33 Endoscopic Skull Base Defect Repair Because of the technological advancements and a greater understanding of endonasal vascular anatomy, the endoscopic repair of skull base defects has undergone a progressive evolution over the past decade. The authors’ initial success with repairing cerebrospinal fluid (CSF) leaks encountered during sinus surgery has evolved to the repair of large defects associated with tumor resection in the anterior, middle, and posterior cranial fossae. Endoscopic techniques were successful because of maintenance of the principles of open skull base reconstruction: (1) multilayer closure, (2) preservation of neurovascular structures, and (3) utilization of vascularized tissue. CSF leak repair has advanced greatly since the first reported repair by Dandy, who in 1926 sealed a cranionasal fistula using a frontal craniotomy approach. Ultimately, improved instrumentation, enhanced resolution of imaging, and miniaturization of instruments allowed for endoscopic repair of CSF leaks by Wigand in 1981.1 In his report, he described the use of endoscopes to seal a small CSF leak using fibrin glue. Over the past 20 years, the minimally invasive endoscopic approach has gained widespread acceptance and become the standard of care because of its high success rate and lower morbidity than traditional intracranial techniques.2–5 Skull base defects are secondary to traumatic or nontraumatic etiology. Nontraumatic causes are predominantly spontaneous CSF leaks and skull base erosion secondary to tumor. Traumatic leaks are a result of blunt or penetrating trauma or surgical procedures involving the skull base. Majority of the nontraumatic CSF leaks are of spontaneous or idiopathic origin, where no other discernible etiology is present, with a reported frequency of 15 to 23%.6,7 These are primarily located at the cribriform plate and lateral recess of the sphenoid sinus, but can also be noted at multiple sites approximately 30% of the time.8–10 The pathophysiology is thought to involve an elevation in intracranial pressure, exerting a constant pulsatile force at weakened sites in the skull base. Because of the elevated pressures, spontaneous CSF leaks tend to have the highest recurrence rate, which stresses the importance of CSF pressure control at the time of surgical repair. Congenital causes are extremely rare and difficult to repair. They are often caused by skull base malformation, allowing the herniation of brain and meninges through the defect into the sinonasal cavity. The most common location is the foramen cecum, as noted by Woodworth et al, in 63% of the cases.11 Historically accidental trauma was the most common etiology of CSF leaks, occurring in 1 to 3% of all cranial head injuries.9 These injuries were often classified as penetrating versus nonpenetrating, and depending on the extent of injuries could present as either an acute leak upon presentation or in a delayed fashion. Fracture patterns can be focal or diffuse, with patients most commonly presenting with cribriform plate (23%) and ethmoid skull base defects (20%), while 35% of patients have multiple sites of injury.12 Defects secondary to surgery are a result of planned defects from skull base tumor resection or iatrogenic CSF leaks most often associated with endoscopic sinus surgery. Defect size and location often dictates the option for repair. The most common locations for CSF leaks secondary to endoscopic sinus surgery were the ethmoid skull base (35.1%), cribriform (27%), and sphenoid sinus (18.9%).12 Defect location varies with the type of surgery performed, with the ethmoid roof, cribriform plate, and sphenoid commonly injured during functional endoscopic sinus surgery, while the sphenoid is more frequently injured during neurosurgical cases.5 With the advent of advanced tumor resection of the skull base, defects requiring repair have advanced in size and complexity. Patel et al introduced the concept of dividing CSF leaks into high and low flow.13 Low-pressure leaks are seen in cases of encephaloceles with small defect size or in pituitary adenoma resection where the sella diaphragm is thin with weeping of CSF. These cases are distinct from a high-pressure leak where either a ventricle or arachnoid cistern is entered.13 High-pressure leaks are seen in cases of endoscopic endonasal approaches (EEAs) to the skull base where tumor removal is performed. EEA to the skull base can be subdivided into the respective regions of repair with vascular flaps that can be utilized for each region (Table 33.1). Region I, the anterior cranial fossa, extends anteriorly from the frontal sinus to the anterior border of the planum sphenoidale or roof of the sphenoid sinus. In region II, middle cranial fossa, there is a central and lateral component that is divided by the anterior clinoid process. Defects in a central location are created with approaches to the sella or suprasellar regions. Lesions located lateral to a sagittal plane through the anterior clinoid process involve the pterygopalatine and infratemporal fossae. In region III, the posterior cranial fossa, clival lesions are the predominant pathologic entity seen. Last, region IV accounts for lesions involving the odontoid and cervical spine. Selection of the appropriate graft materials depends on the many factors encountered during the preoperative and operative stages of repair. The size and location of the defect encountered plays a role in the appropriate graft material to be used. Anatomic considerations and the state of the prepared defect site may also determine the selection of grafting material. Each defect encountered is unique with various confluences of factors influencing the necessary reconstructive material. With a plethora of materials available, algorithms and consensus statements do not presently exist to guide in the selection process. Ultimately, the selection of a specific closure material and technique is based upon the surgeon’s familiarity and experience. Autologous tissues in the form of bone, fascia, fat, cartilage, muscle, and mucosa have been used extensively because of their low cost, availability, and ease of transfer. When local tissue is scarce, nonautogenous grafts or tissue engineered matrices can be utilized successfully but with the added cost of manufacturing and processing.14–16 Below is a discussion on the various reconstructive materials available. Table 33.1 Intranasal and Regional Vascular Flap Choices for Skull Base Reconstruction
Skull Base Defect Etiology
Nontraumatic
Traumatic
Surgical Trauma
High-Flow Leak versus Low-Flow Leak
Reconstructive Materials Available
Flap | Vascular Pedicle | Reconstructive Site |
Nasoseptal flap | Posterior septal branch of sphenopalatine artery | Ideal choice for all defects |
Inferior turbinate flap | Inferior turbinate artery from posterior lateral nasal artery | Clivus and sella/parasellar |
Middle turbinate flap | Middle turbinate artery from posterior lateral nasal artery | Small anterior cranial fossa and sella defects |
Temporoparietal fascia flap | Superficial temporal artery | Clivus and parasellar |
Pericranium flap | Supraorbital and supratrochlear arteries | Ideal for all defects |
Lateral nasal wall flap | Branches of facial and anterior ethmoid arteries | Anterior cranial fossa defects up to planum sphenoidale |
Nonvascularized Autografts
Originally used in the early attempts of skull base reconstruction, nonvascularized autografts provide an excellent source for reconstruction. Bone, fascia, and fat are mainly utilized, acting as a scaffold for viable tissue to be incorporated. Because of the absence of vascularity, a slow resorptive process of the tissue occurs, allowing an influx of native cellular products to be incorporated. Experimental studies have shown free graft adherence to bone by 1 week, fibroblast invasion by 3 weeks, and a substantial amount of postoperative contracture.17
Of the free nonvascularized grafts, fat is most commonly used, primarily for its abundance, ease of harvesting, and malleability to conform to a variety of defects encountered. Typically, fat is harvested from a lower abdomen or lateral thigh incision, because of its high availability. For larger defects, fascia from either incision can also be harvested concurrently, as rectus fascia or fascia lata. Reconstructions utilizing free nonvascularized grafts tend to utilize several different layers of alternating consistency, that is, fat plug followed by fascial layer followed by subsequent layers with the eventual goal of creating a water-tight seal.
The success rate for avascular reconstructive techniques in small and idiopathic defects may be as high as 90 to 97%.18 Unfortunately, the closure rate drops to 50 to 70% in large surgically induced defects. The overall size of the defect encountered and a high CSF leak rate may prevent the utilization of avascular reconstructive techniques.
Vascularized Mucosal Flaps
The development of various vascular pedicled flaps has permitted closure of very large, high-flow defects, with a low CSF leak rate of 3 to 5%.19–23 The process of harvesting a vascularized flap is considered difficult and technically demanding than that described for nonvascularized tissue. On the contrary, the major advantages of these flaps are a preserved vascular pedicle, a capability to cover large surface areas, and relative resistance to volume loss. Many of the described flaps are based on solely one pedicle and therefore imperative that the vascular supply remains intact.
