Fig. 7.1
Concept of aging
The free radical theory: Generation of reactive oxygen species (ROS) eventually overwhelms the counteracting antioxidant defenses leading to cellular damage and aging. The metabolic theory: Overeating creates metabolic stress on the body, which can lead to a shorter life span and serious age-related diseases.
7.1.2 Lacrimal Gland Change with Age
Aging is an important risk factor of dry eye. Age-related changes in the lacrimal gland are associated with alterations in the structural organization and functional response in the lacrimal gland (Damato et al. 1984; Sullivan et al. 1990; Obata et al. 1995). These changes include increased acinar atrophy, periductal fibrosis and accumulation of lipofuscin-like inclusions, and an increase in inflammatory infiltrates, which contain mast cells and lymphocytes (Damato et al. 1984; Obata et al. 1995; Williams et al. 1994; Draper et al. 1998; Ríos et al. 2005):
Histopathological change
Acinar cell atrophy
Fibrosis
Ductal dilation
Infiltration
Accumulation of lipofuscin
Lacrimal gland hypofunction
Expanded acinar cells
Accumulated enlarged secretory vesicle in the cytoplasm
Decreased endoplasmic reticulum
Increase in the nuclei with dark nucleoplasm
7.2 New Perspective on Dry Eye Diagnosis
The two major etiological causes of dry eye are aqueous tear-deficient dry eye and evaporative dry eye:
Aqueous tear-deficient dry eye
Evaporative dry eye (short BUT dry eye)
7.2.1 Aqueous Tear-Deficient Dry Eye
Aqueous-deficient dry eye is mainly caused by disorders of the lacrimal gland and occurs in Sjögren’s syndrome–type and non-Sjögren’s syndrome–type dry eye. Aqueous-deficient dry eye has two major groupings, Sjögren’s syndrome dry eye and non-Sjögren’s syndrome dry eye. Sjögren’s syndrome–type dry eye results from destruction of the lacrimal gland by lymphocytic infiltration and often induces severe epithelial damage.
One increasingly recognized version of non-Sjögren’s syndrome dry eye may be caused by work involving the use of VDTs (visual display terminals/computer screens). VDT has been increasing with the development of information technology in the office environment and daily life. Many computer users suffer from dry eye related to VDT work. One of the causes for VDT-related dry eye is a decreased blinking frequency inducing the excessive evaporation of tear fluid (Tsubota and Nakamori 1993, 1995; Acosta et al. 1999; Kojima et al. 2011; Tsubota et al. 1996). Another cause may be lacrimal gland hypofunction (Nakamura et al. 2010; Kamoi et al. 2012). The mechanism of VDT-related dry eye was recently revealed showing that excessive secretory vesicle accumulation in the acinar epithelia resulting from the decreased blink frequency in VDT users may induce a failure of tear secretion (Figs. 7.2 and 7.3). There is a negative relationship between VDT use duration and tear secretion. Characteristically, working long hours using a VDT for many years may be a risk factor for inducing non-SS dry eye among VDT users. A new type of dry eye, lacrimal gland hypofunction, is advocated as a dry eye mechanism.
