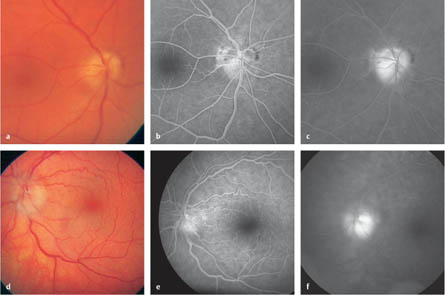
10.1 Differential Diagnosis in Optic Disc Swelling and Anterior Ischemic Optic Neuropathy – Anterior ischemic optic neuropathy (AION), arteritic or nonarteritic – Inflammation due to autoimmune reactions (e. g., optic neuritis, sarcoidosis, or uveitis) or due to infection (e. g., toxoplasmosis, borreliosis, and syphilis) – Intracranial hypertension (papilledema) – Tumors (glioma, meningioma, orbital tumors) – Anomalies (optic disc drusen, hyperopia) – Rare: Leber’s congenital amaurosis, radiation optic neuropathy, ocular hypotony, side effects of drugs Fig. 10.1a–f Differential diagnosis in optic disc swelling and anterior ischemic optic neuropathy a Color photograph. Anterior ischemic optic neuropathy, with mild optic disc swelling. The optic disc swelling is more noticeable below than above (segmental). Individual areas of hemorrhage are visible in the temporal area on the edge of the optic disc. b Arteriovenous phase. There is a filling delay in the optic disc, with a minimal delay in peripapillary choroidal filling. c Late phase. The leakage remains limited to the optic disc. d Color photograph. Anterior ischemic optic neuropathy: the optic disc is prominent, with indistinct borders. e Arteriovenous phase. There is a filling delay at the top in the optic disc and incipient leakage. f Late phase. The leakage remains limited to the optic disc. Buono LM, Foroozan R, Sergott RC, Savino PJ. Nonarteritic anterior ischemic optic neuropathy. Curr Opin Ophthalmol 2002;13:357–61. Ghanchi FD, Dutton GN. Current concepts in giant cell (temporal) arteritis. Surv Ophthalmol 1997;42:99–123. Hattenauer MG, Leavitt JA, Hotge DO, Grill R, Gray DT. Incidence of nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 1997;123:103–7. Ischemic Optic Neuropathy Decompression Trial Research Group. Optic nerve decompression surgery for nonarteritic ischemic optic neuropathy (NAION) is not effective and may be harmful. JAMA 1995;273:625–32. Fig. 10.1g–i Anterior ischemic optic neuropathy g Color photograph. Anterior ischemic optic neuropathy. The swollen optic disc has indistinct borders. h Early phase. There is mild leakage in the area of the optic disc, with minimal filling delay in the upper temporal area. Dilated capillaries are recognizable on the optic disc. i Late phase. The leakage remains limited to the optic disc. – Days 1–3: 4 × 250 g methylprednisolone as a short infusion – Days 4–14: 1 mg/kg body weight prednisone orally – Day 15: 20 mg prednisone orally – Days 16–18: 10 mg prednisone orally Arnold AC. Evolving management of optic neuritis and multiple sclerosis. Am J Ophthalmol 2005;139:1101–8. Beck RW. Clinically definite multiple sclerosis following optic neuritis. Ann Neurol 1997;42:815–6. Beck RW, Trobe JD. The Optic Neuritis Treatment Trial. Putting the results in perspective. The Optic Neuritis Study Group. J Neuroophthalmol 1995;15:131–5. Beck RW, Trobe JD, Moke PS, et al. High- and low-risk profiles for the development of multiple sclerosis within 10 years after optic neuritis: experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol 2003;121:944–9.
Optic Disc Swelling
 The causes of optic disc swelling can rarely be clearly diagnosed by ophthalmoscopy alone. Usually, the etiology has to be deduced from the case history, accompanying symptoms, and additional diagnostic methods.
The causes of optic disc swelling can rarely be clearly diagnosed by ophthalmoscopy alone. Usually, the etiology has to be deduced from the case history, accompanying symptoms, and additional diagnostic methods.
 Optic disc swelling can be caused by any of the following disorders, for example:
Optic disc swelling can be caused by any of the following disorders, for example:
 Fluorescein angiography is helpful in the diagnostic work-up only when the findings are clear. Examples with classic findings are presented in this chapter.
Fluorescein angiography is helpful in the diagnostic work-up only when the findings are clear. Examples with classic findings are presented in this chapter.
Anterior Ischemic Optic Neuropathy
Epidemiology, Pathophysiology, and Clinical Presentation
 Anterior ischemic optic neuropathy (AION) is the most common form of optic disc swelling.
