index of otolithic response.
Vestibular Compensation
How well the central vestibular and ocular motor systems readjust following a partial or total unilateral peripheral insult is an important factor of the recovery to several otologic medical and surgical treatments. Under normal conditions, with two intact ears, there is a near balance of tonic activity from the right and left vestibular nerves. This tonic activity bombards the vestibular nuclei, and the total activity available to drive the ocular motor system can be thought of as the difference in activity between the two sides. Under normal conditions, this difference is close to zero. A unilateral insult or lesion on one side tends to reduce the amount of tonic activity from that side and causes an imbalance that can result in spontaneous nystagmus and a subjective sense of motion. This central nervous system has the potential of correcting the imbalance over time, but the degree of correction varies among individuals. Thus one criterion for “successful” treatment will depend upon the individual patient’s ability to make the desired compensation. One approach to accelerate the compensation process is to use a rehabilitation protocol in which patients make voluntary movements of the body, head, and eyes as soon as it is practical after a treatment has been given. Although the vestibular end organs operate using the principle of mirror symmetry, explained previously, there is some evidence that suggests that even in cases of complete vestibular compensation the input from just one ear does not perfectly replace the function of two ears (1).
CLINICAL EXAMINATION
There are four principal components to the clinical examination of patients with vestibular disorders: (i) vestibular tone; (ii) vestibular gain; (iii) positional nystagmus; and (iv) nonvestibular oculomotor function. Vestibular tone is assessed by noting the presence of spontaneous nystagmus (i.e., nystagmus with the head upright and stationary and the eyes centered in the orbits). This should be evaluated in a lit room in the presence of visual fixation and with fixation removed (i.e., with Frenzel glasses). In general, unilateral peripheral vestibular deficits produce a mixed horizontal-torsional nystagmus,
with slow phases directed toward the involved ear that are suppressed by visual fixation. In contrast, central vestibular disorders can produce a variety of nystagmoid eye movements (such as vertical or torsional) that are not suppressed by fixation. Central disorders only rarely result in a horizontal-torsional nystagmus that can mimic a peripheral lesion. If any spontaneous nystagmus is present, it typically will vary with orbital eye position, increasing in magnitude with gaze in the direction of the quick phases (Alexander’s law). Vestibular tone asymmetry can be amplified by repetitively shaking the head side to side, which produces a horizontal nystagmus with slow phases directed toward the side of the lesion. With several vestibular disorders, a tone imbalance (and associated nystagmus) can be provoked by specific stimuli, such as Valsalva maneuvers (with perilymph fistula, canal dehiscence, or Chiari malformations); modification of pressure in the middle ear (Hennebert’s sign, with perilymph fistula, canal dehiscence, or Meniere’s disease); or hyperventilation (with central or peripheral demyelinative lesions such as multiple sclerosis or microvascular compression of the vestibular nerve).
with slow phases directed toward the involved ear that are suppressed by visual fixation. In contrast, central vestibular disorders can produce a variety of nystagmoid eye movements (such as vertical or torsional) that are not suppressed by fixation. Central disorders only rarely result in a horizontal-torsional nystagmus that can mimic a peripheral lesion. If any spontaneous nystagmus is present, it typically will vary with orbital eye position, increasing in magnitude with gaze in the direction of the quick phases (Alexander’s law). Vestibular tone asymmetry can be amplified by repetitively shaking the head side to side, which produces a horizontal nystagmus with slow phases directed toward the side of the lesion. With several vestibular disorders, a tone imbalance (and associated nystagmus) can be provoked by specific stimuli, such as Valsalva maneuvers (with perilymph fistula, canal dehiscence, or Chiari malformations); modification of pressure in the middle ear (Hennebert’s sign, with perilymph fistula, canal dehiscence, or Meniere’s disease); or hyperventilation (with central or peripheral demyelinative lesions such as multiple sclerosis or microvascular compression of the vestibular nerve).
Vestibular gain, defined as eye velocity divided by head velocity, is normally close to one, so the eyes remain stationary in space when the head moves. This gain can be assessed by three methods, all of which look at eye position during side-to-side head movement.
Dynamic E test. Visual acuity is measured with the head stationary and also with the head passively oscillated. Normally, visual acuity is minimally affected by head motion. If vestibular gain is reduced, however, the eyes move in space when the head is oscillated (abnormal gain). Visual acuity during head motion is degraded by two or more lines on the Snellen chart.
Head thrust test. The patient is instructed to fix his/her gaze on the examiner’s nose. The patient’s head is then rapidly thrust approximately 20 degrees to one side or the other. If the VOR is normal, the eyes remain stationary on the nose during the head thrust. If the gain is abnormal, the eyes move during the head motion toward the affected side and then make a readily observable “reflection saccade” to bring gaze back to the nose.
Use of ophthalmoscope. The optic disk is visualized with an ophthalmoscope while the head is turned side to side. If the vestibular gain is normal, the eye (and optic disk) remains stationary during head motion. If the gain is reduced, the disk moves in the opposite direction of the head, because the disk is behind the center of rotation of the eye. Vestibular gain tends to be markedly reduced when the vestibular system is damaged bilaterally. Such bilateral damage is usually peripheral (e.g., with aminoglycoside toxicity) but can be central (e.g., with Wernicke’s disease). Asymmetries in gain occur with unilateral lesions and can be deduced with the head thrust test, because the gain is lower when the head is rotated toward the bad ear (Ewald’s second law). Increases in gain are rare; their occurrence usually reflects disease in the vestibulocerebellum, particularly the flocculus and paraflocculus.
Positional nystagmus is elicited with the Dix-Hallpike maneuver, whereby the patient’s head is turned 45 degrees to the right or left and is then rapidly moved backward so that the head is tilted 30 degrees below the horizontal. This maneuver provokes vertigo and nystagmus if the subject’s disorder is activated by head motion with respect to gravity. The most common positional disorder is benign positional vertigo (BPV) involving the posterior canal, which produces an upbeat, torsional nystagmus when the affected ear is placed undermost. Less common variants of BPV are in the superior canal (producing a downbeat, torsional nystagmus) or lateral canal (producing a direction-changing geotropic horizontal nystagmus). Positional nystagmus can occur with other peripheral disorders, such as perilymph fistula and Meniere’s disease, and can also occur with central disorders, such as the static downbeat nystagmus associated with lesions of the cerebellar nodulus.
In addition to the specific tests described earlier, clinical examination of a patient with vestibular symptoms should also include a careful assessment of nonvestibular oculomotor function. A complete discussion is beyond the scope of this textbook but generally includes examination of fixation, gaze holding, saccades, pursuit, and optokinetic and vergence eye movements (2). A thorough neurologic and otologic examination also contributes to the clinical assessment of vestibular disorders.
FUNCTIONAL VESTIBULAR TESTING
Vestibular testing is used to identify the peripheral and central abnormalities of vestibular function that can occur with diseases that affect the labyrinth, the eighth nerve, or the brain. Vestibular tests in isolation are not typically diagnostic, but rather are used in conjunction with other clinical information such as the patient history and the physical examination to reach a meaningful diagnosis. Three options will be described: (i) the basic electronystagmography (ENG) test battery, (ii) postural stability tests, and (iii) rotation about the earth vertical. Each of these tests can be affected by nonvestibular sensory or motor systems in potentially complex ways, and therefore each individual test has somewhat limited value. When several tests are analyzed in concert, however, the results may provide convergent data that allow a specific diagnosis to be reached. An American National Standard for the ENG test battery (ANSI S-3.45) (3) has recently been approved by members of the consortium of users, including the American Academy of Otolaryngology—Head & Neck Surgery (AAO-HNS). Having wider access to results from standardized procedures will become increasingly more important as the medical world becomes
more linked—for example, by the computer internet. Accordingly, the ENG test battery will be presented as described in ANSI S-3.45.
more linked—for example, by the computer internet. Accordingly, the ENG test battery will be presented as described in ANSI S-3.45.
ENG Test Battery
The ENG test battery, currently considered to be the standard of practice, consists of the calibration of the electrooculogram (EOG); a test of the saccadic eye movement system; a search for spontaneous or gaze-evoked nystagmus; a test of pursuit eye movements; a search for nystagmus that occurs during or after the patient is positioned in a manner that is apt to provoke nystagmus; and the bithermal, binaural caloric test.