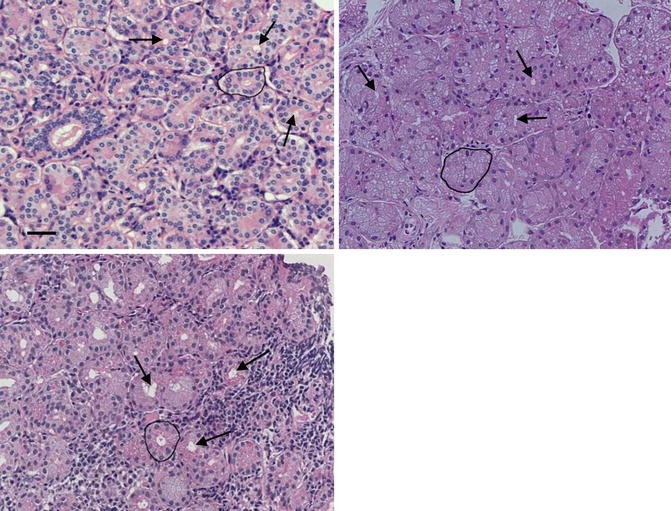
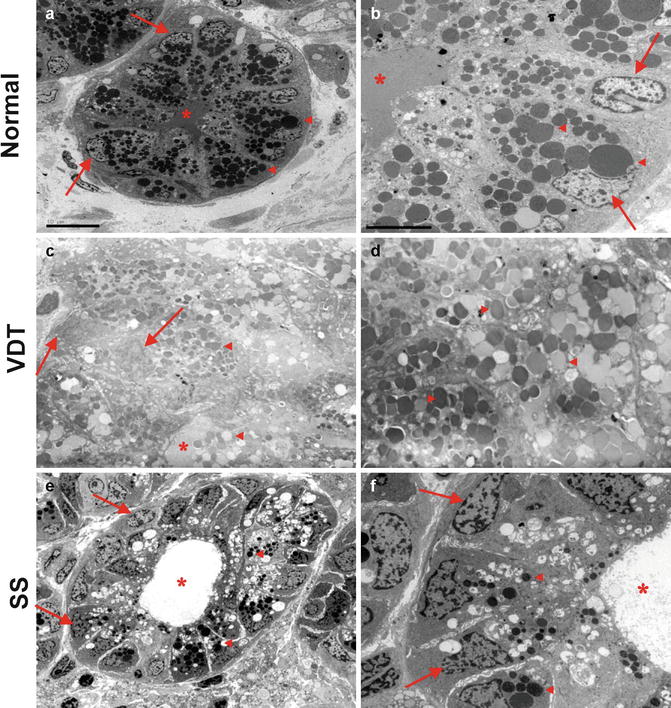
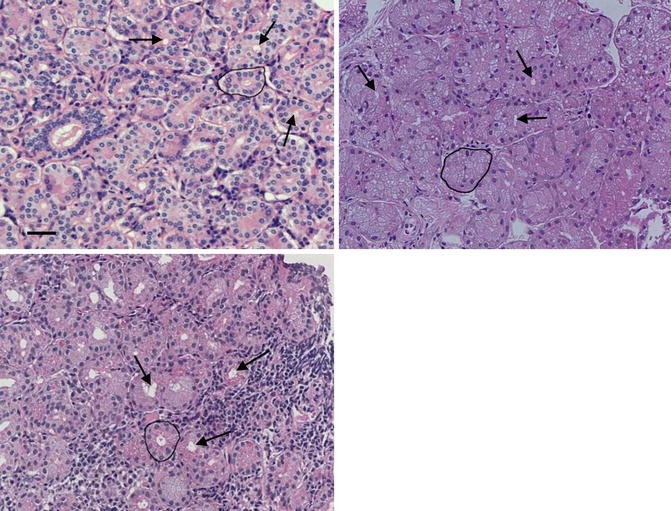
Fig. 7.2
An excessive secretory vesicle accumulation. H&E staining of lacrimal gland. (a) Normal control. The lacrimal gland structure consists of normal acinar cells, ductal cells, capillaries, and connective tissue. (b) Dry eye patient with VDT work. The lacrimal gland acini are larger than those in normal controls and show ductal obstruction. (c) Dry eye patient with Sjögren’s syndrome. The destruction of acini with lymphocytic infiltration and ductal dilation are shown. Arrows: ductal lumens. Circle: one acinus. Scale bars = 50 mm (Reprinted with permission from Kamoi et al. (2012))
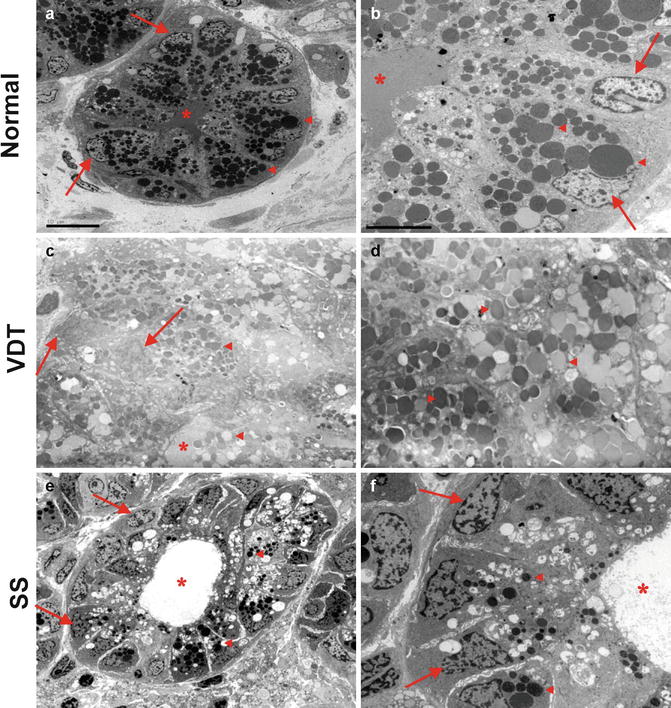
Fig. 7.3
Electron microscopic findings of the lacrimal gland. (a) Secretory vesicle (SV) accumulation in the normal. Scale bars = 10 mm. (b) Homogeneous SVs in normal controls. Scale bars = 5 mm (a, b) Show that SVs accumulated homogeneously toward the apical region of the lacrimal gland epithelial cells. (c) Excessive accumulation of SVs in the VDT group. (d) High-magnification view of SVs in the VDT group. (c, d) Show excessive accumulation of SVs and the nuclei displaced toward the cell periphery by the SVs, which filled the cytoplasm, in the VDT group. SVs of both high and low electron density are observed. (e) Only a few SVs in the SS group. (f) High-magnification view of SVs in the SS group. Figures (e, f) show only a few SVs and dilation of the duct. The SVs are also smaller than those in the normal and VDT groups. The TEM findings indicate that the VDT group has an unusually large number of SVs in the cytoplasm of the lacrimal gland epithelial cells compared with the other two groups. Original magnification: 62,000 (a, c, e), 65,000 (b, d, f). Asterisk, ductal lumen; Arrows, nuclei; triangle, SV (Reprinted with permission from Kamoi et al. (2012))
VDT/computer may be caused by lacrimal gland hypofunction due to reduced blink frequency.
7.2.2 Evaporative Dry Eye
Evaporative dry eye, which is the so-called short breakup time (BUT) dry eye, is characterized by excessive evaporation of the tear film layer from the ocular surface, while tear secretion is normal. Two major BUT patterns have been observed: one is a dry round spot pattern, and the other is a longitudinal tear break pattern (Fig. 7.4). It is sometimes misunderstood that short BUT dry eye represents an early milder form of dry eye, since it is associated with little or no corneal epithelial damage (Sullivan et al. 2010, 2012; Lemp et al. 2011). However, short BUT dry eye is strongly symptomatic. Dry eye symptoms may present as eye fatigue, discomfort, or heaviness but also as visual blur or discomfort during daily activities due to the impaired stability and regularity of tear film, despite a normal tear volume and the absence of corneal staining (Toda et al. 1993; Montes-Mico et al. 2004; Ridder et al. 2005, 2011; Goto et al. 2006; Tong et al. 2010; Walker et al. 2010; Koh et al. 2008; Kaido et al. 2012a).
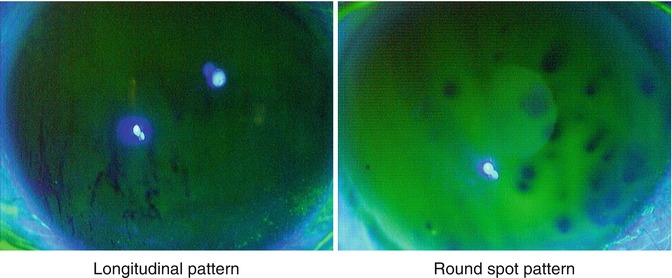
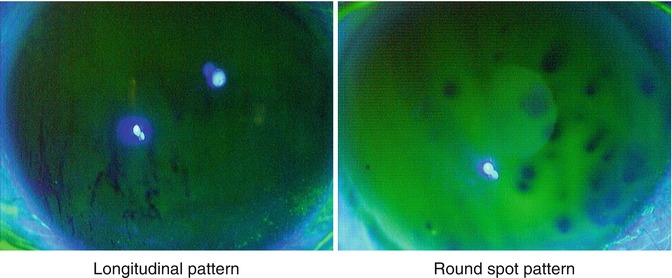
Fig. 7.4
Tear film breakup patterns. Left: Longitudinal tear break pattern is typically observed in elder females. Right: Round spot tear break pattern, which is observed equally in young males and females, may be related to allergic conjunctivitis and VDT work
It seems that short BUT dry eye patients have increased recently in office workers who perform VDT work and wear contact lenses. The etiology has been classified as intrinsic causes (meibomian gland dysfunction (MGD), disorders of lid aperture, low blink rate) or extrinsic causes (vitamin A deficiency; topical drug preservatives, such as benzalkonium chloride (BAC); contact lens wear; and ocular surface disease, e.g., allergy) (Smith et al. 2007). One of the etiological explanations for the short BUT may be decreased goblet cell density (Toda et al. 1993, 1995; Watanabe 2002).
Short tear breakup time dry eye/evaporative tear loss is a major cause of dry eye in office workers. Loss of goblet cells may be an important factor.
7.3 New Examinations for the Tear Function Assessment
Strip meniscometry
TearLab Osmolarity
Oily layer assessment: DR-1
Functional visual acuity measurement system
7.3.1 Strip Meniscometry
Several methods are used for the assessment of dry eye diseases, including the Schirmer test, invasive and noninvasive tear film breakup time assessment, vital stainings, and tear meniscus evaluation. The Schirmer test is an indispensable tool for tear volume assessment; however, there is wide intrasubject and time-wise variability, as well as problems of irritation and induction of reflex tearing.
Strip meniscometry (SM) is a novel, simple, noninvasive method for measuring the tear meniscus volume (Dogru et al. 2006; Ibrahim et al. 2011). It is designed to avoid induction of reflex tearing and is promoted to be mechanically produced with high quality. The strip is applied to the lateral lower lid tear meniscus without touching the ocular surface for 5 s. The length of the stained tear column in the central membrane ditch is regarded as the SM value (Fig. 7.5).
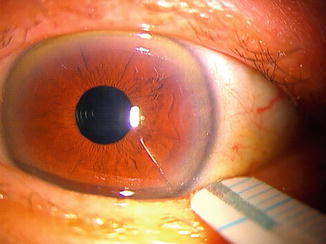
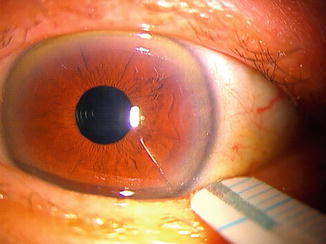
Fig. 7.5
Strip meniscometry. The strip is applied to the lateral lower lid tear meniscus without touching the ocular surface. Length of the stained tear column in the central membrane ditch is regarded as the strip meniscometry value
The strip is composed of polyethylene terephthalate, on which is pasted a urethane-based material of the same size containing a central ditch of 0.40 mm in depth. A nitrocellulose membrane filter paper strip with a pore size of 8 μm impregnated in natural blue dye is then placed into the central ditch.
The SM has a strong correlation with the Schirmer test, BUT, ocular surface vital staining scores, and tear film lipid layer interferometry grades. It is noted that sensitivity and specificity for dry eye diagnosis are high, such as 80.5 and 67.2 % using a single SM, and elevated to 80.5 and 99.3 % using SM and BUT values (Ibrahim et al. 2011).
7.3.2 TearLab Osmolarity
The TearLab Osmolarity System is the first objective and quantitative test for diagnosing and managing dry eye patients (Lemp and Foulks 2007; Nichols and Sinnott 2006; Lemp et al. 2013). The TearLab Osmolarity System is intended to measure the osmolarity of human tears to aid in the diagnosis of patients suspected of having dry eye disease, in conjunction with other methods of clinical evaluation (Fig. 7.6). Hyperosmolarity has been described in the literature as a primary marker of tear film integrity. When the quantity or quality of secreted tears is compromised, increased rates of evaporation lead to a more concentrated tear film (increased osmolarity) that places stress on the corneal epithelium and conjunctiva. The system has been shown to correctly identify 88 % of normal tear subjects, 75 % of mild-to-moderate dry eye disease subjects, and 95 % of severe dry eye disease subjects (Lemp and Foulks 2007).


Fig. 7.6
TearLab Osmolarity (Courtesy of TearLab Corp., San Diego, CA)
7.3.3 DR-1
The DR-1 device (Kowa Co., Nagoya, Japan) is the specific interference camera to visualize the precorneal lipid layer spread (Goto et al. 2003). The interference color chart allows quantification of the interference images, which are graded corresponding to dry eye severity. The DR-1 images were classified from grades 1–5 as follows: grade 1, somewhat gray color and uniform distribution; grade 2, somewhat gray color and nonuniform distribution; grade 3, a few colors and nonuniform distribution; grade 4, many colors and nonuniform distribution; and grade 5, corneal surface partially exposed (Fig. 7.7). It is noted that the severity of dryness on the ocular surface and meibomian gland dysfunction is related to the grades of interference patterns.
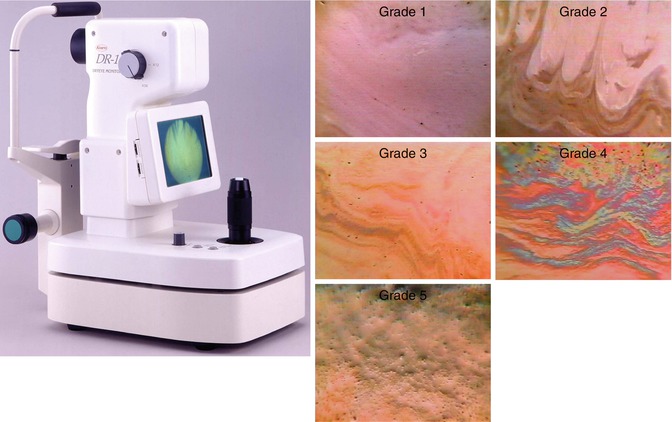
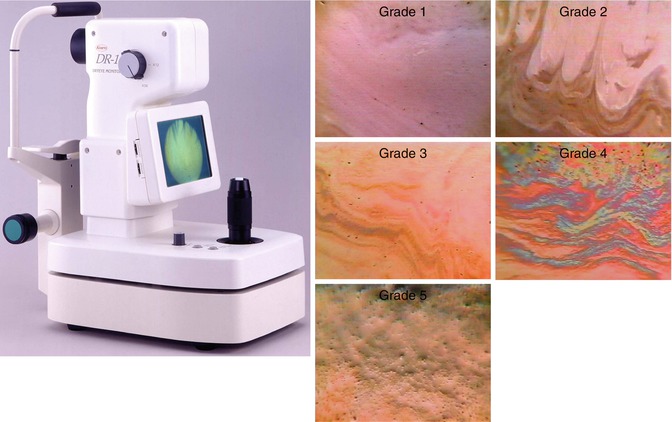
Fig. 7.7
The DR-1 images (Courtesy of Norihiko Yokoi, Kyoto Prefectural University of Medicine)
DR-1 Grading Scores
Grade 1—somewhat gray color and uniform distribution
Grade 2—somewhat gray color and nonuniform distribution
Grade 3—a few colors and nonuniform distribution
Grade 4—many colors and nonuniform distribution
Grade 5—corneal surface partially exposed
7.3.4 Functional Visual Acuity Measurement System
The 2007 International Dry Eye Workshop Epidemiology Subcommittee recommended inclusion of an item on visual function in the definition of dry eye―including fluctuation of vision or transient blurred vision―to capture the effect of ocular surface dryness on visual function and assist in defining a clinically meaningful situation (Smith et al. 2007). Standard visual acuity testing measures instantaneous visual acuity and has been traditionally accepted for assessing the visual function; however, standard testing may have limitations to assess the quality of vision. Several methods, such as contrast sensitivity, corneal topography, glare test, wavefront sensor, and functional visual acuity measurement system, have been developed to assess the quality of an individual’s visual acuity.
Functional visual acuity measurement system (Kowa Co., Nagoya, Japan) is a device that examines the change in visual acuity over time (Fig. 7.8). Functional VA is an index of mean VA value over time. A stable tear film over the corneal surface is essential for clear visual imaging, and an irregular corneal surface resulting from dry eyes is associated with poor quality of vision. Functional visual acuity is effective in evaluating dynamic visual function changes relating with tear film (Ishida et al. 2005; Kaido et al. 2011, 2012a, b).
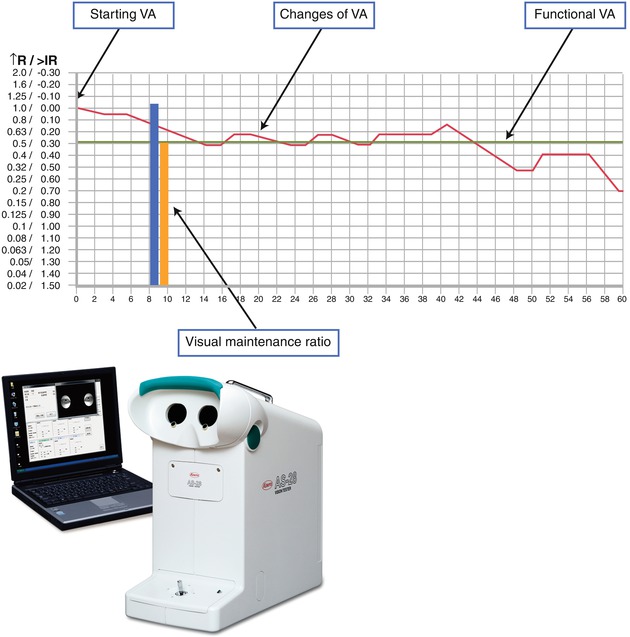
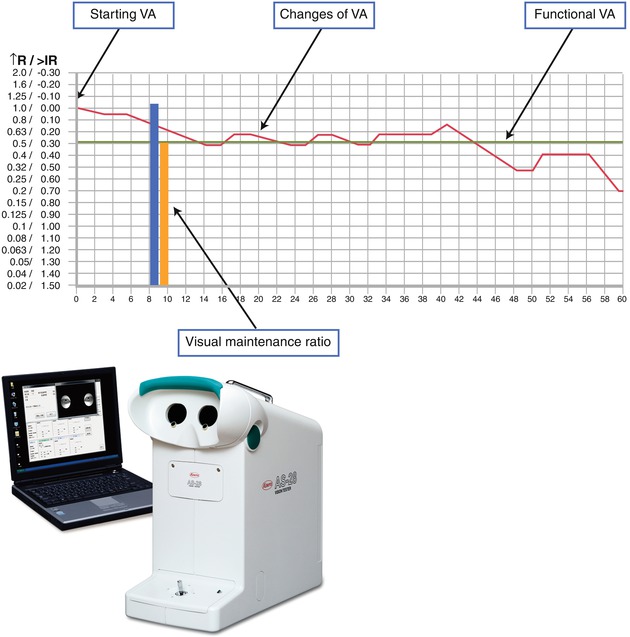
Fig. 7.8
Functional visual acuity measurement system. Upper: functional visual acuity measurement system (Kowa Co., Nagoya, Japan). Lower: the sequential changes in visual acuity over time
Index of Functional Visual Acuity Measurement
1.
Starting visual acuity: baseline visual acuity starting with best corrected visual acuity
2.
Functional visual acuity: the mean VA score of only the correct responses during the measurement period
3.
Visual maintenance ratio: the ratio of functional VA divided by the value of baseline VA
4.
Maximal visual acuity: the highest visual acuity during the measurement period
5.
Minimal visual acuity: the lowest VA score during the measurement period
6.
Response reaction time
7.