Anterior ischemic optic neuropathy (AION) is the most common form of optic disc swelling.
 Reduced circulation in the shorter ciliary arteries is caused in two-thirds of cases by arteriosclerotic changes, and in one-third by inflammation. Circulatory dysfunction can develop anterior to, inside, or just behind the lamina cribrosa.
Reduced circulation in the shorter ciliary arteries is caused in two-thirds of cases by arteriosclerotic changes, and in one-third by inflammation. Circulatory dysfunction can develop anterior to, inside, or just behind the lamina cribrosa.
 Reduced perfusion pressure and an acute lack of oxygen then lead to anterior ischemic optic neuropathy, with optic disc swelling caused by blockage of the fast axoplasmic flow.
Reduced perfusion pressure and an acute lack of oxygen then lead to anterior ischemic optic neuropathy, with optic disc swelling caused by blockage of the fast axoplasmic flow.
Nonarteritic Form
 The incidence is one in 10 000 in the general population and 2–10 per 100 000 per year in those over the age of 50. The fellow eye is affected in approximately 19% of cases within 5 years. Men and women are equally at risk.
The incidence is one in 10 000 in the general population and 2–10 per 100 000 per year in those over the age of 50. The fellow eye is affected in approximately 19% of cases within 5 years. Men and women are equally at risk.
 Risk factors are arterial hypertension in 49% of cases and diabetes mellitus in 26%. Other risk factors include sleep apnea syndrome, cardiovascular or cerebrovascular diseases, carotid changes, coagulation dysfunction, and optic disc hypoplasia.
Risk factors are arterial hypertension in 49% of cases and diabetes mellitus in 26%. Other risk factors include sleep apnea syndrome, cardiovascular or cerebrovascular diseases, carotid changes, coagulation dysfunction, and optic disc hypoplasia.
 A sudden unilateral decrease in visual acuity is often experienced (42%) within the first 2 hours after waking. Patients present with visual acuity loss, abnormal color vision, visual field defects (the inferior visual field is affected in 47% of cases), and optic disc swelling.
A sudden unilateral decrease in visual acuity is often experienced (42%) within the first 2 hours after waking. Patients present with visual acuity loss, abnormal color vision, visual field defects (the inferior visual field is affected in 47% of cases), and optic disc swelling.
Arteritic Form (Caused by Arteritis Temporalis, Giant-Cell Arteritis, Horton Disease)
 The incidence is 15–30 per 100 000 per year in those over the age of 50. Without treatment, the fellow eye is affected within a few days in 95% of cases. Women are more often affected than men (3: 1).
The incidence is 15–30 per 100 000 per year in those over the age of 50. Without treatment, the fellow eye is affected within a few days in 95% of cases. Women are more often affected than men (3: 1).
 The typical case history consists of temporal headache and jaw claudication. Double vision, abnormal fatigue, subfebrile temperatures and polymyalgia rheumatica are less frequent.
The typical case history consists of temporal headache and jaw claudication. Double vision, abnormal fatigue, subfebrile temperatures and polymyalgia rheumatica are less frequent.
 Clinically, optic disc swelling, a distinct reduction in visual acuity, tenderness and absent pulsation in the temporal artery, and an increase in the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level are observed. However, the ESR may be normal in up to 20% of the patients.
Clinically, optic disc swelling, a distinct reduction in visual acuity, tenderness and absent pulsation in the temporal artery, and an increase in the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level are observed. However, the ESR may be normal in up to 20% of the patients.
Inflammatory Anterior Ischemic Optic Neuropathy
 Anterior ischemic optic neuropathy can develop due to infection or as a parainfectious finding in association with borreliosis, chlamydiosis, Mycoplasma infection, neurotropic viruses, and paraneoplastic inflammation.
Anterior ischemic optic neuropathy can develop due to infection or as a parainfectious finding in association with borreliosis, chlamydiosis, Mycoplasma infection, neurotropic viruses, and paraneoplastic inflammation.
Clinical Findings for All Forms
 The optic disc often shows focal nerve fiber hemorrhages, diffuse or focal telangiectasis, and sectorial or diffuse swelling. Narrowing of the arteries on the optic disc may also be seen.
The optic disc often shows focal nerve fiber hemorrhages, diffuse or focal telangiectasis, and sectorial or diffuse swelling. Narrowing of the arteries on the optic disc may also be seen.
 Hard exudates are occasionally present in peripapillary area or in the macula.
Hard exudates are occasionally present in peripapillary area or in the macula.
 Resorption of optic disc swelling takes place within 4–8 weeks. Segmental or diffuse paleness appears after resorption.
Resorption of optic disc swelling takes place within 4–8 weeks. Segmental or diffuse paleness appears after resorption.
Fluorescein Angiography
 A delay in filling of the optic disc area and possibly a nominal delay in peripapillary choroidal filling occur in the early phase.
A delay in filling of the optic disc area and possibly a nominal delay in peripapillary choroidal filling occur in the early phase.
 In the later phases, leakage takes place at the optic disc and is limited to that area.
In the later phases, leakage takes place at the optic disc and is limited to that area.
Diagnosis and Treatment
 The diagnostic work-up includes visual acuity, visual field examination, monitoring of eye mobility (for findings such as double vision or movement pain), and ESR and CRP assessment.
The diagnostic work-up includes visual acuity, visual field examination, monitoring of eye mobility (for findings such as double vision or movement pain), and ESR and CRP assessment.
 For differential diagnosis, temporal artery biopsy, Doppler sonography, computed tomography or magnetic resonance imaging (if there is no regression of optic disc swelling), and a check for inflammatory or neo-plastic systemic diseases can be carried out.
For differential diagnosis, temporal artery biopsy, Doppler sonography, computed tomography or magnetic resonance imaging (if there is no regression of optic disc swelling), and a check for inflammatory or neo-plastic systemic diseases can be carried out.
 It is important to exclude possible cardiovascular risk factors (long-term electrocardiography, transesophageal echocardiography). It is also important to exclude autoimmune diseases, particularly in younger patients.
It is important to exclude possible cardiovascular risk factors (long-term electrocardiography, transesophageal echocardiography). It is also important to exclude autoimmune diseases, particularly in younger patients.
Nonarteritic Anterior Ischemic Optic Neuropathy
 It is important to treat the underlying disease and risk factors (diabetes mellitus, hypertension).
It is important to treat the underlying disease and risk factors (diabetes mellitus, hypertension).
 Acetylsalicylic acid (ASA) 100 mg/d can be administered for prophylactic treatment (preferably short-term rather than long-term).
Acetylsalicylic acid (ASA) 100 mg/d can be administered for prophylactic treatment (preferably short-term rather than long-term).
 It is not yet clear whether treatments with isovolemic hemodilution in the acute phase, early administration of anticoagulants, or the administration of levodopa are effective.
It is not yet clear whether treatments with isovolemic hemodilution in the acute phase, early administration of anticoagulants, or the administration of levodopa are effective.
 Vasoconstrictive agents (e. g., ergotamine for migraine or nasal sprays) should be avoided.
Vasoconstrictive agents (e. g., ergotamine for migraine or nasal sprays) should be avoided.
 Visual acuity improves in 10–35% of cases, and relapses are rare.
Visual acuity improves in 10–35% of cases, and relapses are rare.
Arteritic Anterior Ischemic Optic Neuropathy
 Immediate hospital admission for high-dose treatment with corticosteroids (500–1000 mg prednisone equivalent i. v.; two to four single doses per day) is necessary.
Immediate hospital admission for high-dose treatment with corticosteroids (500–1000 mg prednisone equivalent i. v.; two to four single doses per day) is necessary.
 Corticosteroid administration is reduced with repeated ESR testing. Long-term administration of low-dose corticosteroids is necessary.
Corticosteroid administration is reduced with repeated ESR testing. Long-term administration of low-dose corticosteroids is necessary.
 Improvement in visual acuity is rare.
Improvement in visual acuity is rare.
References
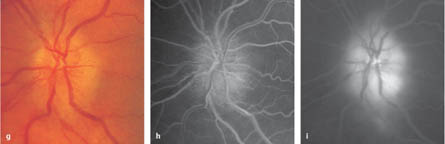
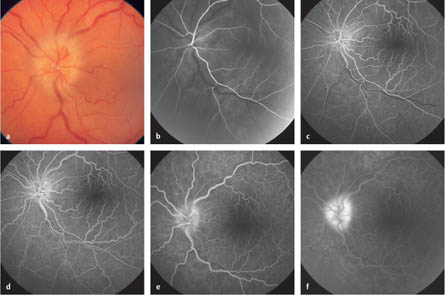
10.2 Optic Neuritis
Epidemiology, Pathophysiology, and Clinical Presentation
 Various diseases have to be distinguished from optic neuritis in the differential diagnosis.
Various diseases have to be distinguished from optic neuritis in the differential diagnosis.
 The most common is optic neuritis caused by autoimmune conditions (with an incidence of five per 100 000 per year). There is a 22% likelihood of multiple sclerosis developing within 10 years if no white-matter lesions are evident on magnetic resonance imaging (MRI). The risk increases to 56% if at least one white-matter lesion is present.
