Purpose
To compare the efficacy of photodynamic therapy (PDT) with or without intravitreal bevacizumab injection for polypoidal choroidal vasculopathy.
Design
Retrospective, comparative, interventional case series.
Methods
We included 146 eyes of 146 patients with treatment-naïve polypoidal choroidal vasculopathy including the subfoveal region treated with PDT monotherapy or combined with intravitreal bevacizumab injection. Treatments were chosen according to the time period. For eyes that received combination therapy, bevacizumab (1.25 mg) was administrated 1 day before PDT. All eyes were followed up for at least 12 months. Ophthalmic evaluations, including measurement of the best-corrected visual acuity and optical coherence tomography, were performed at every visit. Indocyanine green angiography and fluorescein angiography were performed every 3 months.
Results
Sixty-one eyes were treated with PDT combined with bevacizumab and 85 eyes were treated with PDT monotherapy. The mean best-corrected visual acuity was significantly better in the combined treatment group than in the monotherapy group at 3 months ( P = .0016), 6 months ( P = .028), 9 months ( P = .038), and 12 months ( P = .048). However, lesions resolved in 78.7% of eyes in the combined group and in 75.3% in the monotherapy group; the recurrence rates were 43.8% and 40.6%, respectively, and did not differ significantly. The rate of development of subretinal hemorrhage within 1 month from the initial treatment was significantly lower in the combined group than in the PDT monotherapy group (4.5% vs 17.7%; P = .023).
Conclusions
Photodynamic therapy combined with bevacizumab injection offers significantly better early visual outcomes than PDT alone. Combined treatment did not affect the resolution and recurrence of lesions; however, it decreased the rate of development of PDT-related hemorrhages.
Polypoidal choroidal vasculopathy (PCV) is characterized by a complex of branching vascular networks terminating in aneurysmal or polypoidal lesions. The prevalence of PCV is higher in Asian than in white individuals, and recent studies have shown that PCV accounts for almost half of eyes presumed to have exudative age-related macular degeneration (AMD) in Japan.
Photodynamic therapy (PDT) with verteporfin (Visudyne; Novartis Pharma AG, Basel, Switzerland), the first drug available for patients with subfoveal choroidal neovascularization (CNV) associated with AMD, is more effective for treating PCV than CNV and can occlude the polypoidal vascular dilatations, resulting in stable or improved vision. However, recurrent or newly developed polypoidal lesions may affect vision during a longer follow-up. Beside the characteristic polypoidal dilatations, lacy CNV-like vessels can develop with exudation. Unexpected subretinal hemorrhages after PDT are another serious problem in eyes with PCV.
The efficacy of the anti–vascular endothelial growth factor (VEGF) drug bevacizumab (Avastin; Genentech, South San Francisco, California, USA) is well known for treating CNV secondary to AMD ; however, the efficacy for PCV seems limited. We found that intravitreal injections of bevacizumab reduced exudative fluid but did not affect the original abnormal vasculatures and caused subsequent recurrence of fluid in most eyes.
Combined PDT and intravitreal bevacizumab therapy was introduced recently as a treatment strategy for AMD. It resulted in favorable outcomes, including improved visual acuity (VA), low rates of retreatment, and reduced fluorescein leakage, lesion size, and retinal thickness without new safety concerns.
PDT monotherapy and anti-VEGF drugs have separate levels of efficacy and limitations. For PCV, PDT occluded polypoidal vascular lesions and anti-VEGF drugs resolved the associated fluid. If combining these therapies could result in additional or complementary effects, there may be further improvements in visual and anatomic outcomes in eyes with PCV compared with PDT monotherapy. The aim of the current study was to determine if the combined treatment of intravitreal bevacizumab and PDT for PCV is associated with additional efficacy during the 1-year follow-up.
Methods
A total of 146 Japanese patients with symptomatic, treatment-naïve, subfoveal PCV were treated with PDT with or without an intravitreal injection of bevacizumab and followed up for more than 1 year. The initial treatments were chosen according to the time period. From March 2005 through September 2006, PDT monotherapy was administered and from October 2006 through August 2008, PDT combined with intravitreal bevacizumab injection was administered to consecutive patients who agreed to the use of bevacizumab. The data from patients who did not agree to bevacizumab treatment during the latter period were included as having been treated by PDT monotherapy.