Blink frequency
7.4 Dry Eye Treatments
7.4.1 New Equipment for Dry Eye Treatments
JINS Moisture glasses are designed for the protection of the eyes from dryness. These have a small container filled with water on the side (Fig. 7.9). The moisture glasses are suitable for anyone who suffers from severe eye pain due to dryness but also experiences the irritation that comes with sitting in front of a computer screen for a few hours.


Fig. 7.9
JINS Moisture glasses
7.4.2 Dry Eye Treatments on Tear Film–Oriented Therapy
Tear film–oriented therapy (TFOT) is a new strategic direction for treating dry eye. Tear film stability and regularity are based on the balance of the trilaminar tear film—consisting of lipid, aqueous, and mucin layers—on the ocular surface. Lipid meibom reduces aqueous evaporation. The lacrimal glands produce the tears that make up the aqueous layer, and mucins provide wettability and an intimate layer of protection at the corneal and conjunctival surface. The TFOT is the treatment targeting the specific tear layers on the ocular surface (Fig. 7.10).
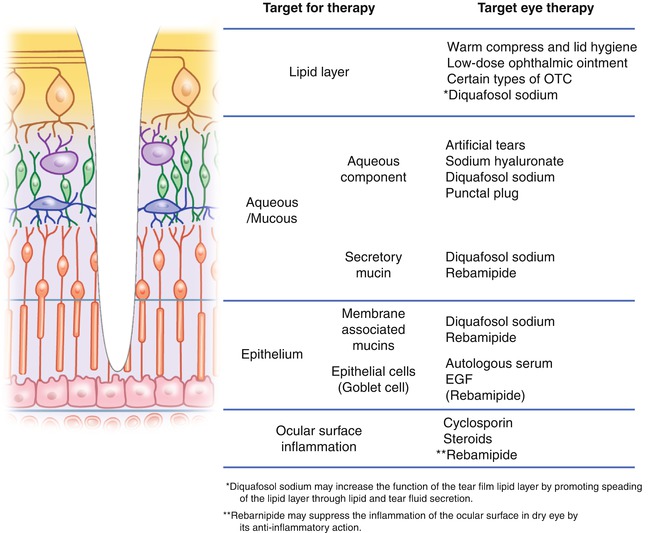
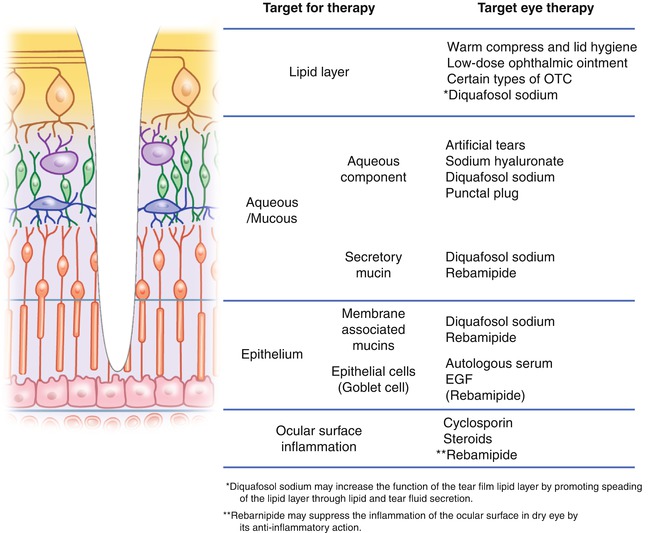
Fig. 7.10
Tear film-oriented therapy (TFOT) (Courtesy of the Japanese Dry Eye Society)
New Eye Drops for Tear Film–Orientated Therapy (TFOT)
Diquafosol tetrasodium ophthalmic solution
Rebamipide ophthalmic solution
7.4.3 Diquafosol Tetrasodium Ophthalmic Solution
Diquafosol tetrasodium, a P2Y2 receptor agonist, is a new preparation of eye drops that stimulates tear and mucin secretion which improves tear film stability (Fujihara et al. 2001, 2002; Takaoka-Shichijo and Nakamura 2011). The induction of mucin production from the ocular surface may increase the stability of the tear film. It is noted that the administration of diquafosol tetrasodium ophthalmic solution has beneficial effects on tear film stability and/or optical quality and on visual performance in short BUT dry eye (Kaido et al. 2013).
