Endoscopic surgery of the inner ear may be a useful, minimally invasive approach to remove pathologic lesions and yet retain inner ear function. Several different endoscopic inner ear surgical entry sites and strategies that may help to preserve otologic function are described. These endoscopic surgical method alternatives are based on temporal bone studies, prior literature, and clinical patient experiences. Endoscopic inner ear surgery is a challenging, but potentially very useful method to address inner ear problems.
Surgery of the inner ear remains an elusive goal. Intervention usually means loss of function. Even procedures that superficially invade the labyrinth may give rise to hearing loss. Nevertheless, successful procedures, such as stapedectomy and canal plugging, are performed, and function is preserved. Even with naturally occurring pathologies that destroy the otic capsule, such as cholesteatoma, function can be spared. However, the possibilities of traumatic hearing loss, tinnitus, and vertigo remain obstacles to progress towards more direct inner ear surgery.
Presently there are some patients with a relatively circumscribed otologic lesion, such as an erosive cholesteatoma or intralabyrinthine schwannoma, who nevertheless undergo a surgically destructive procedure of the entire inner ear. Currently methods of surgery were devised using the operating microscope as the enabling tool, which may limit preservation surgery. In addition, there is an ingrained belief in surgeons that opening of the labyrinth immediately leads to disabling or loss of all acoustic and vestibular function. Rather than chance a chronically debilitated ear as the surgical result, ablation surgery is chosen by the surgeon.
Recent advances in endoscopic technology have allowed for small diameter endoscope designs suitable for inner ear surgery. These endoscopes are narrow enough to fit through small openings into the otic capsule. They have optical and working channels and are the prototype surgical instruments for atraumatic entry into the inner ear. Completion of surgical goals without destroying the remaining anatomic content of the inner ear may be possible using micro-endoscopes.
Entry of endoscopes into the inner ear has already taken place. Endoscopic work has taken place as part of cochlear implant research. Microscopic endoscopes to research hair cell physiology are also in use. Research into stem cells for inner ear cell regeneration is progressing. These early attempts point towards a goal of directly operating on the inner ear to structurally remediate a patient’s medical problem.
Before reliable inner ear endoscopy outcomes can be expected in the future, much groundwork needs to be achieved. Understanding how to enter the inner ear with minimal or no anatomic inner ear trauma is one part of the groundwork. There are other aspects, such as degree of trauma induced, recovery from trauma, and so forth. In this article, temporal bone (TB) laboratory studies together with clinical experiences of endoscopes contribute to early understanding of surgical entry into the inner ear using the endoscope.
Materials and procedures
TB Laboratory
Multiple sites of entry into the human inner ear were explored. Cadaver TBs, which were either dry or bare, or formaldehyde fixed with attached tissue, were used. Specific endoscopic entry sites for the otic capsule were divided into 3 areas: cochlea, vestibule, and the semi-circular canals (SCC). These multiple sites were evaluated for their relative visual clarity, disruption to normal structures, realistic approach angle, and surgical work through simultaneous double-entry sites.
Multiple specialized instruments and surgical steps were used. Sialendoscopes (K. Storz Medical, Tuttlingen, Germany) with an outer diameter of 0.75 mm and 3000 pixels (model no. 11576) and a diameter of 1.1 mm and 6000 pixels (model no. 11573) were used; the angle for both endoscopes was 0°. The endoscopes are categorized by the manufacturer as semirigid for salivary cases and rigid for otology-type work. Forceps (K. Storz, model no. 11577ZJ) with 1.0 mm outer diameter and a 200-μm laser fiber (Lumenis Inc., Santa Clara, CA) were also tested. To simulate schwannoma tumors, small pieces of white modeling clay (Permaplast Clay, AMACO, Indianapolis, IN) were placed in the vestibule and then mock-resected using the endoscope, laser fiber, and forceps.
To achieve adequate surgical exposure, all cases required a canal wall down (CWD) mastoidectomy with removal of the incus and malleus bones. Next, routine microscope-assisted otologic drilling through the otic capsule bone with soft surgery technique was used as a preliminary step to gain access to the inner ear structures before endoscopy commenced.
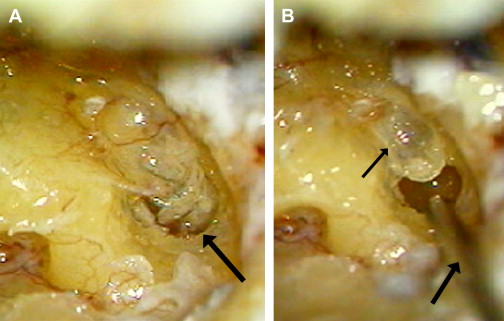
For the endoscopic surgical techniques, the Oval Window (OW) approach uses either footplate removal or a stapedotomy opening to access the vestibule; the endoscopic Extended-Oval Window (E-OW) approach gains wide exposure of the posterior vestibule through the fossula post-fenestram. In the E-OW approach, removing the stapes pyramid and stapedius muscle are followed by soft surgery techniques and the CO 2 laser over the postfenestram endosteum in a technique similar to laser stapedotomy ( Fig. 1 A, B ). The E-OW approach can be performed with or without prior removal of the stapes footplate. In the OW and E-OW approaches, perilymph was revealed and the endoscope entered the vestibular cistern under the footplate or fossula post fenestram.
