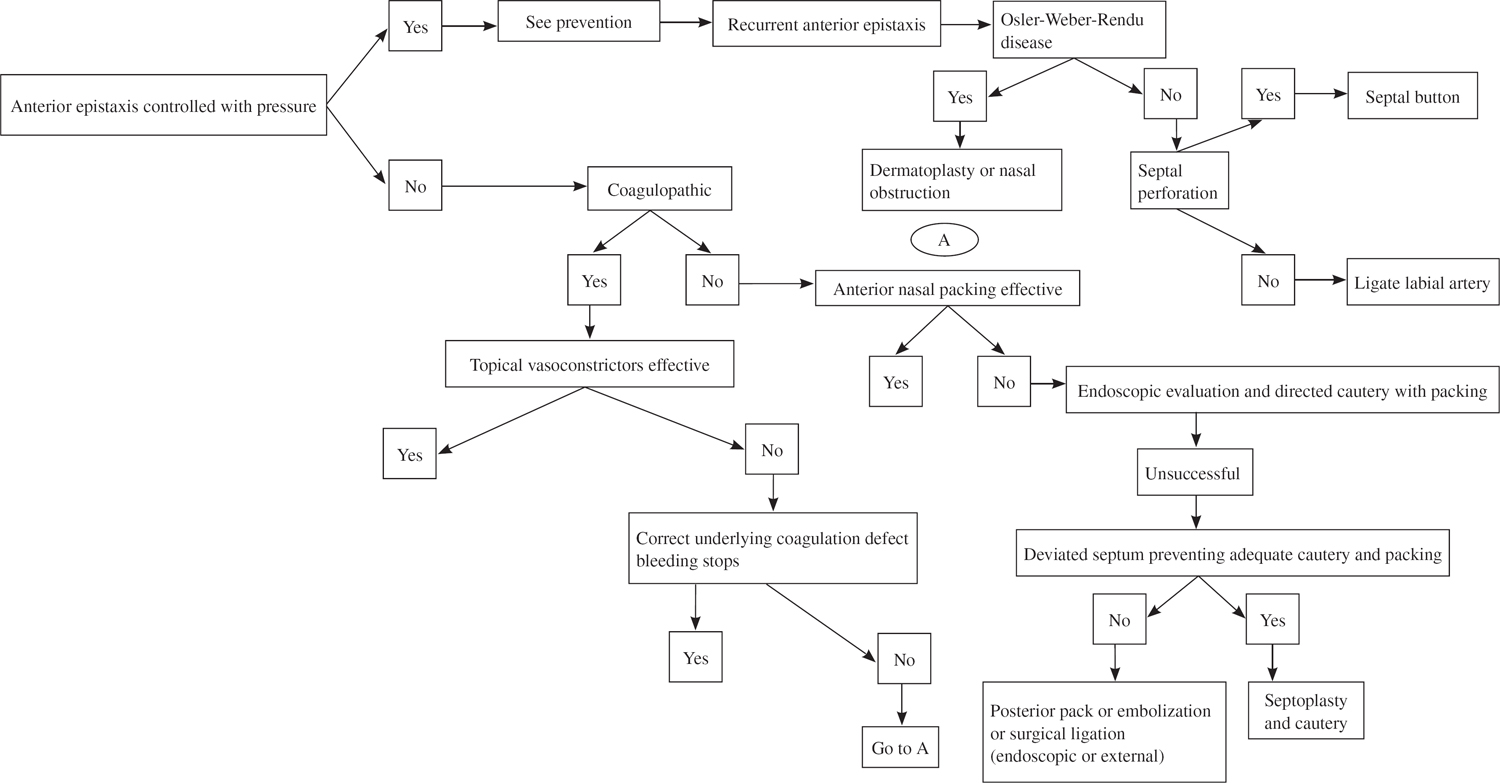
44 Epistaxis Control Epistaxis is common. Patients are often anxious and fearful that the bleeding represents infection, tumor, or impending stroke or that it may lead to exsanguination. Fortunately, epistaxis usually resolves with simple first aid measures such as anterior digital pressure or anterior packing. More problematic is epistaxis from a posterior site or beneath or behind a septal deflection. Death is rare, but morbidity is high, particularly in the older patient.1,2 This review will discuss the analysis and control of predisposing conditions, nasal packing, and surgical interventions and embolization. The control of epistaxis is a stepwise series of increasingly elaborate interventions until control is achieved. Patients should be informed that there is no guarantee of control with a particular intervention but reassured that you will continue to be available to direct care until the bleeding stops. Epistaxis is a common problem afflicting both the young and old, with those over age 40 increasingly likely to require hospital admission. Patients ages 20 to 49 are more likely to be male; those over age 50 are equally distributed between the sexes. The decreased incidence of female epistaxis in the younger age group has been attributed to a premenopausal protective effect, although the mechanism is unknown.1 Risk factors for epistaxis include coagulopathies, septal perforations, hypertension, and nasal trauma.2 Nasal trauma can range from nasal fracture to nose picking to the trauma of dry air administered through oxygen prongs. In the latter case, counseling the patient regarding nasal lubricants such as AYR gel (BF Ascher & Co., Lenexa, Kansas) and petroleum jelly or increased room humidity may prevent further bleeding. The initial work-up for epistaxis includes a history (Table 44.1) followed by a physical examination, including all vital signs, with special attention on significant hypertension. Many patients will demonstrate some hypertension, which is secondary to the anxiety of the situation and not causal. Laboratory studies are required only for recurrent or severe bleeding. These should include hematocrit, hemoglobin, and coagulation profiles. If bleeding is thought to be or has been profuse, then blood should be obtained for a type and cross. Patients initially packed and placed on a penicillin or a first-generation cephalosporin class of antibiotics may return with recurrent bleeding. In some cases, this is because this class of antibiotics can interfere with platelet function and may unmask a platelet abnormality in a patient who was previously compensated, thus leading to a perpetuation of bleeding, sometimes at additional, previously uninvolved sites. A repeat bleeding time and more elaborate coagulation work-up will aid in this diagnosis. The first step in the control of epistaxis is to protect the caregivers. This includes, at a minimum, gloves for all medical personnel and drapes for the patient. Face shields, overgowns, and hair protection are required in some situations. Prepare all materials to control the bleeding, including pledgets soaked in an anesthetic (i.e., 4% Xylocaine) combined with a vasoconstrictor (a few drops of 1:1000 epinephrine or equal parts 4% oxymetazoline). Next, instruct the patient to gently blow his or her nose free of all blood clots. (Occasionally, this can be assisted with directed suction.) Then one or several pledgets soaked in Xylocaine and oxymetazoline are inserted into the nostrils under direct vision. In most cases, the vasoconstrictive effects of oxymetazoline combined with the pressure from the pledgets will slow the bleeding substantially within 10 minutes and allow inspection and painless cautery and, if required, packing. Table 44.1 Important Inclusions in History for Patient with Epistaxis