7.4.4 Rebamipide Ophthalmic Suspension
Rebamipide, an amino acid derivative of 2(1H)-quinolinone, is originally a gastroprotective drug, which has been used for mucosal protection, healing of gastroduodenal ulcers, and treatment of gastritis (Uchida et al. 1985). Rebamipide suspension was then developed more recently for use in the ophthalmic field. The therapeutic effects of rebamipide demonstrate an increase in corneal and conjunctival mucin-like substances and improve corneal and conjunctival injury in vivo (Urashima et al. 2004). It is noted that rebamipide increased the mucin production in cultured conjunctival goblet cells and in corneal epithelial cells (Rios et al. 2006, 2008).
7.5 New Dry Eye Approach with Oral Supplements
New Approach on Oral Supplement
Lactoferrin
Omega-3 fatty acids
Tear lactoferrin level, which is an indicator of lacrimal secretory function, is decreased in dry eye (Danjo et al. 1994). Lacrimal gland secretory function is correlated with age-induced dry eye disease in rats, which may stem from oxidative stress; lactoferrin concentration in tears decreases with age (Jensen et al. 1986; McGill et al. 1984).
Lactoferrin has an antioxidant effect in that it binds free iron, thus preventing the production of hydroxyl radicals. Lactoferrin is also known to have an anti–inflammatory effect. The increased occurrence of eye surface infections and the uncontrolled development of inflammation typical of dry eye have been reported to be a result of the reduced amount of lactoferrin in the tear film (Baveye et al. 1999; Kanyshkova et al. 2001; Legrand et al. 2005).
It has been shown that oral lactoferrin administration preserves lacrimal gland function in aged mice by attenuating oxidative damage and suppressing subsequent gland inflammation (Kawashima et al. 2012). One report showed the improvement of tear stability and ocular surface damage in patients with Sjögren’s syndrome by the oral lactoferrin supplementation (Dogru et al. 2007). Lactoferrin supplementation is expected to be a safe and effective therapy for age-related decline of lacrimal gland dysfunction by attenuating oxidative damage and suppressing subsequent gland inflammation.
Lactoferrin
An iron-binding glycoprotein present in serum and exocrine secretions
Anti-inflammatory effects
The promotion of cell growth and DNA synthesis
Exhibition of anti-angiogenic and anti-tumorigenic properties
Antioxidative and carcinogenic bioactivities
7.5.1 Omega-3 Fatty Acids
Omega–3 fatty acids, including docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), and alpha-linolenic acid (ALA), cannot be synthesized by the human body but are vital for normal metabolism. DHA, the major polyunsaturated fatty acid found in retinal rod outer segments, is noted to play a role in the prevention of age-related macular degeneration and dry eye syndrome (Miljanović et al. 2005). Omega-3 essential fatty acids have anti–inflammatory effects and inhibit multiple aspects of inflammatory response as demonstrated in the lacrimal gland where omega-3s prevent apoptosis of the secretory epithelial cells. Supplementation is expected to clear meibomitis, allowing a thinner, more elastic lipid layer to protect the tear film and cornea and treat dry eye disease.
7.6 Dry Eye Treatments by an Antiaging Approach
Because dry eye is exacerbated by aging, a useful approach for the prevention or treatment of dry eye may be to interfere with the aging process.
Prevention of cellular oxidation and calorie restriction may slow or prevent aging and therefore dry eye.
Antiaging medicine may expand the possibilities for the dry eye treatments. Age-related changes in tears and lacrimal gland secretary function lead to an increased prevalence of dry eye disease (Moss et al. 2000; Schaumberg et al. 2003, 2009; Chia et al. 2003; Lin et al. 2003; Uchino et al. 2006; Viso et al. 2009). The aging process may be managed by controlling reactive oxygen species or levels of calories as an antiaging strategy (Harman 1956; Frisard and Ravussin 2006; Matsuzawa 2006). The two important antiaging strategies, prevention of cellular oxidation and calorie restriction, are examined, and how to apply these theories for the prevention and treatment of dry eye is discussed below.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