The vestibular cistern fluid space was used to gain wide endoscopic visualization and access to all the vestibular structures in the OW and E-OW approaches. The vestibular cistern is a volume of vestibular perilymph space between the footplate area and the utriculosaccular structures. The saccule and utricle rest between 1 and 2 mm from the plane of the footplate. Because of the cistern space, there is adequate distance between the otic capsule and membranous structures to allow endoscopic entry without disrupting structures.
The endoscope was also used in the cochlear basal turn to guide a 30-gauge hypodermic needle (Becton Dickinson PrecisionGlide, Franklin Lakes, NJ) into the modiolus. The basal turn was opened by drilling away the anterior lip of the round window using soft surgery techniques. Then, the needle tip was visually guided to the modiolus using the endoscope. Fingertip pressure was sufficient to penetrate the bone with the needle into the desired modiolar position ( Fig. 2 ). The middle turn is preferred.
The SCCs were approached by soft surgery drilling techniques. In the initial step, the otic capsule bone was drilled, then the endosteum was gently removed, followed by entry of the endoscope and advancing toward the vestibule. The SCCs and ampullae have different diameters and therefore different endoscopes were gently used in each SCC to visualize structures and instruments. To disrupt as little anatomy as possible, soft surgery techniques were used.
Results
Table 1 provides an overview of the predicted surgical experience when using endoscopes to gain intralabyrinthine access directly into the cochlea and into the vestibule by OW/E-OW approaches. Each entry point is paired with the 2 endoscopic sizes tested. The technical and mechanical findings are listed, followed by the endoscopic visual findings to help the surgeon decide on a practical access point into the inner ear that visually targets the specific endolabyrinthine pathology at hand.
| Endoscopy Entry Point | Endoscope Size | Technical and Mechanical Findings | Visual Findings |
|---|---|---|---|
| Basal turn cochlea | 0.75 mm | Entry possible into ST and SV | WB: wide views of basal turn structures, ST, SV, modiolus, basal membrane; view in anterior direction for 3.5 mm beyond endos tip in ST |
| 1.1 mm | Entry into ST | ||
| Other | Cochleostomy 1 mm anterior to RW; forceps size (1 mm) necessitates entry into separate scala from endos, laser fiber placement simultaneously in same scala as endos; CWD-TM or TM with anteriorization of soft tissue ear canal for approach; posterior direction viewing angle limited by anterior ear canal | ||
| Middle turn cochlea | 0.75 mm | Entry into ST both directions | WB: both directions viewable, tightly turned ST and SV allow only 1 mm view beyond endos; with 1.1-mm endos, structures only seen in cross section; MCF approach views like those in basal turn findings |
| 1.10 mm | Too wide for single scala, ST/SV viewed simultaneously in cross section | ||
| Other | Posterior viewing angle limited by anterior ear canal; Superior aspects of basal and middle turns viewable by MCF approach | ||
| Apical turn cochlea | 0.75 mm/1.10 mm | No endoscopic viewing without uncapping of entire apical turn by removing tensor tympani muscle and bone; apical turn destroyed by endoscopy attempts | Structures of uncovered apical turn fully visible; visualization during endos contact with structures is destructive; not of practical clinical application presently |
| Other | Good approach angles from CWD-TM or TM with anteriorization of soft tissue ear canal | ||
| OW/E-OW | 0.75 mm/1.10 mm | Both endoscopes fit into OW/E-OW to enter vestibular cistern | WB: vestibular cistern gives wide views of entire V. Anterior view shows S, U, saccule-utricle interface, VA, anterior cochlear artery, S-SCC ampulla. Posterior view shows U, CC, P-SCC ampulla, H-SCC ampulla, P-SCC ampulla, posterior cochlear artery |
| Other | Multiple good approach angles from CWD-TM or TM with anteriorization of soft tissue ear canal; transcanal approach limited by constricted angulation of endos; SS technique |
Table 2 provides an overview of the predicted surgical experience when using endoscopes to gain intralabyrinthine access through the semi-circular canals.
