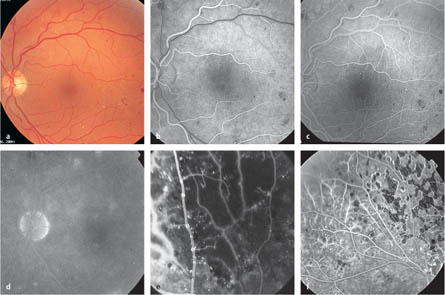
6.1 Nonproliferative Diabetic Retinopathy – Mild NPDR: microaneurysms – Moderate NPDR: additional retinal hemorrhage, cotton-wool spots – Severe NPDR: additional larger hemorrhages in four quadrants, venous beading in two quadrants, or distinct intraretinal microvascular anomalies (IRMAs) Bornfeld N, Joussen AM, Helbig H, et al. Augenerkrankungen. In: Mehnert H, Standl E, Usadel KH, editors. Diabetologie in Klinik und Praxis, 5th ed. Stuttgart: Thieme, 2003: 523–49. Cunha-Vaz J, Bernardes R. Nonproliferative retinopathy in diabetes type 2: initial stages and characterization of phenotypes. Prog Retin Eye Res 2005;24:355–77. Flynn HW, Smiddy WE. Diabetes and ocular disease: past, present, and future therapies. San Francisco: Foundation of the American Academy of Ophthalmology, 2000 (Ophthalmology Monographs, 14). Hamilton AMP, Ulbig MW, Polkinghorne P. Management of diabetic retinopathy. London: British Medical Journal Publishing Group, 1996. Wilkinson CP, Ferris FL 3rd, Klein RE, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003:110:1677–82. Fig. 6.1a–f Nonproliferative diabetic retinopathy a Color photograph. Moderate nonproliferative diabetic retinopathy with small retinal hemorrhages, microaneurysms, and hard exudates. b Early arteriovenous phase. Blockage of the background fluorescence caused by retinal hemorrhages. c Arteriovenous phase. Dot-like hyperfluorescence of the micro-aneurysms. d Late phase. Areas of mild hyperfluorescence in a region with permeable capillaries and microaneurysms, reflecting localized retinal edema. e Arteriovenous phase (in a different patient). Severe nonproliferative diabetic retinopathy with extensive areas of capillary occlusion and venous beading. f Arteriovenous phase (in a different patient). The effect of laser coagulation on an ischemic retina. Retinal areas with capillary occlusion and ill-defined staining of the vessels, reflecting increased vessel wall permeability, can be seen on the left of the image. An area with laser scars can be seen on the right; in this area, only the vessel lumina stain, with no dye leakage. – Focal diabetic macular edema – Diffuse diabetic macular edema – Ischemic diabetic maculopathy – Mixed forms
Epidemiology, Pathophysiology, and Clinical Presentation
 Diabetic retinopathy occurs in 98% of patients with type 1 diabetes after 15 years of diabetes, in approximately 55% of those with type 2 diabetes not receiving insulin treatment, and in approximately 85% of those with type 2 diabetes receiving insulin treatment.
Diabetic retinopathy occurs in 98% of patients with type 1 diabetes after 15 years of diabetes, in approximately 55% of those with type 2 diabetes not receiving insulin treatment, and in approximately 85% of those with type 2 diabetes receiving insulin treatment.
 The basic pathophysiological alterations relate to increased permeability as well as occlusion of the retinal capillaries, leading to the development of retinal edema and reduced perfusion and ischemia of the retina, resulting in deterioration of retinal function.
The basic pathophysiological alterations relate to increased permeability as well as occlusion of the retinal capillaries, leading to the development of retinal edema and reduced perfusion and ischemia of the retina, resulting in deterioration of retinal function.
 Nonproliferative diabetic retinopathy (NPDR) is classified according to its severity:
Nonproliferative diabetic retinopathy (NPDR) is classified according to its severity:
Fluorescein Angiography
 Microaneurysms appear as dot-like areas of hyper-fluorescence, or may appear hypofluorescent if they have thrombosed.
Microaneurysms appear as dot-like areas of hyper-fluorescence, or may appear hypofluorescent if they have thrombosed.
 Retinal hemorrhages and hard exudates block the choroid fluorescence.