The diagnosis of PCV was established based on the finding of polyplike choroidal vessel dilatation with or without a branching vascular network on indocyanine green angiography (ICGA). The ICGA images were obtained using a camera (TRC-50EX; Topcon, Tokyo, Japan) in all patients. A scanning laser ophthalmoscope (Heidelberg Retina Angiograph 2; Heidelberg Engineering, Heidelberg, Germany) also was used beginning in June 2005. Eyes with either polypoidal lesions or regions of branching vascular networks in the subfovea were included. Eyes with coexisting CNV were excluded.
Treatment and Follow-Up
Three authors (F.G., M.S., and M.T.) treated and followed up all patients. PDT with verteporfin was administrated in a full-fluence dose according to the Treatment of Age-Related Macular Degeneration with Photodynamic Therapy protocol with 1 modification: the greatest linear dimension (GLD) of the lesion for laser exposure during PDT was determined based on ICGA findings in all patients as previously reported. In eyes treated with combined therapy, 1.25 mg bevacizumab was injected intravitreously 1 day before PDT. Before the bevacizumab injections, the eyes and lids were disinfected with povidone iodine after topical anesthesia was administered. Bevacizumab was injected 3.5 to 4.0 mm posterior to the limbus using a 29-gauge needle. A topical antibiotic was applied 4 times daily for 1 week.
All patients underwent a comprehensive ocular examination, including measurement of the best-corrected visual acuity (BCVA) using Landolt C charts, fundus examinations, color fundus photography, and optical coherence tomography (OCT) using Stratus or Cirrus devices (Carl Zeiss Meditec, Dublin, California, USA) at least 1, 3, 6, 9, and 12 months after the initial treatments. If patients were not examined at those follow-up dates, the point closest to the defined date was selected. Additional intermediate visits were scheduled for patients with combined therapy at 4- to 6-week intervals. Fluorescein angiography and ICGA were performed at baseline and every 3 months to assess the resolution and recurrence of abnormal polypoidal lesions. Additional treatments were performed when abnormal vascular lesions associated with exudative fluid were seen on ICGA with the same therapy received at baseline. In the combined treatment group, intravitreal bevacizumab without PDT was administered when exudative fluid was seen on OCT during the intermediate visits.
The resolution of PCV lesions after the initial treatment was defined as the disappearance of symptomatic polypoidal vasculatures on ICGA at 3 months with complete resolution of exudative fluid on OCT. A recurrence was defined by the reappearance of abnormal vasculature on ICGA with exudative fluid on OCT.
The development of serious adverse events related to the initial treatment was recorded. Because a subretinal hemorrhage is the major adverse event associated with PDT for PCV, the incidence of new subretinal or subpigment epithelial hemorrhage of more than 1 optic disc diameter developed within 1 month after the initial treatment was assessed.
Statistical Analysis
The BCVA was converted to the logarithm of the minimal angle of resolution (logMAR) equivalents. Missing data at intermediate time points were input using the method of last observation carried forward. Each 0.10-unit difference in logMAR VA was calculated as 1 line.
The changes in BCVA at 1, 3, 6, 9, and 12 months from baseline with each treatment were evaluated by analysis of variance repeated measures. The BCVA values at 1, 3, 6, 9, and 12 months were compared between treatments by analysis of covariance (ANCOVA) to rule out any bias correlated with the visual outcomes. The initial ANCOVA model included the treatment as a factor and the baseline age, gender, BCVA, GLD, presence or absence of pigment epithelial detachment (PED), and the presence or absence of subretinal or subpigment epithelial hemorrhages as covariates. A PED was defined as the presence of serous or hemorrhagic PEDs, or both, 1 disc area or larger on ICGA and OCT independent of the polypoidal lesions. Appropriate covariates were selected for the final ANCOVA model using the Akaike information criterion. Stepwise regression analysis was performed to elucidate factors that affected the BCVA at 12 months among baseline age, gender, BCVA, GLD, PED, hemorrhage, and the treatment. To determine which factors were associated with a BCVA of 20/40 or better at 12 months, logistic regression analysis was performed using the same variables as the stepwise regression analysis. We also compared the rate of resolution and recurrence between treatments (Pearson chi-square test). The incidence of hemorrhage developing after PDT and other adverse events also were compared. Statistical analyses were performed with SAS software version 9.1 (SAS Institute, Cary, NC). P values less than .05 were considered significant, and all tests were 2-sided.