Many options for vascularized pedicled flaps are available and include the workhorse nasoseptal flap based off the posterior septal branch of the sphenopalatine artery, the inferior turbinate flap based off the inferior turbinate artery, tunneled periosteal flaps based off the superficial temporal artery, middle turbinate flap based off the posterior sphenopalatine branches and finally “rescue” or palatal flaps based off the descending palatine arteries.22–25 The nasoseptal flap, as described by Hadad et al, is commonly used given its versatility (Fig. 33.1). The flap is based on the posterior septal neurovascular pedicle, with the possibility of modifications for flap length and width given the various dimensions of defects encountered. Generally, it is advised that an overestimation of flap harvest takes place, with trimming excess tissue as needed. The mucoperichondrium is elevated in an anterior to posterior fashion with careful dissection along the pedicle. Once elevated, the flap is displaced in the nasopharynx or maxillary sinus until ready to use. This nasoseptal flap has become the workhorse of most skull base reconstructions, given its proximity to most areas needed to be addressed and its large surface area to be utilized for coverage.26 Depending on the vascular pedicle isolated during the harvest, the extent of the flap rotation can address defects extending from the lateral, ventral, and anterior skull base.20
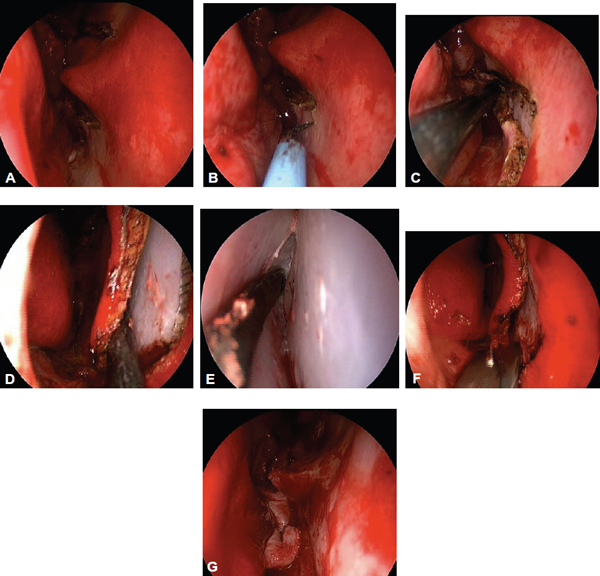
Figure 33.1 Right side of the nasoseptal flap. (A) Make posterior incisions first above and below pedicle and then extend onto the septum. Note the large septal spur of the posterior septum. The presence of a spur may make flap elevation more difficult, but it is still feasible. (B) The inferior vertical incision is then made onto the floor. This can be done with a long needle tip bovie. A similar superior vertical incision is performed next. (C) The inferior incision has been completed from the face of the sphenoid and then brought anteriorly onto the septum. (D) An anterior incision is then made and the flap is elevated in a posterior direction. (E) In the correct plane elevation of the flap will be avascular. The superior and inferior cuts are not made until the flap is elevated to the posterior incisions. (F) The inferior and superior incisions are made last using an endoscopic scissor. Cautery used along the superior incision may result in olfactory dysfunction. (G) Push the flap back into the nasopharynx. Notice that flap elevation was performed despite the presence of a large septal spur.
Patel et al, in a review of the various flaps currently described, provided a list of advantages and limitations associated with each of them.13 The nasoseptal flap was found to be a versatile flap for many of the defects encountered. The inferior turbinate flap was found to be a great option for small clival and sella/parasellar defects,23 but is limited in the overall reach within the paranasal sinuses. The middle turbinate flap was a great option for small anterior cranial defects, but it provided little tissue with thin mucosa, which was difficult to elevate. The inferior turbinate flap is more suited for more posterior reconstruction in the region of the sella and clivus. It does not have the reach nor width to reconstruct the anterior cranial fossa.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree