and Mitrofanis Pavlidis2
(1)
Department of Ophthalmology, Uppsala University Hospital, Uppsala, Sweden
(2)
Augencentrum Köln, Cologne, Germany
14.2 Easy PDR
14.2.2 Complications
14.2.3 FAQ
14.3 Difficult PDR
14.3.1 General Introduction
14.3.3 Complications
14.3.4 FAQ
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-319-20236-5_14) contains supplementary material, which is available to authorized users.
Electronic supplementary material
for this chapter is accessible online at http://extras.springer.com/ by searching via the ISBN.
General Introduction
The surgical planning of the diabetic eye is very important; this is especially the case in active proliferative diabetic retinopathies. What is the right timing for a vitrectomy? Do not operate too early; if the eye is not pretreated with PRP or anti-VEGF injections and the diabetes is badly regulated, then the vitrectomy becomes very difficult. But do not operate too late either; if an active PDR progresses to a tractional detachment with macular involvement, then the vitrectomy will be difficult and visual prognosis poor.
The main rule is not to perform a vitrectomy in an untreated eye. Pretreat the eye first with PRP and anti-VEGF (Fig. 14.1), keep a tight follow-up until the retinopathy is inactive and then schedule surgery.
Fig. 14.1
Our treatment algorithm for surgical planning of a PDR
For surgery of diabetic eyes, we favour a stepwise procedure, i.e. we operate in several sessions depending on the severity of the PDR (see Table 14.1). Why a stepwise procedure? The difficulty of the vitrectomy depends on the severity of the PDR. A severe diabetic retinopathy requires a long traumatic surgery. The surgical trauma however aggravates the diabetic retinopathy, resulting in a vicious cycle.
The surgical planning is, however, also determined by local factors such as reimbursement of the surgery or the travel distance to the hospital. If the costs of the surgery are covered by the national health system and the patient lives close by, then the surgeon has much more freedom in surgical planning. If the patients pay the cost for surgery on his own and the travel distance is long, then the surgical planning is limited; the surgeon may be forced to perform the complete surgery in one session.
The grade of surgical difficulty depends on the severity of the diabetic retinopathy. The grades of difficulty are differentiated below:
Easy diabetic retinopathy
1.
Mild PDR: A complete PVD with vitreous haemorrhage is present. The retina is treated with scatter laser (Fig. 14.2).
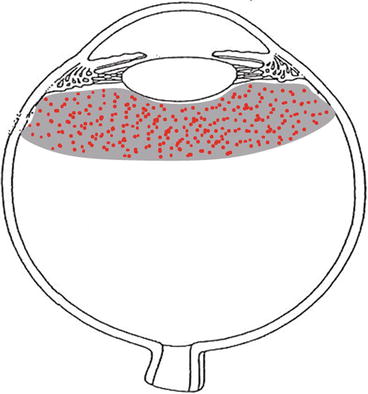
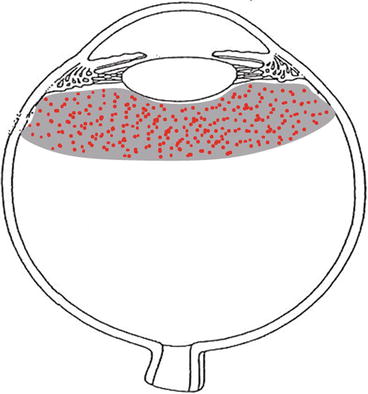
Fig. 14.2
A mild (surgically easy) PDR with vitreous haemorrhage. Note that a complete PVD is present. It is unlikely that fibrovascular membranes are present because the posterior hyaloid is detached
Difficult diabetic retinopathy
2.
Severe PDR: A partial PVD is present. Fibrovascular membranes are located at the posterior pole and the eye is scatter laser treated (Fig. 14.3).