Retinal hemorrhages and hard exudates block the choroid fluorescence.
 In the majority of cases, capillary occlusions can only be identified angiographically. Vessels adjacent to nonperfused areas often show increased permeability.
In the majority of cases, capillary occlusions can only be identified angiographically. Vessels adjacent to nonperfused areas often show increased permeability.
 Increased permeability of retinal capillaries is angio-graphically characterized as ill-defined hyperfluorescence in the vessel wall. In late images, the adjacent edematous retinal tissue is diffusely stained.
Increased permeability of retinal capillaries is angio-graphically characterized as ill-defined hyperfluorescence in the vessel wall. In late images, the adjacent edematous retinal tissue is diffusely stained.
 Cotton-wool spots represent swollen nerve fibers in the area of micro-infarctions of the inner retina, and have a hypofluorescent appearance due to blockage of the choroidal fluorescence by the opaque nerve fibers and due to the underlying retinal capillary occlusion.
Cotton-wool spots represent swollen nerve fibers in the area of micro-infarctions of the inner retina, and have a hypofluorescent appearance due to blockage of the choroidal fluorescence by the opaque nerve fibers and due to the underlying retinal capillary occlusion.
 Intraretinal microvascular abnormalities are dilated and tortuous preexisting capillaries, or may be newly formed intraretinal vessels. As with localized areas of venous beading, they typically occur next to areas of capillary occlusion.
Intraretinal microvascular abnormalities are dilated and tortuous preexisting capillaries, or may be newly formed intraretinal vessels. As with localized areas of venous beading, they typically occur next to areas of capillary occlusion.
Diagnosis and Treatment
 The diagnosis is established by clinical examination with binocular ophthalmoscopy. Angiography is not obligatory.
The diagnosis is established by clinical examination with binocular ophthalmoscopy. Angiography is not obligatory.
 Optimization of blood pressure and the blood glucose level delays the development of diabetic retinopathy and progression to proliferative retinopathy in both type 1 and type 2 diabetes.
Optimization of blood pressure and the blood glucose level delays the development of diabetic retinopathy and progression to proliferative retinopathy in both type 1 and type 2 diabetes.
 Mild scatter laser coagulation can be considered in severe nonproliferative diabetic retinopathy (NPDR), particularly when there is proliferative retinopathy in the fellow eye or if poor compliance with check-up examinations is expected.
Mild scatter laser coagulation can be considered in severe nonproliferative diabetic retinopathy (NPDR), particularly when there is proliferative retinopathy in the fellow eye or if poor compliance with check-up examinations is expected.
References
6.2 Diabetic Macular Edema
Epidemiology, Pathophysiology, and Clinical Presentation
 Macular edema is responsible for the majority of visual loss in diabetic retinopathy, particularly in patients with type 2 diabetes. Functional loss develops as a result of swelling of the central retina.
Macular edema is responsible for the majority of visual loss in diabetic retinopathy, particularly in patients with type 2 diabetes. Functional loss develops as a result of swelling of the central retina.
 Diabetic macular edemas are clinically divided into the following subgroups:
Diabetic macular edemas are clinically divided into the following subgroups:
Fluorescein Angiography
 Macular edema occurs as a result of leakage of fluid from hyperpermeable capillary walls into the adjacent macular tissue. These capillaries are also permeable to fluorescein, which during angiography initially stains the vessel walls and then in the late phase stains the swollen retinal tissue.
Macular edema occurs as a result of leakage of fluid from hyperpermeable capillary walls into the adjacent macular tissue. These capillaries are also permeable to fluorescein, which during angiography initially stains the vessel walls and then in the late phase stains the swollen retinal tissue.
 The perifoveal capillary arcades show rarefaction and ectatic changes in the retinal capillaries, as a sign of incipient central ischemia. Laser coagulation is not advisable in cases of marked central ischemia. Angiography is recommended before laser coagulation of diffuse macular edema.
The perifoveal capillary arcades show rarefaction and ectatic changes in the retinal capillaries, as a sign of incipient central ischemia. Laser coagulation is not advisable in cases of marked central ischemia. Angiography is recommended before laser coagulation of diffuse macular edema.
 Angiographically, diffuse macular edema often shows cystoid components.
Angiographically, diffuse macular edema often shows cystoid components.
Diagnosis and Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree