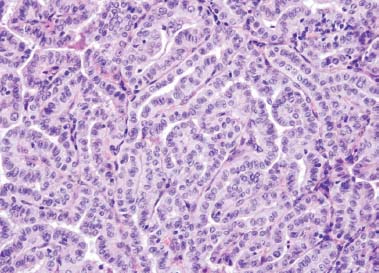
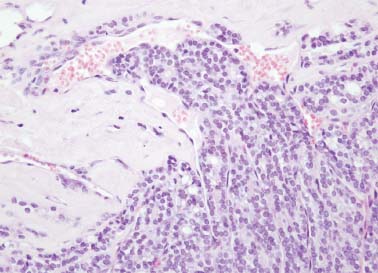
3 Core Messages • Differentiated thyroid carcinomas (DTCs) are the most common endocrine malignancy in humans. • DTCs generally have good prognosis. • The cornerstone of treatment is surgery. • Minimally invasive techniques are emerging as newer options in the treatment of these tumors. Thyroid malignancies account for approximately 1 to 1.5% of all malignancies in humans. It is also the most common among all endocrine malignancies and accounts for 90% of cases. Of these, differentiated thyroid carcinomas (DTCs) alone constitute approximately 95% of the disease bulk. There are three major types of DTCs: papillary thyroid carcinoma (PTC; Fig. 3.1), follicular thyroid carcinoma (FTC; Fig. 3.2), and Hürthle cell tumors. These three variants collectively account for approximately 90% of all DTC cases. The most commonly encountered DTC is papillary thyroid cancer (constitutes 80 to 85% of all cases), followed by follicular thyroid cancer (10 to 20% of all cases) and Hürthle cell cancer (2 to 5% of all DTC cases). The disease is more commonly encountered in women than in men, with a woman to man ratio of 3:1 in most of the studies. Production and secretion of thyroglobulin is the characteristic feature of all types of DTCs. The serum level of this hormone supports correct diagnosis, helps in surgical radicality assessment, and serves as an early biochemical recurrence marker. More than 80% of the patients diagnosed with DTC have good or even excellent prognosis, with approximately 99% 20-year survival rates. However, the remaining 20% of the patients have a less favorable course of disease, with 10-year rates ranging between 20 and 50%.1 In the United States, approximately 20,000 new cases of thyroid carcinoma are diagnosed each year. Some 200,000 patients with thyroid carcinoma are followed-up each year in the United States, and nearly 1500 die from this disease annually. The age at diagnosis ranges between 45 and 50 years. Less than 10% of all DTCs are found in patients younger than 21 years. The clinical course of DTC in children younger than 10 years is less favorable than in older individuals, as is in patients older than 65 years. This fact is not reflected in the current AJCC/TNM (American Joint Committee on Cancer/Tumor-Node-Metastasis) classification, and it also results in poorer outcomes for the whole stage I and II groups (all patients younger than 45 years and independent of extension of the disease are classified as stage I or II; see below for details).2 Various environmental, hormonal, and genetic factors play a role in the development of DTC. The risk of developing DTC is associated with radiation exposure: therapeutic irradiation (e.g., treatment for Hodgkin lymphoma in childhood/adolescence), accidental irradiation (e.g., after explosion in Chernobyl in 1986, 100-fold higher DTC incidence has been noted in several contaminated regions of Belarus and Ukraine), and occupational and geological irradiation. The peak risk of developing DTC is seen 20 to 30 years after irradiation. It is estimated that about 10% of the DTCs may be radiation induced.3 The risk of developing thyroid carcinoma rises linearly with increasing radiation doses. At doses higher than 20 Gy, complete ablation of the thyroid tissue supervenes. One of the factors that cause the development of a DTC is iodine intake. Interestingly, PTC is more common in regions with high iodine intake, while FTC is common in iodine-deficient regions.4 Other environmental factors that possibly play a role in thyroid carcinoma development are retinol, vitamin C, and vitamin E. Approximately 3 to 5% of PTC are inherited as an autosomal dominant trait and are supposed to be more clinically aggressive than the sporadic ones. Familial FTC is extremely rare. In general, familial DTC may be associated with familial adenomatous polyposis, Gardner syndrome, Cowden syndrome, Carney syndrome, or multiple endocrine neoplasia type I. Among genetic mutations that are linked to the pathogenesis of DTC are RAS, RET/PTC, BRAF, PAX8/PPARg, TRK, MET. RAS oncogens are most commonly identified in DTC (up to 80% of FTC, 50% of PTC, and 12% of Hürthle cell carcinoma).4 BRAF proteins are found exclusively in PTC (up to 70% of the cases). Tyrosine kinase oncogenes (RET, TRK, MET) are also typical for PTC (RET in 50%, TRK in 20%, MET in up to 80% of the cases). The only tyrosine kinase oncogene found in FTC (10% of the cases) is MET. FTC is also associated with PAX8/PPARg.5 Figure 3.1 Microphotograph of the classical-type papillary carcinoma. Note the papillary structures and distinctive nuclear features of the tumor. Hematoxylin and eosin stain, magnification ×400. Image courtesy: Prof. Janusz Ryś, Cancer Center Kraków, Poland. According to the Bethesda System for Reporting Thyroid Cytopathology, each thyroid fine-needle aspiration biopsy (FNAB) report should begin with a general diagnostic category. The diagnostic categories are given in Table 3.1. PTC has characteristic cytological features, which can be easily recognized in aspirates from FNAB. Typically, there is a large number of cells that may be grouped into clusters and monolayers or formed papillary arrangements (Fig. 3.1). Other important features that help distinguish PTC from follicular cells are crowding, overlapping, and molding. The defining and diagnostic features of PTC are seen in the nuclei of cancer cells—enlarged nuclei containing dusty (powderlike) chromatin (ground glass nuclei). Contrary to PTC, cytological diagnosis of FTC is often impossible because of microscopic similarity to adenoma. Smears contain numerous clusters of glandular cells, usually arranged in ringlike (follicular) or rossette-like acinar structures (Fig. 3.2). The presence of nuclear atypia does not necessarily imply malignant behavior of tumor. Therefore, the diagnosis of malignancy has to be based on histological and not cytological evaluation. The cytological diagnosis of follicular neoplasm implies obligatory surgical excision and microscopic examination of specimen. Figure 3.2 Microphotograph of follicular carcinoma. Note the vascular invasion in the peripheral portion of the tumor. Hematoxylin and eosin stain, magnification ×200. Image courtesy: Prof. Janusz Ryś, Cancer Center Kraków, Poland. The role of frozen section in the evaluation of thyroid nodules is limited. Artificial changes in microscopic appearance of cells make the assessment of the nuclear features virtually impossible. PTC accounts for 80 to 85% of all cases of malignant epithelial tumors of thyroid. Multifocality is found in 20 to 30% of the cases; however, in some series it can reach 80% depending on the extent of the gland that has been evaluated and the thickness of sections used. Multifocality may be associated with intraglandular metastases, but data from the studies of the clonal rearrangements or X chromosome inactivation patterns support rather the simultaneous growth of multiple primary tumors in most patients. Patients with PTC generally have an excellent prognosis with 95% 10-year survival. PTC presents a variety of macroscopic patterns. Most commonly, it presents as a gray-white mass with irregular margins. Calcifications may also be noticed on gross examination. PTC can present as solid and/or cystic tumor; however, entirely cystic papillary carcinoma is a rare finding. PTC can involve the whole lobe of thyroid gland and infiltrate into periglandular fat, invade skeletal muscles, and adjacent organs (esophagus, larynx, and trachea). When carcinoma’s dimension is less than 1 cm in diameter, it is called “papillary microcarcinoma.” The World Health Organization (WHO) classification of thyroid tumors specifies 16 histological types of PTCs (including conventional variant). The histological division is based on the growth patterns, cytological features of tumor cells, and the type of tumor stroma. All papillary carcinomas present the typical nuclear features that are required for the diagnosis of PTC (see section on Cytology). Histological variants of PTC and their respective clinical behavior are listed in Table 3.2. Table 3.1 Bethesda System for Reporting Thyroid Cytopathology with Risk of Malignancy
Differentiated Thyroid Carcinomas
Epidemiology and Risk Factors
Pathology
Cytology
Histopathology
Papillary Thyroid Carcinoma
Diagnostic Categories of FNAB | Risk of Malignancy (%) |
Nondiagnostic or unsatisfactory specimen | 1–4 |
Benign Consistent with a benign follicular nodule Consistent with Hashimoto thyroiditis Consistent with granulomatous thyroiditis | 0–3 |
Atypia of undetermined significance or follicular lesion of undetermined significance | 5–15 |
Follicular neoplasm or suspicious for a follicular neoplasm | 15–30 |
Suspicious for malignancy Suspicious for papillary carcinoma Suspicious for medullary carcinoma Suspicious for metastatic carcinoma Suspicious for lymphoma | 60–75 |
Malignant Papillary thyroid carcinoma Poorly differentiated carcinoma Medullary thyroid carcinoma Undifferentiated (anaplastic) carcinoma Squamous cell carcinoma Carcinoma with mixed features Metastatic carcinoma Non-Hodgkin lymphoma | 97–99 |
FNAB, fine-needle aspiration biopsy.