Fig. 14.3
Illustration of a severe (surgically difficult) PDR. The retina is laser treated. Many retinal proliferations and vitreoretinal adhesions are present. The posterior hyaloid is attached in the posterior pole and partially detached in the periphery; the nasal posterior hyaloid is often attached
3.
Advanced PDR: A PVD is not present. No laser treatment has been performed. A tractional retinal detachment may be present (Fig. 14.4).
Fig. 14.4
A tractional retinal detachment (surgically very difficult). The retina is not laser treated. Many retinal proliferations and vitreoretinal adhesions are present. A tractional detachment is present. The posterior hyaloid is completely attached
The more active the retinopathy, the more stepwise we operate:
# In an easy PDR, we operate in one session if the nucleus is soft and in two sessions if the nucleus is hard, the latter, of course, in combination with an intravitreal anti-VEGF injection (Fig. 14.2).
Surgical trauma triggers the diabetic retinopathy and consequently the postoperative healing. It increases also the risk of recurrence of fibrovascular membranes. If you only operate on the cataract of an eye with active proliferative diabetic retinopathy, then the retinopathy will progress in the most cases and an iris rubeosis may occur. Therefore, combine a phacoemulsification always with an intravitreal anti-VEGF treatment in order to prevent a progression of the retinopathy and to quieten the retinopathy for the following vitrectomy.
We perform a stepwise procedure: First phacoemulsification combined with an anti-VEGF injection and 4 weeks later a vitrectomy. The vitrectomy is much easier, if the eye is pretreated with phacoemulsification and Avastin. The posterior hyaloid is easier to open, less intraoperatively bleeding will occur, the membranes are easier to remove and so forth. And the postoperative healing is of course faster.
A cautionary note regarding the timing of phaco and Avastin treatment: The effect of Avastin lasts 6 weeks. After 4–6 weeks, a laser treatment with/without vitrectomy should be scheduled. Alternatively, repeat an Avastin injection. Otherwise the PDR will reoccur after 3 months.
In the case of a lens-sparing vitrectomy (i.e. a young diabetes type I patient), we perform in a first step an intravitreal anti-VEGF injection. And 1–4 weeks later, we perform a lens-sparing vitrectomy.
Do not operate on an eye with advanced diabetic retinopathy that is not pretreated with anti-VEGF or PRP. If the retina is attached, then perform a PRP and inject anti-VEGF medication. If the retina is partially detached, then laser treat the attached retina. These advanced eyes are like a VEGF forest fire. A vitrectomy will add extra fuel to the fire. Extinguish the fire with PRP and anti-VEGF and perform a vitrectomy at a later time point when the PDR is inactive.
14.1 Combined Phacoemulsification and Anti-VEGF Treatment
Video 14.1: Phaco and Avastin (no audio)
A diabetic vitrectomy is easier if the eye is pretreated with anti-VEGF 1–4 weeks prior to the vitrectomy. If you have an opacified lens and the patient is older than 50 years, then perform also a cataract operation before the vitrectomy. It only takes 10 min of extra surgical time. Especially in advanced diabetic retinopathy cases, avoid anterior segment inflammation with iris rubeosis. A diabetic eye, which is pretreated with anti-VEGF and cataract surgery, is much easier to vitrectomize.
Perform a phacoemulsification as usual. Inject the IOL and place it into the capsular bag. Before removing the viscoelastics, perform an intravitreal injection with an anti-VEGF medication. Inject 0.1–0.2 ml. Then remove the viscoelastics and hydrate the incisions (Figs. 14.5 and 14.6).