Epidemiology
Directed History and Laboratory Examination
Control of Bleeding: Initial Encounter
Factors that aid in localizing site |
Side of bleeding, or predominant side |
Mostly anterior, posterior, or both |
Factors that predispose to bleeding |
Hypertension |
Coagulopathy |
Family history of bleeding |
Past episodes of bleeding |
Medications (especially: aspirin and nonsteroidal anti-inflammatories, warfarin, vitamin E, or chemotherapy; see Table 44.2 for a more complete listing) |
Trauma—history of |
Nasal steroid spray usage |
Nose picking |
Presence of septal perforation and date first noted |
Onset of bleeding |
Estimate of amount of blood loss |
Prevention
Patients with a history of anterior epistaxis should be taught first aid measures to employ if bleeding restarts, including appropriate anterior pressure, use of nasal lubricants, and avoidance of trauma, such as nose picking. Patients using prescribed nasal sprays should be directed to aim them laterally and not toward the septum and to stop the sprays if bleeding occurs.3 A Merocel (Xomed Inc., Jacksonville, Florida) sponge cut into several pieces and given to a patient with a history of anterior epistaxis may allow that patient to self-treat anterior epistaxis and avoid an emergency room visit. Recently, a device called NasalCEASE (Les Laboratoires Brothier, Nanterre Cedex, France), available in Europe as an over-the-counter product for 50 years, has become available in the United States. NasalCEASE is a specific calcium alginate product that has been shown to cause coagulation via platelet aggregation and plasmatic coagulation.4 The patient places the sterile pack in the nose for a half hour and then removes it. To date there are no reports of toxic shock syndrome associated with the product. Patients who are prone to nosebleeds should be apprised of the medications that can cause coagulopathy and promote bleeding (Table 44.2).
Endoscopic Evaluation and Management
Patients with an easily seen anterior site of bleeding can be effectively treated with digital pressure, vasoconstrictors, and directed cautery and packing, if required. For patients with recurrent or posterior bleeding, endoscopic assessment in an anesthetized and decongested state is optimal. The best chance of controlling epistaxis with the least intervention is the accurate visual localization of the bleeding before the nasal mucosa is traumatized with packing and cautery. Merocel packs can be trimmed to precise sizes to tamponade the bleeding and underlain with an absorbable collagen hemostatic material such as Helistat (Colla-Tech Inc., Plainsboro, New Jersey) or Avitene (Med Chem Products, Inc., Woburn, Massachusetts), which will not require removal. The mucosa will thus be protected from rebleeding when the nonabsorbable pack is removed. If the bleeding site can be accurately identified endoscopically, then cautery directed to the bleeding site is highly effective, and further packing may be unnecessary. The offending vessel may often be seen endoscopically as a raised bump protruding above the level of the mucous membrane. Gently touching it will produce bleeding, confirming this as the source. This may be accomplished in the office or emergency department; however, if endoscopically directed suction cautery is required, then the patient is best taken to the surgical suite for general anesthesia, as it is quite difficult to achieve the level of anesthesia or instrumentation required for suction cautery outside the operating room.
Table 44.2 Medications That Can Prolong Bleeding
Advil | BC Cold Powder | Congesprinin |
Alcohol | BC Powders | Cope |
Aleve | Brufen | Coricidin |
Alka-Seltzer | Buff-A-Com | Coumadin |
Anacin |