The most common is optic neuritis caused by autoimmune conditions (with an incidence of five per 100 000 per year). There is a 22% likelihood of multiple sclerosis developing within 10 years if no white-matter lesions are evident on magnetic resonance imaging (MRI). The risk increases to 56% if at least one white-matter lesion is present.
 Other autoimmune processes causing optic neuritis include vasculitis, sarcoidosis, lupus erythematosus, panarteritis nodosa, and Crohn disease.
Other autoimmune processes causing optic neuritis include vasculitis, sarcoidosis, lupus erythematosus, panarteritis nodosa, and Crohn disease.
 Inflammatory causes include toxoplasmosis, borreliosis, syphilis, herpes zoster, and parainfectious processes.
Inflammatory causes include toxoplasmosis, borreliosis, syphilis, herpes zoster, and parainfectious processes.
 Toxic causes include side effects of drugs and radiation optic neuropathy.
Toxic causes include side effects of drugs and radiation optic neuropathy.
 Generally, a slow (within days) unilateral decrease in visual acuity develops, and eye movement is painful in 92% of cases.
Generally, a slow (within days) unilateral decrease in visual acuity develops, and eye movement is painful in 92% of cases.
 Visual impairment increases as the body temperature rises.
Visual impairment increases as the body temperature rises.
 A central scotoma develops in the visual field. There is a latency delay in the pattern visual evoked potential (VEP).
A central scotoma develops in the visual field. There is a latency delay in the pattern visual evoked potential (VEP).
 Ophthalmoscopically, a swollen and prominent optic disc can be seen. Hemorrhages at the optic disc are rare.
Ophthalmoscopically, a swollen and prominent optic disc can be seen. Hemorrhages at the optic disc are rare.
 Swelling of the retrobulbar optic nerve can be demonstrated with ultrasonography.
Swelling of the retrobulbar optic nerve can be demonstrated with ultrasonography.
Fluorescein Angiography
 Fluorescein angiography is not necessary for diagnostic purposes. As optic neuritis can be associated with various diseases, familiarity with the findings is important when assessing the angiographic images.
Fluorescein angiography is not necessary for diagnostic purposes. As optic neuritis can be associated with various diseases, familiarity with the findings is important when assessing the angiographic images.
 Early leakage of dye from the dilated capillaries takes place in the early phase.
Early leakage of dye from the dilated capillaries takes place in the early phase.
 Accentuated hyperfluorescence appears in the prominent optic disc areas in the arteriovenous phase.
Accentuated hyperfluorescence appears in the prominent optic disc areas in the arteriovenous phase.
 The leakage remains restricted to the optic disc in the late phase.
The leakage remains restricted to the optic disc in the late phase.
Diagnosis and Treatment
 The diagnosis is based on the typical case history and ophthalmoscopic findings.
The diagnosis is based on the typical case history and ophthalmoscopic findings.
 Pattern VEP is important for follow-up and for examination of the fellow eye.
Pattern VEP is important for follow-up and for examination of the fellow eye.
 MRI of the brain and a neurological examination should be carried out for further clarification.
MRI of the brain and a neurological examination should be carried out for further clarification.
 A serological analysis can be undertaken to clarify the differential diagnosis.
A serological analysis can be undertaken to clarify the differential diagnosis.
 The prognosis and treatment depend on the cause of the optic neuritis.
The prognosis and treatment depend on the cause of the optic neuritis.
 Treatment of optic neuritis is advisable if demyelinating lesions are evident on MRI or the patient is severely affected by reduced visual acuity:
Treatment of optic neuritis is advisable if demyelinating lesions are evident on MRI or the patient is severely affected by reduced visual acuity:
 Combination treatment with immunomodulating agents may be even more promising in order to reduce the risk of multiple sclerosis developing later.
Combination treatment with immunomodulating agents may be even more promising in order to reduce the risk of multiple sclerosis developing later.
 The prognosis for the recovery of visual acuity is relatively good. After 1 month, visual acuity is 1.0 in 65% of the patients and at least 0.5 in 95% of the patients.
The prognosis for the recovery of visual acuity is relatively good. After 1 month, visual acuity is 1.0 in 65% of the patients and at least 0.5 in 95% of the patients.
 Irreversible damage generally develops with other autoimmune processes. Early steroid therapy and, depending on the diagnosis, additional specific general therapy is recommended.
Irreversible damage generally develops with other autoimmune processes. Early steroid therapy and, depending on the diagnosis, additional specific general therapy is recommended.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree