Purpose
To determine if the location of neodymium:yttrium–aluminum–garnet laser peripheral iridotomy (LPI) is related to the occurrence of postoperative visual dysphotopsia.
Design
Randomized, prospective, single-masked, paired-eye comparative clinical trial.
Methods
setting : Private subspecialty clinic in Mississauga, Canada. study population : Patients with primary angle closure or primary angle-closure suspects were recruited and randomized to receive LPI temporally in one eye and superiorly in the other. Patients were masked to the location of treatment in each eye. intervention : Temporal or superior LPI. main outcome measures : Occurrence of new-onset linear dysphotopsia. Other visual disturbances also were assessed using a questionnaire before and 1 month after intervention. Secondary outcome measures included eyelid position, laser parameters, and any intraoperative complications.
Results
A total of 208 patients were recruited to the study, of which 169 (84%) completed it. New-onset linear dysphotopsia was reported in 18 (10.7%) eyes with superior LPI versus 4 (2.4%) eyes with temporal LPI ( P = .002). Eleven eyes (6.5%) with superior LPI reported linear dysphotopsia despite complete eyelid coverage of the iridotomy. No significant differences were found with other visual disturbances between them. There was more pain experienced by the temporal LPI (2.8 ± 2.2 vs 2.1 ± 2.0; P = .001), despite no difference in laser energy or number of shots. Intraoperative rates of hemorrhage were similar (8.9% vs 10.1%; P = .71).
Conclusions
Temporal placement of LPI is safe and was found to be less likely to result in linear dysphotopsia as compared with superior placement. Temporal iris therefore may be considered a preferred location for LPI.
Laser peripheral iridotomy (LPI) with neodymium:yttrium–aluminum–garnet laser treatment is performed frequently in patients with narrow angles to relieve pupil block and to reduce the risk of acute and chronic angle-closure glaucoma. Side effects associated with LPI typically are benign and include transient blurred vision, transient intraocular pressure rise, transient uveitis, and hyphema. More severe complications can include corneal trauma, cataract, closure of the iridotomy, and retinal detachment.
Visual disturbances or dysphotopsias have been reported in 2.7% to 4% of patients after LPI, but few studies have addressed this specific issue. These dysphotopsias can manifest as haloes, lines, ghost images, glare, shadows, crescents, and so forth. Murphy and Trope first reported linear dysphotopsias that they described as the presence of a blurred or a colored line occurring after superior LPI in a previously asymptomatic patient. Their patient had a patent iridotomy partially exposed by the upper lid, and they hypothesized that placement of the iridotomy entirely under the upped eyelid might have avoided linear dysphotopsia. After Murphy and Trope’s report, Weintraub and Berke reported 4 cases with similar symptoms of linear dysphotopsia in the inferior hemifield after superior LPI, despite full coverage by upper eyelid. They hypothesized that a base-up prism effect of the tear meniscus at the upper lid margin may have redirected incoming light superiorly through the LPI, despite its position behind the lid. They also found that altering the light path by either raising or lowering the upper eyelid, thereby disrupting the tear meniscus, resulted in resolution of the dysphotopsias.
However, a recent paper by Congdon and associates prospectively compared 217 subjects with superior LPI with 250 controls. Some LPIs were totally covered by the lid, some were partly covered by the lid, and some were uncovered by the lid. Straylight and prevalence of visual symptoms were rare in their study and did not differ between treated subjects and controls regardless of lid coverage, size of the LPI, or iris color.
The purpose of our study was to determine if the location of the LPI, superior or temporal, affected the incidence of dysphotopsia after surgery. Specifically, we were interested in linear dysphotopsia because these are most specific to LPIs and most problematic to patients.