| Endoscope Entry Point | Endoscope Size | Technical and Mechanical Findings | Endoscope Visual Findings |
|---|---|---|---|
| H-SCC Anterior limb | 0.75 mm | Good entry into bony canal after drilling access with SS; membranous canal not passable without avulsion | DB: view encompasses area of S and U, S-SCC anterior limb; WB: 0.75 mm shows membranous canal in cross section or folded as endos advances and avulsion occurs with advance of endos; ampulla with cupula seen with both 0.75-, 1.10-mm endos |
| 1.10 mm | Entry into ampulla after removal of bony SCC | ||
| Other | Good approach angle from CWU-TM for both endos | ||
| Posterior limb | 0.75 mm | Entry as for H-SCC anterior limb | Endos angled toward medial wall of vestibule; WB: utricle; DB: U and S areas |
| 1.10 mm | Entry into posterior V after removal of bony canal | ||
| Other | Good approach angle from CWU-TM for both endos | ||
| S-SCC Anterior limb | 0.75 mm | Good entry into bony canal after drilling access with SS; membraneous canal not passable without avulsion | Ampulla with cupula seen with both 0.75- and 1.10-mm endos; WB: beyond ampulla into U; DB: view encompasses area of footplate, hook of cochlear duct, SV, VA |
| 1.10 mm | Entry into ampulla after removal of bony SCC | ||
| Other | MCF approach angle for both endoscopes | ||
| CC/limb | 0.75 mm | CC accessible through limb of S-SCC, membraneous canal avulsed with advance of endos | WB: visualization of membranous S-SCC DB: CC leads to view of posterior vestibule, OW |
| 1.10 mm | Not accessible through S-SCC limb until drilled to CC | ||
| Other | Extreme MCF approach angle for both endoscopes, not practically useful at present | ||
| P-SCC Inferior limb | 0.75 mm | Entry into bony canal after drilling access with SS | WB: Good view of ampulla with cupula DB: cribriform area of nerve seen, posterior-most vestibule. |
| 1.10 mm | Accessible after P-SCC bony canal removed to ampulla | ||
| Other | CWU-TM with good approach angle | ||
| CC/limb | 0.75 mm | CC accessible through limb of P-SCC | WB: P-SCC limb enters into CC with membranous SCC seen DB: CC view of posterior vestibule |
| 1.10 mm | Not accessible through superior limb until drilled to common crus | ||
| Other | MCF approach angle for both endoscopes |
TB Laboratory
The dry- and wet-preserved TB study findings were consistent and their results are combined.
Cochlea
The basal and middle turns of the cochlea were accessible with both endoscope sizes, whereas the apical turn was too small for endoscopic entry (see Table 1 ).
In the basal turn, the 0.75-mm endoscope fitted both major scalae, but the 1.1-mm endoscope could be used only in the scala tympani. Simultaneous use of the endoscope and microforceps could only be performed in the basal turn and necessitated the use of both scalae with 1 instrument in each scala; patient use would be for a lesion straddling the 2 scalae. The laser fiber was useable simultaneously with both endoscope sizes within 1 scala. The major landmark structures of the cochlea, such as the stria vascularis, osseous spiral lamina, and modiolus, were clearly visualized ( Fig. 3 ). The modiolus was in direct view and accessible for surgical entry. The maximal clear viewing distance along the basal turn was 3.5 mm beyond the endoscope tip. Alternately, the middle cranial fossa (MCF) approach to the basal turn provided visual clarity as good as the transmastoid middle ear approach; however, the morbidity of an MCF craniotomy would be incurred in patient use.
In the middle cochlear turn, the 0.75-mm endoscope fitted into the individual scalae. However, the endoscope was relatively large and was traumatic to the cochlear structures to a point that would cause bleeding in a patient. The 1.1-mm endoscope was too wide to insert into the individual middle turn scalae; however, if it was abutted against a cross section of both scalae, a clear viewing distance of 2 mm was achieved.
For the apical turn, exposure was achieved by first removing the overlaying tensor tympani muscle and tendon. Once the apical turn was opened using soft surgery with the drill, only the microscope was useable, as the endoscopes were too wide to enter.
Vestibule
Two entry sites were useful for endoscopy of the labyrinthine vestibule: the OW area and the horizontal semi-circular canal (H-SCC; discussed in the next section) (see Tables 1 and 2 ).
For both approaches (OW and E-OW), the endoscopes fitted easily into the OW niche and into the openings created. Simultaneous instrumentation, with the endoscope and instruments in separate openings, was possible using both approaches.
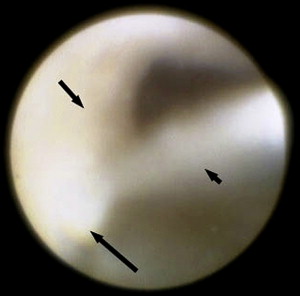
Both approaches were used to visualize the vestibule. With the OW approach, the anterior and middle portions of the vestibule were easily seen and revealed light reflections on the saccule, utricle, the vestibular aqueduct, the canal openings of the H-SCC, and the superior semi-circular canal (S-SCC) ( Fig. 4 ). The OW approach gave a wider view of the vestibule when enlarged in a posterior direction into the fossula post fenestram as an E-OW technique. The E-OW approach without removal of the footplate (ie, postfenestram only) allowed for endoscopic visualization and surgical work on the entire posterior vestibule ( Figs. 5 and 6 ).