Results
A total of 146 eyes of 146 patients (113 men, 33 women) were included; 61 eyes of 61 patients (44 men, 16 women) were treated initially with combined therapy and 85 eyes of 85 patients (68 men, 17 women) were treated with PDT monotherapy. The patient characteristics in both groups are shown in the Table . The baseline factors, including BCVA, gender, age, GLD, and the rates of coexisting PED, hemorrhage, or both, did not differ significantly between treatments.
| Combined Therapy (n = 61) | PDT Monotherapy (n = 85) | |
|---|---|---|
| Sex, no. (%) | ||
| Men | 44 (72.1) | 68 (80.0) |
| Women | 16 (26.2) | 17 (20.0) |
| Age (yrs) | ||
| Mean ± SD | 70.9 ± 7.1 | 70.9 ± 6.8 |
| Range | 54 to 83 | 53 to 85 |
| Lesion GLD (μm) | ||
| Mean ± SD | 2626 ± 1138 | 2521 ± 996 |
| Range | 500 to 5800 | 800 to 5300 |
| LogMAR visual acuity (Snellen) | ||
| Mean | 0.48 (20/60) | 0.45 (20/56) |
| Median | 0.40 (20/50) | 0.40 (20/50) |
| Range | 1.15 (20/286) to 0 (20/20) | 1.05 (20/222) to 0 (20/20) |
| SRH, no. (%) | 21 (34.4) | 22 (25.9) |
| PED, no. (%) | 30 (49.2) | 36 (42.4) |
Visual Outcomes
The mean BCVA scores over time are shown in Figure 1 . The BCVA in the combined therapy group improved significantly from baseline at 1 month ( P = .016), 3 months ( P < .0001), 6 months ( P < .0001), 9 months ( P < .0001), and 12 months ( P = .0027) after the initial treatment; in the PDT monotherapy group, the BCVA improved significantly at 9 months ( P = .011) and tended to improve at 12 months ( P = .056).
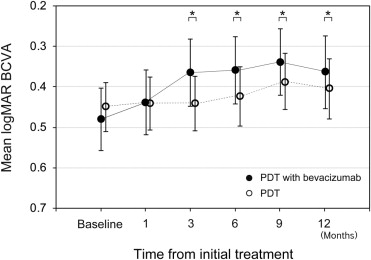
To compare the visual outcomes at various time points between treatments, we performed ANCOVA analyses. Because the initial ANCOVA analyses suggested that some baseline factors such as the BCVA, GLD, and the presence of PED were correlated with the posttreatment VA at each time point, those factors were adjusted and the mean logMAR VAs were compared between treatments. Ultimately, the mean BCVA in the combined therapy group was significantly better than that in the monotherapy group at 3 months ( P = .0016), 6 months ( P = .028), 9 months ( P = .038), and 12 months ( P = .048) from the initial treatment. The data showed that combined therapy had a maximum effect on VA improvement compared with PDT monotherapy at 3 months, and this effect gradually decreased with time but was still significant at 12 months.
Eyes gained a mean of 0.12 logMAR unit (1.2 lines) in the combined therapy group and 0.04 logMAR unit (0.4 lines) in the PDT monotherapy group over 12 months. All eyes (100%) in the combined therapy group and 80 eyes (94.1%) in the PDT monotherapy group had improved or stable VA (defined as a loss of 3 or fewer lines of vision at 3 months); the rates were 90.2% (55/61) and 88.2% (75/85) at 12 months, respectively, in the treatment groups. An improvement in the BCVA of 3 lines or more was seen in 14.8% (8/44) in the combined therapy group and in 3.5% (4/79) in the PDT monotherapy group at 3 months, which was significant (Fisher exact test, P = .044); however, the respective rates were 23.0% and 18.8% at 12 months, which were not significant. The percentages of eyes with a BCVA of 20/40 or better at 12 months was 62.3% in the combined therapy group and 54.1% in the monotherapy group ( Figure 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