A special variant of PTC that requires separate description because of its clinical importance is a papillary microcarcinoma. This term is reserved for incidentally found neoplasm measuring 10 mm in diameter or less. Typically, this type of PTC is characterized by relatively benign clinical course; however, in children it can behave more aggressively. Irrespective of the size of the tumor, up to 11% of the papillary microcarcinomas can be lymph-node positive. The features of papillary microcarcinoma suggestive of more aggressive behavior and implying prompt surgery are as follows:
• Tumors located near the trachea or on the dorsal surface of thyroid (these carcinomas will show dorsal extension and invade the adjacent organs).
• Features of high-grade tumor in cytological material (FNAB).
• Presence of regional lymph-node or distant metastasis, and
• Increase in the size of the tumor and/or appearance of node metastasis during observation.
Follicular Thyroid Carcinoma
By definition, it is a malignant epithelial tumor that shows a follicular differentiation (follicle formation) and a lack of characteristic nuclear features of papillary carcinoma (see section on Cytology). FTC accounts for 10 to 15% of the thyroid malignancies. FTC is more common in women and usually occurs later in life compared with PTC. It has much lower frequency of lymph-node metastasis compared with PTC (less than 5%), but distant metastasis (mainly to lung and bone) are more frequent at presentation (20 to 33%).6
Follicular carcinomas usually present as encapsulated solid tumors of larger than 1 cm diameter. The color varies from gray-tan to brown. The capsule can be noticed in some cases. Minimally invasive carcinomas are practically identical on gross examination with follicular adenomas.
Morphology of FTC is variable and includes tumors with follicles filled with colloid and neoplasms, which have solid and trabecular growth patterns. Diagnosis of malignant growth is based on the presence of vascular and/or capsular invasion. Architecture and cytological atypia are not essential for the diagnosis. Generally, FTC is divided into two main groups according to the extent of tumor invasiveness: minimally invasive (with limited infiltration of the tumor capsule or extension through the tumor capsule and/or vascular invasion) and widely invasive follicular carcinoma. The latter category includes carcinomas with distinct and wide infiltration of the thyroid tissue and/or blood vessels. “Capsular invasion” should be recognized with the penetration of tumor cells only through the capsule (not in the site of previous FNAB). “Vascular invasion” means the presence of intravascular tumor cells covered by endothelium or associated with thrombus; it refers to the vessels only within or beyond the capsule. Some authors also use the term “grossly encapsulated angioinvasive follicular carcinoma” to describe tumor in which both capsular invasion and vascular invasion are present (as opposed to minimally invasive carcinoma with only capsular invasion). Histological variants of FTC and their respective clinical behavior are presented in Table 3.2.
Survival rates for FTC vary from 70 to 95% and are little lower than for PTC. Prognostic factors that are related to unfavorable prognosis include age greater than 45 years, oncocytic variant of FTC, malignant infiltration beyond the thyroid, tumor size greater than 4 cm, and the presence of distant metastases.
Hürthle Cell Carcinoma
The WHO classification lists Hürthle cell carcinoma as a variant of FTC (“oncocytic variant of FTC”; see Table 3.2); however, it is frequently considered a separate pathologic entity characterized by distinct microscopic appearance and clinical behavior. Hürthle cell carcinoma or oncocytic variant of FTC comprises approximately 5% of the malignant thyroid tumors, and in contrast to FTC, the frequency of nodal metastases in this neoplasm is approximately 30%.
There is no evidence that pathogenesis of Hürthle cell carcinoma is different from that of conventional FTC, although H-Ras mutations are more often found in this type of tumor than in FTC.
Table 3.2 Histological Variants of PTC and FTC and Their Respective Prognosis
Type | Prognosis |
PTC subtypes | |
• Classical PTC (the most frequent; presents typical papillary architecture) | Good |
• Follicular PTC | Similar as in the classical type |
• Macrofollicular PTC | Similar to other follicular variants, with lymph-node metastases present in ~20% and distant metastases in 7% of the cases |
• Oncocytic cell | Not known |
• Clear cell | Not known |
• Diffuse sclerosing | Similar as in the classical type (despite high incidence of regional lymph-node and distant metastases) |
• Tall cell | Poor |
• Columnar cell | Poor |
• Solid | Poor |
• Cribriform | Not known (usually associated with FAP or Gardner syndrome) |
• With fascitis-like stroma | Similar as in the classical type |
• With focal insular component | Not known |
• With squamous cell or mucoepidermoid carcinoma | Poor |
• With spindle and giant cell carcinomas | Not known |
• Combined papillary and medullary carcinomas | Not known |
• Papillary microcarcinoma | Good (but in up to 11% cases, lymph-node metastasis can be present) |
FTC subtypes | |
• Encapsulated FTC with microscopic capsular invasion (no vascular invasion is present) = minimally invasive follicular carcinoma | Very low probability (less than 5% of the cases) of metastases, recurrences, or tumor-associated mortality |
• Encapsulated FTC with angioinvasion (capsular invasion is present or absent) | Metastases, recurrences, or tumor-associated mortality in 5–30% of the cases |
• Widely invasive follicular carcinoma | Metastases, recurrences, or tumor-associated mortality in 50–55% of the cases |
• Oncocytic cell (Hürthle cell) | Nodal metastases in ~30% of the cases |
• Clear cell | Not known |
• Mucinous variant | Not known |
• FTC with signet-ring cells | Not known |
PTC, papillary thyroid carcinoma; FAP, familial adenomatous polyposis; FTC, follicular thyroid carcinoma.
Macroscopically, Hürthle cell tumors have characteristic brown mahogany color (different from the color of other thyroid tumors) and are encapsulated. The morphological changes within the tumor, such as hemorrhage, cystic areas, infarction, fibrosis, and cellular atypia, can be associated, but not exclusively, with previous FNAB.
The tumor is built almost exclusively of oncocytic cells (at least 75% of all tumor cells). The growth pattern can be follicular or solid/trabecular. The Hürthle cells have deeply eosinophilic and granular cytoplasm; their nuclei are round and hyperchromatic with prominent nucleoli. Similar to FTC, the differentiation between Hürthle cell adenoma and carcinoma is based on the same criteria of capsular and/or vascular invasion. The malignant tumors are divided into minimally invasive and widely invasive variants.
Patients with Hürthle cell carcinoma are considered to have a poorer prognosis compared with patients with FTC and PTC. The frequency of lymph-node metastases as well as of distant metastases is higher than in non-Hürthle DTC. A lower uptake of radioactive iodine also makes the treatment of these tumors more challenging.
Patient Evaluation
Eliciting a detailed patient history is of immense importance. Besides the general history, the clinician should always ask the patient about important specific symptoms pertaining to thyroid disease. These include dysphagia, dyspnea, voice change (hoarseness), cough, sensation of a mass in the neck, change in weight, tremor, unusual sweating, mood changes, and palpitations. These help in establishing the diagnosis and in evaluating the extent of the disease process.
It is also important to ask about a family history of thyroid disorders and previous radiation exposure. As stated before, it is estimated that as many as 3 to 5% of all DTCs can occur in the familial settings. Patients with familial colon poliposis, those with Cowden disease, and those with Gardner syndrome also have a higher risk of developing a DTC.
Clinically apparent thyroid nodules can be found in approximately 4 to 7% of the adult population. It is important to bear in mind that of these nodules, malignancy will eventually be found in 5 to 12% of the patients with single nodules and in 3% of the patients with multiple nodules.
The clinical examination of a patient starts with visual inspection of the neck while it is slightly extended and the patient seated comfortably on an examination chair. During palpation it is customary to stand behind the patient. The examiner should place his or her hands on the patient’s neck so that the index fingers are just below the cricoid cartilage. Then, the examiner asks the patient to swallow so that the isthmus can be palpated. Examination is continued, with the examiner moving his or her fingers downward and laterally. The examiner should look for single nodules fixed to surrounding tissues with hard consistency. Palpable cervical lymph nodes can also be noted in some cases.
Finding the lower borders of the thyroid may at times be difficult because it can be partially or totally retrosternal; further extension of the neck may help.
Cervical spine flexibility should also be assessed to ensure hyperextension of the neck during surgery (only minimally invasive techniques do not require neck hyperextension to ensure adequate visualization; see below). Examination of larynx and vocal cords mobility should also be performed and documented, especially with more advanced tumors.
Algorithm for the Evaluation of a Thyroid Nodule
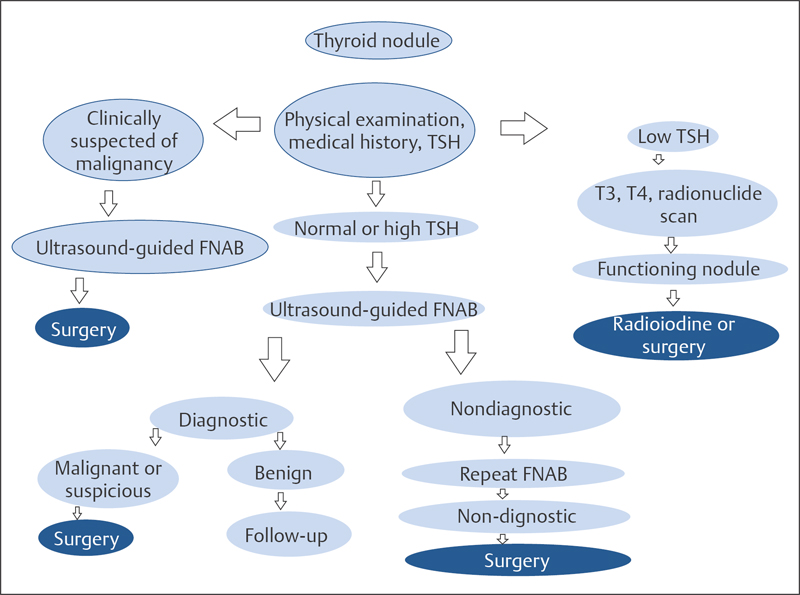
Because the autopsy series suggests that up to 50% of the general population can have thyroid nodules, it is of utmost importance to identify those lesions that are potentially harmful. Furthermore, a vast majority of thyroid nodules that are being seen and investigated by clinicians are incidental, asymptomatic findings. It is therefore crucial to not overdiagnose and overtreat otherwise healthy individuals who happen to have a completely benign thyroid nodule. The algorithm presented in Fig. 3.3 should help in correctly addressing these issues.
Laboratory Tests and Imaging Studies
The screening test for the evaluation of thyroid function is a must when evaluating any thyroid nodule. It is sufficient to start with the estimation of serum thyroid-stimulating hormone (TSH) level. In the case of subnormal TSH serum levels (i.e., < 0.5 mIU/L), one should proceed to T3 and T4 serum levels evaluation and a radionuclide scan should be obtained. The serum TSH level serves as a screening test for thyroid function. The evaluation of T3 and T4 can confirm the diagnosis of hyperthyroidism, and radionuclide scan will identify hyperfunctioning nodules. The evaluation of thyroid nodules with radionuclide scan (it has been estimated that 16% of the nonfunctioning nodules and 9% of the normal-functioning nodules on radionuclide scan are malignant, while hyperfunctioning nodules only occasionally harbor a malignancy) is no longer used as a first-line diagnostic tool in thyroid cancer.
Obtaining a thyroid ultrasound is an essential step for the exact characterization of the mass, and best results are achieved when it is performed by a dedicated neck ultrasonologist. The decision whether ultrasound-guided FNAB should follow is based on several factors, as shown in Fig. 3.3. If the decision on FNAB is taken, the laboratory tests for hemostatic function become mandatory.
Until recently, it was presumed that the size of thyroid nodule as seen on ultrasound should be a threshold for biopsy. This approach has changed, and currently the decision concerning the biopsy is based on features other than the tumor size. The ultrasonic features of a thyroid nodule that warrant an FNAB are calcification, irregularity (irregular halo), solid lesion, and hypervascularity.
The possible general categories of FNAB of a thyroid mass are as follows:
• Benign.
• Malignant (PTC, medullary thyroid carcinoma, anaplastic thyroid carcinoma).
• Indeterminant (follicular neoplasm; this can mean FTC and follicular adenoma). and
• Insufficient/nondiagnostic specimen (15 to 25% of all FNABs).
The FNAB result should be reported by using Bethesda System for Reporting Thyroid cytopathology (see Table 3.1). The diagnostic accuracy of FNAB is estimated at greater than 95%, and its false-negative rates are around –5%. FNAB is more accurate for lesions measuring 1 to 4 cm in diameter. Smaller lesions are difficult to sample accurately, while larger lesions have greater sampling error. As mentioned before, the FNAB is able to provide definitive diagnosis of PTC due to characteristic nuclear changes. It is unfortunately unable to distinguish between FTC and follicular adenoma, and therefore the diagnosis of FTC requires a histological proof of capsular invasion and/or vascular invasion. If the FNAB result suggests follicular neoplasm, thyroid lobectomy should be performed to permit full histological evaluation of the tumor. In approximately 20% of the lobectomy specimens in patients operated on because of FNAB suggesting follicular neoplasm, the final diagnosis confirms FTC. Undetermined or insufficient FNAB requires repetition of FNAB (see algorithm in Fig. 3.3).
Figure 3.3 Algorithm for the evaluation and diagnosis of a thyroid nodule. FNAB, fine-needle aspiration biopsy; TSH, thyroid-stimulating hormone.