Methods
A prospective, randomized, single-masked, paired-eye study was performed with Institutional Review Board Services (Aurora, Ontario, Canada) approval and was registered at ClinicalTrials.gov (no. NCT01758237). All primary angle-closure patients and primary angle-closure suspects seen in the subspecialty clinic in Mississauga, Ontario, Canada, were invited to participate. The inclusion criteria were patients with an indication for LPI who were older than 18 years, were able and willing to give consent, were able to follow study instructions, and were able to attend the required study visits. Patients were excluded if they had any previous intraocular surgery, corrected distance visual acuity worse than 20/40, asymmetrical ptosis of more than 2 mm, active intraocular inflammation, or a history of acute-attack angle-closure glaucoma. Before surgery, age, gender, race, and corrected distance visual acuity were recorded and a questionnaire on visual disturbance symptoms was administered ( Supplemental Material , available at AJO.com ).
Using a binary random number generator, one eye was selected and then randomized using the same method to an LPI in the temporal location or superior location. The other eye by default was assigned the opposite location. Patients were masked to the location of treatment performed in each eye. The LPI was performed using the neodymium:yttrium–aluminum–garnet laser using an Abraham iridectomy lens (Ocular Instruments Inc., Bellevue, Wasington, USA). Superior LPIs were place between 11 and 1 o’clock with an attempt to place as peripheral as possible and under the superior eyelid. Temporal LPIs were placed between 2 and 4 o’clock (for left eyes) or between 8 and 10 o’clock (for right eyes), being careful to avoid placing near the lid margin for patients whose lid crossed near the temporal cornea. Preference was made for iris crypts, while avoiding iris vessels. Both LPIs were performed sequentially at the same visit. Intraoperative data collected included iris color, number of laser shots, energy used, a subjective rating of pain on a scale from 0 to 10, and the occurrence of any complications.
Each patient had a follow-up visit 1 month after LPI, during which the same visual symptom questionnaire was administered. This was followed by corrected distance visual acuity, slit-lamp, gonioscopic, and external examinations to measure palpebral fissure, margin reflex distance, presence of cataract, location and size of LPI, its distance from the limbus, and the degree of eyelid coverage. The primary outcome measure was the presence of new linear dysphotopsias. Secondary outcomes included the presence of other visual dysphotopsias, laser parameters, pain experienced during the procedure, and complications.
A sample size of 163 patients (163 eyes per group) was calculated based on an estimated of incidence of 10% linear dysphotopsias in the superior LPI group versus 3% in the temporal group (power, 80%; α, 0.05). This was based on previously unpublished pilot study data. To account for a 15% dropout rate, a total of 200 patients were planned to be recruited.
Statistical analyses were carried out using the Statistical Package for the Social Sciences version 15 (IBM, Chicago, Illinois, USA). Paired t tests were used for comparison of the neodymium:yttrium–aluminum–garnet laser settings. The Mann–Whitney U test or Wilcoxon signed-rank test were used for all other analysis. Correlation between eye color and dysphotopsia was performed using binary logistic regression. Significance was set at P = .05.
Results
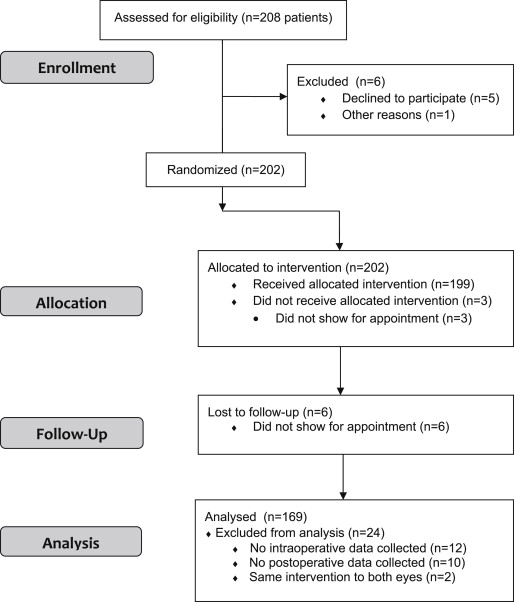
A total of 208 patients were eligible for recruitment into the study. Of those, 202 patients were enrolled and 199 of these underwent the intervention. There were 169 (81.3%) patients who completed their questionnaires and examinations before and after laser treatment and underwent the correct treatments in either eye ( Figure 1 ). Two patients received the same intervention in both eyes, and so were excluded from the analysis. In total, 338 eyes from the 169 patients were included in the data analysis. Demographic characteristics for these patients are listed in Table 1 .
| No. of patients | 169 |
| Mean age ± SD, y | 53.4 ± 11.5 |
| Male / female gender, n (%) | 52 (30.8)/117 (69.2) |
| Race, n (%) | |
| Black | 9 (5.3) |
| Asian | 11 (6.5) |
| White | 85 (50.3) |
| Hispanic | 5 (3.0) |
| South Asian | 59 (34.9) |
There was no statistically significant difference in the mean laser energy used (4.99 ± 1.13 mJ vs 5.06 ± 2.07 mJ; P = .733), number of shots (8.1 ± 8.4 vs 8.7 ± 16.7; P = .684), and total energy (41.5 ± 48.2 mJ vs 47.1 ± 107.9 mJ; P = .539) used to perform the LPI between the superior and temporal locations. Subjective pain grading scores showed temporal LPIs were significantly more painful than superior LPIs (2.8 ± 2.2 vs 2.1 ± 2.0; P < .001). There was also no difference in the presence of intraoperative hemorrhage, which was graded as mild, between superior or temporal LPIs (8.9% vs 10.1%; P = .71).
Before LPI, 94 patients (55.6%) experienced 1 or more dysphotopsias ( Table 2 ). Rates of each dysphotopsia before LPI were similar in both superior and temporal LPI eyes with no significant difference. Of dysphotopsias present before laser, glare, blurred vision, and haloes tended to more common, whereas linear dysphotopsias were present in only 3 (0.9%) of 338 eyes.
| Variable | Superior LPI | Temporal LPI | ||||
|---|---|---|---|---|---|---|
| Before Laser | After Laser | P Value a | Before Laser | After Laser | P Value a | |
| Halo | 23 | 8 | .002 | 23 | 10 | .007 |
| Lines | 1 | 18 | <.001 | 2 | 5 | .180 |
| Crescent | 4 | 2 | .317 | 2 | 1 | .317 |
| Glare | 33 | 23 | .059 | 33 | 22 | .048 |
| Ghost images | 14 | 4 | .008 | 14 | 5 | .013 |
| Shadows | 8 | 7 | .763 | 8 | 8 | 1.00 |
| Blurry vision | 28 | 33 | .369 | 28 | 35 | .209 |
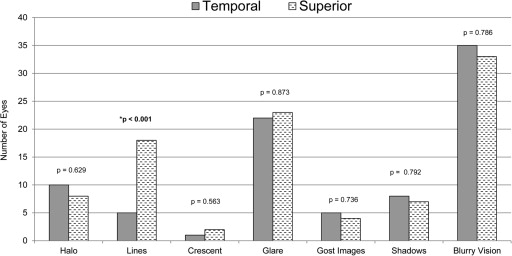
After LPI, there were no differences in reported dysphotopsia from before LPI for both superiorly treated and temporally treated eyes, with the exception of linear dysphotopsia and halos ( Table 2 ). After LPI, 23 (6.8%) eyes demonstrated linear dysphotopsias. There were 18 eyes (10.7%) that had undergone superior LPI as compared with 5 (3.0%) eyes that had undergone temporal LPI, one of which had the same dysphotopsia before laser treatment. This was a statistically significant difference ( P = .002; Figure 2 ). Thus, the number of new-onset linear dysphotopsias after laser treatment was 18 (10.7%) for superior LPI eyes versus 4 (2.4%) for temporal LPI eyes ( P = .002). In 2 patients, linear dysphotopsia present before LPI resolved after LPI, 1 in each group. There were 2 patients who demonstrated linear dysphotopsias in both eyes after LPI. The presence of haloes and ghost images seemed to improve in a significant number of patients after LPI regardless of location ( Table 2 ).