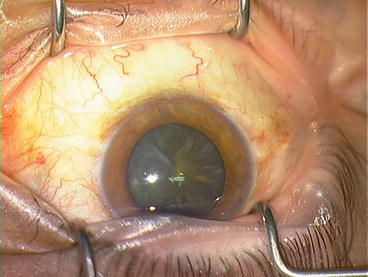
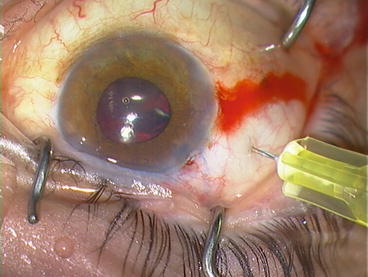
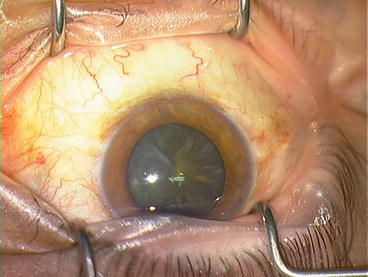
Fig. 14.5
A diabetic eye with vitreous haemorrhage. We apply a stepwise technique: First a combined phacoemulsification with intravitreal Avastin and 1 month later, if still necessary, a vitrectomy
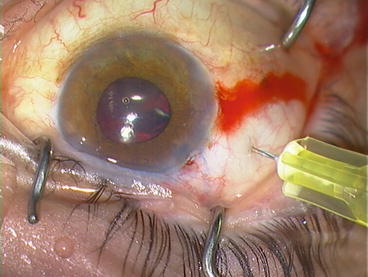
Fig. 14.6
After implantation of the IOL and before removal of the viscoelastics, an intravitreal injection of Avastin (0.1 ml) is performed
Surgical Pearls No. 50
If a patient has a bilateral PDR and you decide to vitrectomize one eye, then do not forget the other eye. Treat the other eye in the same session (or shortly after) with phaco + IOL + Avastin or at least only Avastin. It easily happens that the clinical focus lies on the vitrectomized eye and the other eye (often the better eye) gets worse.
14.2 Easy PDR
Video 14.2: 27G lens-sparing vitrectomy of a type I diabetic
A vitreous haemorrhage with attached retina and no associated major vitreoretinal pathology is suitable for the beginner. In most cases, a PVD is present and the haemorrhage fills out the vitreous gel behind the lens (Fig. 14.2). In the presence of vitreous haemorrhage, a previous history of panretinal photocoagulation usually facilitates the surgery, because it is associated with a higher rate of posterior vitreous detachment and promotes retinal adhesion to the RPE and choroid. He/she learns to work with the vitreous cutter and apply a PRP but does not need to perform any significant manipulations of the retina.
The main problem with this procedure is that there is no view of the fundus (Fig. 14.7). The procedure is even harder when the natural lens is still present, due to the risk of injuring the posterior capsule. In the learning phase, perform only PPVs in pseudophakic eyes.
Fig. 14.7
A dense vitreous haemorrhage with attached retina behind the vitreous
Practice the application of panretinal laser photocoagulation (PRP) very well using a chandelier light. In one hand, hold the scleral depressor and indent the sclera and retina, and in the other hand, hold the laser probe and apply a PRP up to the ora serrata (Fig. 14.8). This surgery can be performed under local anaesthesia. We use mostly 27G for these cases.
Fig. 14.8
Perform a PRP up to the ora serrata
Surgical Pearls No. 51
B-scan: In cases with vitreous haemorrhage, always perform a detailed preoperative ultrasound examination. Try to determine the state of the posterior vitreous face (attached, partially attached or detached) and the retina.
Instruments
1.
27G three-port trocar system with or without chandelier illumination
2.
120D lens
3.
Vitreous cutter
4.
Backflush instrument
5.
Scleral depressor
Tamponade
Air, SF6
Individual Steps
1.
Three-port trocar system with or without chandelier illumination
2.
Core vitrectomy
3.
Peripheral vitrectomy
4.
PRP
5.
Tamponade and intravitreal anti-VEGF treatment
6.
Removal of the trocar cannulas
14.2.1 The Surgery Step-by-Step: Figs. 14.7 and 14.8
1.
Three-port trocar system with or without chandelier illumination
2.
Core vitrectomy
The vitreous haemorrhage reduces the illumination of the light fibre, because the light cone is hidden by blood. Therefore, the surgeon should first make a core vitrectomy. Keep the vitreous cutter behind the IOL and remove all vitreous gel. It might be easier to work first without BIOM and use the microscope only as you would in cataract surgery. If the visibility is not improved, then try only to aspirate the liquefied blood. Try next to cut a break in the posterior hyaloid in order to obtain a view of the fundus (Fig. 14.7). It is important to identify the retinal vessels to make sure that the surgeon is in the right plane (and not in the subretinal space). If successful, continue the vitrectomy from the break into the posterior hyaloid.
Surgical Pearls No. 52
Blocked infusion: The haemorrhagic vitreous blocks sometimes the infusion. Check the infusion trocar before vitrectomy, and if in doubt, then cut the haemorrhagic vitreous around the infusion trocar.
Surgical Pearls No. 53
Removal of anterior hyaloid: In case of a haemorrhage directly behind the lens, it may be necessary to remove the anterior hyaloid. This is an easy procedure in pseudophakic patients but a lens-threatening procedure in phakic patients. We perform two techniques: Work at the edge of the lens (i.e. behind the zonules) in order to avoid a lens touch. (1) With help of a serrated jaws forceps, grab the anterior hyaloid/vitreous and pull it towards the centre of the globe. Work from both sides. (2) With help of a vitreous cutter, suck the anterior hyaloid/vitreous (only aspiration) and pull the vitreous cutter towards the centre of the globe. Cut the vitreous there. Work from both sides.
3.
Peripheral vitrectomy
Proceed to trim the vitreous base. Do not trim the vitreous base completely because the risk of causing damage to the retina is higher than the benefits. If the posterior vitreous body is not detached, then a PVD should be performed now. If the aetiology of the bleeding is, for example, a bleeding vessel, treat it now with laser, diathermy or cryo.
Surgical Pearls No. 54
How should epiretinal blood be removed? (1) Aspirate epiretinal blood by sweeping with a silicone tip flute needle over the retina. (2) By pressing several times on the side opening/tubing of the backflush instrument, water is ejected from the tip of the flute needle and blows the epiretinal blood upwards. The blood can then be easily aspirated at the same time with the vitreous cutter. (3) Clotted blood can be grasped with an ILM forceps and be removed with the vitreous cutter.
4.
Panretinal photocoagulation (PRP)
We recommend completing a PRP intraoperatively in all cases of vitrectomy for proliferative diabetic retinopathy. This is the best opportunity to complete the PRP, as rebleeding into the vitreous cavity is a common problem following vitrectomy, which will have a negative influence on performing additional PRP after the vitrectomy. Use the scleral depressor and apply a dense PRP up to the ora serrata (Fig. 14.8). For PRP we recommend the following laser parameters: power, 100–150 mw; duration, 200 ms; and interval, 200–300 ms at an OcularLight GL Company Iridex. These values are dependent on the device and the pigmentation of the fundus.
After endolaser photocoagulation, check if a new haemorrhage occurred at the central pole, and treat it before you move on to the tamponade.
Surgical Pearls No. 55
Small pupil: If the pupil constricts during surgery, inject 0.01 % Adrenalin into the anterior chamber. The pupil should enlarge within seconds. If the small pupil is caused by posterior synechiae, use stretching instruments such as a push–pull or insert iris hooks to enlarge the pupil.
5.
Tamponade and intravitreal anti-VEGF treatment
An air or gas tamponade is recommended to avoid a rebleeding into the vitreous cavity. Inject 0.2 ml bevacizumab at the end of the procedure to inhibit proliferative vessels.
6.
Removal of trocar cannulas
The trocars are removed, as described above. In cases of a 25G trocar and silicone oil tamponade, suture the sclerotomy.
Postoperative Tamponade and Posture
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


