Purpose
To determine whether Descemet stripping automated endothelial keratoplasty (DSAEK) donor cornea graft thickness impacts measurements of best spectacle-corrected visual acuity (BSCVA), refractive error and intraocular pressure (IOP).
Design
Retrospective chart review in a tertiary care center at Duke University Eye Center.
Methods
We studied 460 eyes that had undergone DSAEK surgery. They were segregated into three groups based on the thickness of the donor graft: <100 μm (n = 67 eyes); 100–150 μm (n = 316 eyes); and >150 μm (n = 77 eyes). The three graft-thickness groups were assessed at about 6 months postoperatively for measurement of BSCVA, spherical equivalent, and IOP.
Results
Baseline demographics were similar in the three groups. All groups experienced significant improvement in BSCVA (mean ± SD = −0.34 ± 0.50 logMAR); mild hyperopic shift (mean ± SD = 0.48 ± 1.7 D); and stability in IOP measurements (mean ± SD = 0.19 ± 4.8 mm Hg). There were no significant differences in groups according to donor graft thicknesses with respect to change in BSCVA ( P = 0.8); hyperopic shift ( P = 0.76); or IOP measurement ( P = 0.56).
Conclusions
DSAEK significantly improves BSCVA. DSAEK graft thickness may not play an important role in the final BSCVA, refractive error, or accuracy of IOP measurement. The ideal DSAEK graft thickness to minimize graft-related complications remains to be determined.
Treatment of corneal endothelial dysfunction by partial thickness corneal transplantation has evolved considerably since the revival of posterior lamellar keratoplasty by Melles and associates in 1998. Terry and Ousley performed the first U.S. cases of deep lamellar endothelial keratoplasty in 2000. Endothelial keratoplasty continues to increase in popularity. In 2005, endothelial keratoplasty represented 4% of all cornea transplants in the United States compared to 44% in 2008. In the ensuing years, numerous methods of graft preparation, insertion and manipulation have been described and improved upon. Descemet stripping automated endothelial keratoplasty (DSAEK) has become the procedure of choice for the replacement of diseased corneal endothelium in patients with Fuchs endothelial dystrophy or pseudophakic bullous keratopathy. In DSAEK, the diseased endothelium is removed and replaced by a donor graft that consists of variable amounts of posterior lamellae, Descemet membrane and healthy endothelial cells. DSAEK is often performed through a small sclerolimbal incision. Thus it offers many advantages over penetrating keratoplasty. Specifically, DSAEK provides better tectonic stability, minimal induced astigmatism, early refractive stability, faster vision recovery, and reduced suture-related complications. DSAEK has showed great promise in improving the visual acuity of patients with corneal endothelial disease. Initially, DSAEK was thought to induce negligible change in refractive error. However, there has been increasing evidence that DSAEK may lead to a hyperopic shift. Further, there have been questions related to whether adding tissue to the recipient cornea affects measurement of intraocular pressure (IOP). It is well known that a thicker central corneal thickness (CCT) leads to falsely high measurements of IOP by the Goldmann tonometer in normal corneas.
As endothelial keratoplasty enters its second decade, interest remains high in refining the numerous methods that compose the procedure, including the preservation of prepared tissue, the tools and techniques of graft preparation and insertion, and the optimal characteristics of the donor lenticule. Regarding the last element, there is anecdotal evidence favoring thinner grafts to lessen the DSAEK-induced hyperopic shift. There is also ongoing discussion among endothelial keratoplasty surgeons about the ideal DSAEK graft thickness that would lead to the best visual acuity, the lowest complication rates, and the least effect on IOP.
This study aimed to address these questions by examining differences among three different graft thickness groups as they relate to visual acuity, refractive error, and IOP measurement.
Methods
Inclusion and Exclusion Criteria
This retrospective chart review was approved by the institutional review board of Duke University Medical Center. Patients who underwent DSAEK surgery between 2004 and 2008 at the Duke University Eye Center were studied. Surgeries were performed by one of three surgeons, typically under monitored anesthesia care with topical therapy.
Inclusion criteria were endothelial dysfunction, attending physician as primary surgeon, and minimum duration of follow-up of 6 months or more. Exclusion criteria were any significant ocular comorbidity (eg, glaucoma, macular degeneration); concurrent ocular surgery; or prior ocular surgery (except for cataract extraction and intraocular lens implantation).
Baseline Demographics
Baseline assessment of each patient included age, gender, diagnosis, uncorrected visual acuity, and best spectacle-corrected visual acuity (BSCVA), manifest spherical equivalent (SE), IOP, CCT, corneal topography, and slit-lamp biomicroscopic examination. Patients were similarly assessed on postoperative day 1, then at the first week, the first month, and 3 months, 6 months, and 12 months following the surgery. Visual acuity for all patients during all visits was measured by Snellen charts projected by the Nikon NPS-3 Chart Projector (Nikon Instruments, Melville, New York, USA). Refractive error was assessed via manifest refraction. In patients with very poor BSCVA, manifest refraction could not be obtained. Preoperative as well as postoperative IOP was measured by Tono-Pen XL Applanation Tonometer (Reichert Technologies, Depew, New York, USA). Central corneal thickness was measured by Pachmate handheld pachymeter (DGH Technology, Exton, Pennsylvania, USA). Preoperative graft thickness for all tissues was provided by the corneal donor tissue supplier (Ocular Systems, Winston-Salem, North Carolina, USA). Measurements were performed by ultrasound pachymeter on the posterior graft directly following preparation via microkeratome. All surgeons used a standardized air management method featuring 10 minutes of 100% anterior chamber air-fill intraoperatively. Patients then remained supine for 1 hour. The air-fill was then reduced to about 50% at the slit-lamp. Patients were then sent home with instructions to lie flat for much of the next 24 hours.
Outcome Measures and Statistical Analysis
Analysis of patient outcomes included comparisons of mean preoperative and postoperative logMAR BSCVA, IOP and SE for the study population as well as for each cohort. A paired t test was used for statistical comparison of the preoperative and postoperative means in the study population. Difference in preoperative and postoperative logMAR BSCVA, IOP, and SE were calculated for each group. Comparisons of the mean change in each variable in the three groups were performed using the Kruskal-Wallis test. Statistical analyses were performed using the statistical software, SPSS 9.1 (IBM SPSS, Somers, New York, USA) and SAS v 9.1 (SAS Institute, Cary, North Carolina, USA).
Results
Baseline Demographics
Between 2004 and 2008, 880 eyes underwent DSAEK surgery at the Duke University Eye Center. Of those, 420 were excluded based on our inclusion and exclusion criteria. The two greatest reasons for exclusion were follow-up time of less than 6 months and concurrent ocular pathology. Our inclusion and exclusion criteria were met by 460 patients.
The preoperative graft thickness was provided by the corneal donor tissue supplier (Ocular Systems). Three groups were identified based on thickness of the transplanted donor graft: 67 eyes received grafts thinner than 100 μm (group 1); 316 eyes received grafts between 100 and 150 μm in thickness (group 2); and 77 eyes received grafts thicker than 150 μm (group 3). The mean (± SD) follow-up period was 7.5 ± 0.2 (group 1); 7.4 ± 0.2 (group 2); and 8.1 ± 0.4 months (group 3).There was no statistically significant difference among the three groups with respect to age, gender, mean logMAR BSCVA, IOP, CCT, SE, or diagnosis. Also, there was no difference in the donor grafts’ endothelial cell counts ( Table 1 ).
| Graft Thickness range (Mean ± SD) (μm) a | Number of eyes | Gender b | Mean Age (years) | Mean BSCVA (LogMAR) c | IOP | SE d | CCT e | Etiology f | ECC g |
|---|---|---|---|---|---|---|---|---|---|
| 47–99 (92 ± 12) | 67 | 45 F (67%) | 66 | 0.99 | 15.2 | −0.12 | 648 | 67% Fuchs | 2985 |
| 100–150 (126 ± 14) | 316 | 198 F (63%) | 70 | 0.88 | 14.9 | −0.10 | 672 | 70% Fuchs | 2998 |
| 151–196 (159 ± 11) | 77 | 40 F (52%) | 68 | 0.86 | 15.2 | 0.18 | 674 | 73% Fuchs | 3095 |
a μm, graft thickness in microns.
b Number of patients who were female (%).
c BSCVA = best spectacle-corrected visual acuity; LogMAR = logarithm of the minimum angle of resolution.
d SE = spherical equivalent. SE could not be obtained in patients with poor vision.
e CCT = central corneal thickness as measured by pachymetry.
f Etiology = underlying disorder (% who have Fuchs corneal endothelial dystrophy).
g ECC = median endothelial cell count of the donor graft (cells/mm 2 ).
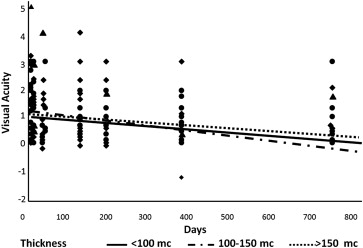
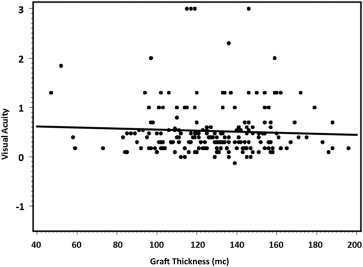
Visual Acuity
Our patients experienced significant improvement in visual acuity (mean = −0.34 ± 0.50 logMAR BSCVA) around the 6-month follow-up time point ( P < 0.01). At that time, group 1 had a mean improvement in logMAR BSCVA of −0.35 ± 0.59. This was comparable to the results achieved in group 2 (mean = −0.32 ± 0.50) and group 3 (mean = −0.34 ± 0.49). The BSCVA continued to improve in all three groups throughout the duration of our study. There was no statistically significant difference among the three groups with respect to improvement in visual acuity at about 6 months ( P = 0.8) ( Figure 1 ) nor during the duration of our study ( P = 0.77). In addition, there was no correlation between BSCVA and donor graft thickness at about 6 months of follow-up ( P = 0.48) ( Figure 2 ). Further, there was no difference among the three groups in the percentage of patients achieving BSCVA ≥20/20, ≥20/25, or ≥20/40 ( P = 0.71) ( Table 2 ).
| DSAEK graft thickness (mc) a | ≥20/20 n (%) b | ≥20/25 n (%) b | ≥20/40 n (%) c | P value b |
|---|---|---|---|---|
| 47–99 (92 ± 12) | 0 (0) | 1 (2) | 15 (30) | 0.71 |
| 100–150 (126 ± 14) | 3 (1) | 16 (6) | 81 (29) | |
| 151–196 (159 ± 11) | 0 (0) | 5 (7) | 18 (26) |
a DSAEK = Descemet stripping automated endothelial keratoplasty.
b n = number of patients achieving BSCVA.
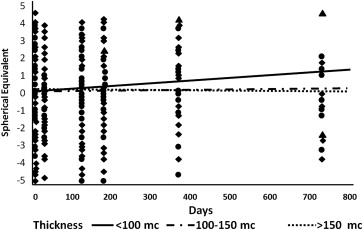
Refractive Error
DSAEK surgery resulted in a mean hyperopic shift in this patient population. At about the sixth month of follow-up, all groups showed mean hyperopic shifts compared to baseline. The mean hyperopic change was 0.48 ± 1.7D. The mean hyperopic shift for group 1 was 0.54 ± 1.8D. This is comparable to the results achieved by group 2 (mean = 0.42 ± 2.0D) and group 3 (mean = 0.34 ± 1.8D). There was no statistically significant difference among the three groups in the amount of mean hyperopic shift ( P = 0.76) ( Figure 3 ). In addition, there was no correlation between hyperopic shift and donor graft thickness at about 6 months of follow-up ( P = 0.26) ( Figure 4 ).
Intraocular Pressure Measurement
The mean baseline IOP measurement for the study population was 15.0 (± 4.3) mm Hg. At about the 6-month follow-up time point, there was no change in the IOP measurement in our study population (mean change = 0.19 ± 4.8 mm Hg). Mean change in IOP measurement for group 1 was 0.15 ± 2.9 mm Hg. This is comparable to the results achieved by group 2 (mean = 0.41 ± 5.4 mm Hg) and group 3 (mean = −0.65 ± 4.12 mm Hg). There was no statistically significant difference among the three groups in the change in IOP measurement ( P = 0.56) ( Figure 5 ). In addition, there was no correlation between IOP measurement and donor graft thickness at about 6 months of follow-up ( P = 0.95) ( Figure 6 ).




