Purpose
To investigate the effects of different head positions in the lateral decubitus posture on intraocular pressure (IOP) in medically treated patients with open-angle glaucoma (OAG).
Design
Prospective observational study.
Methods
setting : Institutional. participants : Twenty patients with bilateral OAG who received only latanoprost as treatment. observation procedures : IOP was measured using an ICare Pro tonometer in the sitting, supine, right, and left lateral decubitus posture. In lateral decubitus posture, IOP measurements were taken with 3 different head positions (30 degrees higher than, 30 degrees lower than, and parallel to the center of the thoracic vertebra) in a randomized sequence. main outcome measures : Comparison of the IOPs between the dependent (lower-sided) and nondependent eyes in the lateral decubitus postures with different head positions. We also analyzed the differences in IOPs between the better and worse eyes.
Results
IOP was higher in the dependent eyes than in the nondependent eyes in lateral decubitus posture, regardless of the head position (all P < .05). Lower head position increased the IOP of dependent eyes, compared with the neutral or higher head position. However, the amounts of IOP elevation seen during the changes of body posture or head position were not significantly different between the better and worse eyes.
Conclusions
Low head position elevates IOP of the dependent eyes of medically treated OAG patients compared with neutral head position in the lateral decubitus posture. Adjustment of the height of a pillow may help mitigate IOP elevations resulting from lying on the side with a low or no pillow in glaucoma patients.
Elevated intraocular pressure (IOP) is one of the major risk factors for the development and progression of glaucoma. Accurate assessment of IOP is important because elevated IOP is the only risk factor that can be modified by therapeutic interventions. IOP has been shown to vary with alteration of the body posture. Thus, IOP readings obtained using the Goldmann applanation tonometer with patients in the sitting posture at the office may not reflect what happens in the eyes outside office hours.
IOP is well established to be higher in the recumbent postures compared with that measured in the upright posture. In previous studies on the nocturnal variations of IOP, the supine posture has been considered as the only habitual posture and nighttime IOPs have been measured in the supine posture. However, sleep studies have shown that one may take nonsupine postures such as lateral decubitus or prone, and that the lateral decubitus posture is preferred to the supine posture by older patients. Recent studies have shown that lateral decubitus or prone positioning with head rotation increases IOP in the dependent (lower-sided) eye, compared with the supine posture. Recumbent posture–induced IOP elevation has been shown not only in healthy subjects but also in untreated open-angle glaucoma (OAG) patients. Moreover, such posture-induced IOP elevation has been associated with greater glaucomatous visual field damage in OAG patients. Therefore, it would be helpful to know the changes of IOP in various recumbent postures for better management of glaucoma patients.
People usually use a pillow of uniform height that has been designed high enough to support the neck in the flat-lying position. Recently, we conducted a prospective study in healthy individuals to investigate how different head positions, resulting from alterations of pillow height, in the lateral decubitus posture influence IOP, and this study found that the head position influences the IOP elevation of the dependent eye in the lateral decubitus posture.
The present study aimed to investigate how changing the head position in the lateral decubitus posture influences IOP in the medically treated OAG patients, and to assess the relationship between the IOP alteration in such a change of head position in the lateral decubitus posture and the level of visual field damage.
Methods
This prospective, observational study was conducted at the Department of Ophthalmology, Korea University College of Medicine. This study included 20 patients who had been diagnosed with bilateral OAG and treated only with latanoprost 0.001% ophthalmic solution in both eyes at the Korea University Ansan Hospital. Study approval was obtained from the Institutional Review Board of the Korea University Ansan Hospital. The study was conducted in adherence with the tenets of the World Medical Association’s Declaration of Helsinki. Written informed consent was obtained from each subject prior to participating in the study.
Each patient underwent comprehensive ophthalmic examinations of both eyes, including best-corrected visual acuity, refractive error, slit-lamp biomicroscopy, axial length (AL) with IOL Master (Carl Zeiss Meditec, Jena, Germany), central cornea thickness (CCT) with a noncontact specular microscope (sp-3000p; Topcon, Tokyo, Japan), gonioscopy, Goldmann applanation tonometry, Humphrey Swedish interactive threshold algorithm (SITA) 30-2 testing (Zeiss-Humphrey, San Leandro, California, USA), and dilated stereoscopic funduscopy.
To meet the criteria for a diagnosis of OAG, patients had to have a glaucomatous optic disc change, a reproducible glaucomatous visual field defect on the SITA 30-2 perimetry, and normal-appearing open angles on gonioscopy. Glaucomatous optic disc changes were defined as focal or diffuse neuroretinal rim thinning, localized notching, or retinal nerve fiber layer defects with corresponding visual field defects. Glaucomatous visual field defects were defined by 2 of the following 3 criteria: the presence of a cluster of 3 points on a pattern deviation probability plot with P < .05, one of which had P < .01; a pattern standard deviation with P < .05; or glaucoma hemifield test results outside normal limits.
Patients with concomitant ocular disease, best-corrected visual acuity worse than 20/40, refractive error of more than 9 diopters spherical equivalent (SE) or 2 diopters of astigmatism, use of contact lenses, a history of previous intraocular surgery, or a history of spine disease and its related symptoms were excluded from this study. Patients with advanced glaucoma (mean deviation ≤−12 dB) were also excluded.
To minimize the effect of diurnal variation, IOP measurements were performed by a single observer between 6:00 PM and 8:00 PM. IOP was measured using a single ICare rebound tonometer (ICare Pro; Tiolat Oy, Helsinki, Finland) in both eyes for each position. The right eye was always examined first. The subject was asked to look straight ahead and the IOP was measured by touching the transducer to the center of the subject’s cornea. ICare Pro has a built-in inclination sensor to measure the supine posture IOP; an arrow appears in the display indicating the vertical position of the tonometer. Three consecutive sets of measurements, with 6 measurements for each set, were made. The average of each set was made automatically, and the averaged values were used for the statistical analyses. To allocate a randomized sequence of IOP measurements in the lateral decubitus posture, each participant was asked to pick up 1 card, where the different positions of head and body were written on the back, one after another until all the 6 cards were open. Thus, each participant was informed of the sequence of changing body and head positions.
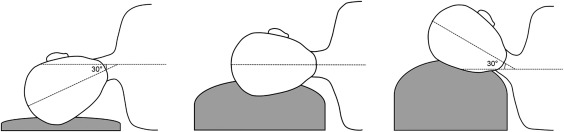
First, each participant was asked to sit on a backrest chair in a quiet room under dim light conditions. Five minutes later, IOP was measured in the sitting posture; and IOP was measured in the supine posture in another 5 minutes. Then, the subject was asked to maintain the right or left lateral decubitus posture on a bed with a soft pillow of different heights underneath the head, in the randomized sequence predetermined in the aforementioned manner. IOP was measured 5 minutes after assuming each posture. In the right and left lateral decubitus postures, IOP measurements were taken with 3 different head positions ( Figure 1 ): lateral decubitus with the head 30 degrees higher than the center of the thoracic vertebra; lateral decubitus with the head parallel to the center of the thoracic vertebra; lateral decubitus with the head 30 degrees lower than the center of the thoracic vertebra. Multiple pillows (2 or 3) were used for the 30 degrees head-up position (right and left lateral decubitus posture with high head position), whereas a smaller pillow (of lower height) or no pillow was used for the 30 degrees down position (right and left lateral decubitus with low head position). The degree of a lateral-ward bend of the neck was determined by assessment of the angle between the midlines of the face and the body. The subject was asked to maintain a straight gaze during assumption of the lateral decubitus posture so that his or her dependent eye was not compressed against the pillow.
For all patients, the better eye and the worse eye were defined based on the mean deviation value determined by the Humphrey visual field testing. The height and weight were recorded by patients’ self-report.
Statistics
Sample size was calculated using the G*Power software (version 3.0.10; Universität Kiel, Dusseldorf, Germany) with α = 0.05 and ß = 0.2. A preliminary investigation of 5 patients revealed that the standard deviation of the IOP difference of the dependent eyes was 2.25 mm Hg between the neutral and the low head position in lateral decubitus postures. A sample size calculation determined that at least 20 patients would be required to detect an IOP difference of more than 2.0 mm Hg in the dependent eyes with a power of 80%. All statistical analyses were performed using SPSS version 20.0 (SPSS, Inc, Chicago, Illinois, USA). The Wilcoxon signed rank test was used to compare refractive errors, AL, CCT, and IOP measured by Goldmann tonometer between fellow eyes, and also to assess the inter-eye IOP differences in each body and head position. The Wilcoxon signed rank test with Bonferroni correction was used to compare IOP by changing pillow heights in the lateral decubitus postures. The linear regression analysis was used to assess the associations among the IOP elevations induced by the recumbent postures and the baseline characteristics such as refractive error, AL, CCT, height, and weight. Both univariate and multivariate analyses were performed separately for each recumbent posture. Variables with a P value less than or equal to .3 in the univariate analyses were included as candidate variables for the multivariate analysis. A P value of < .05 was considered significant unless the Bonferroni correction method for multiple comparisons was used, in which case a P value < .003 was considered significant.
Results
Among 20 patients, 9 patients were male and the overall mean age was 52.6 ± 8.0 years. The mean height was 165.1 ± 7.6 cm and the mean weight was 61.1 ± 8.6 kg. There was no significant difference between right and left eyes in refractive error, mean AL, CCT, mean IOPs measured by Goldmann applanation tonometry, or mean deviation (all P > .05) ( Table 1 ). No significant inter-eye difference was found in IOPs measured by ICare Pro tonometry in the sitting and supine posture. Among the 20 patients, 8 patients had the worse visual field in the right eye and 12 patients had the worse visual field in the left eye. There was no significant difference between better and worse eyes in refractive error, mean AL, CCT, or mean IOPs measured by Goldmann applanation tonometer, but there was a significant difference for the mean deviation ( P < .001). No significant difference in IOPs was found between the better and worse eyes in the sitting and supine posture (all P > .05) ( Table 1 ).
| Variable | Right Eye (Mean ± SD) | Left Eye (Mean ± SD) | P Value a | Better Eye (Mean ± SD) | Worse Eye (Mean ± SD) | P Value b |
|---|---|---|---|---|---|---|
| SE, diopter | −2.19 ± 2.60 | −2.01 ± 2.48 | .226 | −2.14 ± 2.46 | −2.06 ± 2.62 | .569 |
| AL, mm | 24.4 ± 1.0 | 24.3 ± 1.0 | .204 | 24.3 ± 1.0 | 24.4 ± 1.0 | .940 |
| CCT, μm | 514.5 ± 34.0 | 516.4 ± 33.3 | .201 | 514.5 ± 3.2 | 516.4 ± 34.1 | .218 |
| IOP, mm Hg | ||||||
| IOPg | 13.7 ± 2.2 | 13.6 ± 2.0 | .317 | 13.6 ± 2.1 | 13.6 ± 2.1 | 1.00 |
| IOP SIT | 13.8 ± 2.5 | 13.6 ± 2.0 | .562 | 13.6 ± 2.3 | 13.7 ± 2.2 | .400 |
| IOP SUP | 15.7 ± 2.0 | 15.7 ± 1.8 | .711 | 15.6 ± 2.0 | 15.7 ± 1.9 | .365 |
| MD, dB | −3.49 ± 2.30 | −4.70 ± 3.03 | .108 | −2.98 ± 2.14 | −5.21 ± 2.84 | <.001 |
a Wilcoxon signed rank test between right and left eye.
Table 2 lists the IOP measurements obtained in the lateral decubitus postures with different head positions. The IOP of the dependent eye was significantly higher than that of the nondependent eye in the lateral decubitus postures with different head positions (all P ≤ .05).
| Body Posture | Head Position | IOP (Mean ± Standard Deviation), mm Hg | P Value a | ||
|---|---|---|---|---|---|
| Dependent Eye | Nondependent Eye | Mean Difference a | |||
| Right lateral decubitus | High | 16.6 ± 3.3 | 15.8 ± 2.9 | 0.79 ± 1.21 | .014 |
| Neutral | 17.5 ± 3.5 | 16.3 ± 3.1 | 1.25 ± 0.83 | <.001 | |
| Low | 19.5 ± 2.6 | 16.6 ± 3.3 | 2.94 ± 1.84 | <.001 | |
| Left lateral decubitus | High | 16.6 ± 3.8 | 15.7 ± 2.7 | 0.90 ± 1.49 | .013 |
| Neutral | 17.3 ± 3.5 | 15.9 ± 2.5 | 1.39 ± 1.15 | <.001 | |
| Low | 19.6 ± 3.2 | 17.5 ± 2.5 | 2.10 ± 1.47 | <.001 | |
| Better eye–dependent decubitus | High | 16.7 ± 3.6 | 15.6 ± 2.9 | 1.13 ± 1.42 | .008 |
| Neutral | 17.3 ± 3.5 | 16.2 ± 3.0 | 1.10 ± 1.00 | <.001 | |
| Low | 19.8 ± 2.9 | 17.7 ± 2.9 | 2.74 ± 1.87 | <.001 | |
| Worse eye–dependent decubitus | High | 16.4 ± 3.5 | 15.9 ± 2.6 | 0.54 ± 1.22 | .050 |
| Neutral | 17.5 ± 3.5 | 15.9 ± 2.7 | 1.52 ± 0.97 | <.001 | |
| Low | 19.3 ± 3.0 | 17.0 ± 3.1 | 2.26 ± 1.52 | <.001 | |
Figure 2 shows the differences of IOP alterations between supine and lateral decubitus postures with different head positions. Compared with that of the ipsilateral eye in the supine posture, the IOP of the dependent eye was higher in lateral decubitus posture with head at 30 degrees lower position (all P < .003). The IOP of the dependent eye in right, left, or worse eye–dependent lateral decubitus posture with neutral head position was higher than that of the ipsilateral eye in the supine posture ( P = .003, P = .002, and P = .001, respectively), whereas such difference was not noted in the better eye–dependent lateral decubitus posture ( P = .011). Figure 3 shows comparisons of IOPs of the dependent eye in the lateral decubitus postures with different head positions. Among those measured in the lateral decubitus posture, the IOP of the dependent eye with 30 degrees lower head position was higher than that measured in the neutral or 30 degrees higher head position (all P < .001). Detailed P values and IOP differences are listed in Supplemental Table 1 (available at AJO.com ).
Figure 4 is the scatterplot of the individual changes in IOP in the supine and the lateral decubitus postures with different head positions compared with the sitting IOP. The magnitude of IOP elevations induced by recumbent postures varied among the OAG patients. When compared between the IOP of the dependent eye measured in the lateral decubitus postures with the head lowered and that measured in the supine position, 28 of 40 eyes (70%) showed IOP elevations of ≥3 mm Hg; 20 eyes (50%), ≥4 mm Hg; 11 eyes (28%), ≥5 mm Hg; and 4 eyes (10%), ≥6 mm Hg. Table 3 summarizes the magnitudes of changes in IOP induced by alterations of body or head position. No significant difference in the amount of posture-induced IOP changes was found between the better and worse eyes (all P > .05).
| Between Positions | Better Eye | Between Positions | Worse Eye | P Value a | ||
|---|---|---|---|---|---|---|
| IOP Difference (mm Hg) | Range (mm Hg) | IOP Difference (mm Hg) | Range (mm Hg) | |||
| Supine vs sitting | 2.0 ± 0.9 | 0.2–4.2 | Supine vs sitting | 2.0 ± 0.9 | 0.5–4.0 | .492 |
| BED LD-H vs sitting | 3.1 ± 2.1 | −0.2 to 5.5 | WED LD-H vs sitting | 2.7 ± 1.9 | −0.1 to 7.3 | .235 |
| BED LD-N vs sitting | 3.7 ± 1.5 | 1.6–6.7 | WED LD-N vs sitting | 3.7 ± 1.7 | 1.1–6.7 | .331 |
| BED LD-L vs sitting | 6.2 ± 1.6 | 3.4–8.8 | WED LD-L vs sitting | 5.6 ± 1.6 | 2.6–8.5 | 1.00 |
| BED LD-H vs supine | 1.0 ± 2.1 | −1.6 to 6.2 | WED LD-H vs supine | 0.7 ± 2.1 | −2.0 to 6.2 | .287 |
| BED LD-N vs supine | 1.7 ± 2.0 | −0.6 to 5.4 | WED LD-N vs supine | 1.7 ± 1.9 | −0.1 to 5.4 | .239 |
| BED LD-L vs supine | 4.2 ± 1.7 | 1.7–7.4 | WED LD-L vs supine | 3.6 ± 1.6 | 0.7–7.4 | .117 |
Univariate and multivariate linear regression analysis ( Supplemental Tables 2 and 3 , available at AJO.com ) between the recumbent posture–induced IOP elevations and the demographic data found that AL was positively associated with the IOP elevations induced by neutral (dependent eye, B = 0.969; nondependent eye, B = 0.894; both P < .05) and high (dependent eye, B = 1.387; nondependent eye, B = 0.523; both P < .05) head position in lateral decubitus posture. The age correlated negatively with IOP elevations induced by lateral decubitus posture with low head position (dependent eye, B = −0.086, P = .037). The other factors including CCT, SE, height, and weight showed no association with the recumbent posture–induced IOP elevations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


