Purpose
To describe the distribution and determinants of lens vault and to investigate the association of lens vault with narrow angles.
Design
Prospective cross-sectional study.
Methods
Phakic subjects 50 years and older were evaluated at a primary healthcare clinic with gonioscopy, partial laser interferometry, and anterior segment optical coherence tomography (AS-OCT). Narrow angles were defined as posterior trabecular meshwork not visible for ≥2 quadrants on non-indentation gonioscopy. Lens vault was defined as the perpendicular distance between the anterior pole of the crystalline lens and the horizontal line joining the 2 scleral spurs on horizontal AS-OCT scans. Analysis of covariance, multivariate logistic regression, and area under the receiver operating characteristic curves (AUC) were performed.
Results
Of the 2047 subjects recruited, 582 were excluded because of poor image quality or inability to locate scleral spurs, leaving 1465 subjects for analysis. Eyes with narrow angles had greater lens vault compared to eyes with open angles (775.6 µm vs 386.5 µm, P < .0001). Women had significantly greater lens vault than men (497.28 µm vs 438.56 µm, P < .001), and lens vault increased significantly with age ( P for trend <.001). Adjusted for age and sex, significant associations with greater lens vault were shorter axial length, shallower anterior chamber depth(ACD), higher intraocular pressure, and more hyperopic spherical equivalent (all P < .001). On multivariate analysis, subjects with lens vault >667.6 µm were more likely to have narrow angles (OR 2.201, 95% CI: 1.070-4.526) compared to those with lens vault ≤462.7 µm. The AUC for lens vault (0.816) and ACD (0.822) for detecting narrow angles were similar ( P = .582).
Conclusions
Lens vault was independently associated with narrow angles and may be useful in screening to detect eyes with narrow angles.
Primary angle-closure glaucoma (PACG) is a major cause of irreversible visual impairment in Asia. Identification of ocular factors associated with angle closure may be useful for screening for the disease and eventual prevention of PACG, as interventions such as laser iridotomy may halt the angle-closure process and prevent the development of glaucomatous optic neuropathy. Known predisposing anatomical features for PACG include shallow anterior chamber depth (ACD), thick anteriorly positioned lens, steeply curved corneas, and short axial length (AXL).
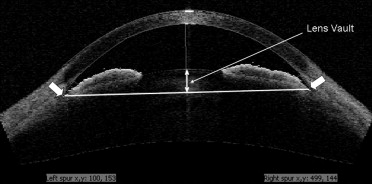
Anterior segment optical coherence tomography (AS-OCT) is a noncontact, easily performed examination that allows high-resolution cross-sectional imaging of the entire anterior chamber in a single image. It enables the quantitative evaluation of morphologic features of the anterior chamber such as lens vault, defined as the perpendicular distance between the anterior pole of the lens and a horizontal line joining the 2 scleral spurs ( Figure ). A recent study on angle-closure patients recruited from a glaucoma clinic showed that lens vault is an ocular parameter independently associated with angle closure, and one that may capture the role of the lens in this disorder better than other lens parameters.
The aim of this study was to evaluate the distribution and determinants of lens vault in a large sample of subjects recruited from a polyclinic located in the community, and to investigate the association of lens vault with narrow angles.
Methods
Study Population
This was a cross-sectional study of persons aged 50 years and older who were recruited between December 7, 2005 and July 12, 2006 from a government-run polyclinic in Singapore that provides primary healthcare services for residents living in the area around the clinic. Details of the study have been described previously. In brief, subjects were identified by systematic sampling (every fifth patient registered at the polyclinic) and asked to participate in the study after obtaining written informed consent. Subjects did not specifically have ophthalmic complaints at the time of consultation. A detailed questionnaire, including socioeconomic and education details, as well as medical and ocular history, was administered. Individuals with a history of glaucoma, previous intraocular surgery, previous laser treatment, penetrating eye injury, or corneal disorders preventing anterior chamber assessment were excluded.
Ocular Examination
All participants underwent a standardized eye examination that included visual acuity measurement using a logarithm of minimal angle of resolution chart (logMAR chart; Lighthouse Inc, Long Island, New York, USA), autorefraction (Topcon RM-8000B; Topcon Corporation, Tokyo, Japan), slit-lamp examination (Model BQ 900; Haag-Streit, Bern, Switzerland), stereoscopic optic disc examination with a 78-diopter lens (Volk Optical Inc, Mentor, Ohio, USA), and intraocular pressure (IOP) measurement using Goldmann applanation tonometry (Haag-Streit AG, Koniz, Switzerland). AXL and central ACD were also measured by IOLMaster (Carl Zeiss, Jena, Germany).
Gonioscopy was performed at a low level of ambient illumination using a Goldmann 2-mirror lens (Haag-Streit AG) at high magnification (×16) with the eye in the primary position of gaze. Indentation gonioscopy with the Sussman 4-mirror lens (Ocular Instruments Inc, Bellevue, Washington, USA) was used to establish the presence or absence of peripheral anterior synechiae (PAS). An eye was considered to have narrow angles if the posterior trabecular meshwork was not visible for at least 180 degrees on non-indentation gonioscopy with the eye in the primary position using the Goldmann lens. Gonioscopy was performed by a single ophthalmologist (R.L.) with extensive experience in performing gonioscopy in epidemiologic studies, who was standardized against another ophthalmologist with subspecialty glaucoma training (T.A.).
Anterior Segment Optical Coherence Tomography Imaging
AS-OCT (Visante, Carl Zeiss Meditec, Dublin, California, USA) imaging was performed on all subjects under standardized dark conditions (20 lux) by an experienced operator who was masked to the results of the clinical ophthalmic examination. Scans were centered on the pupil and taken along the horizontal axis (nasal-temporal angles at 0 to 180 degrees), using the standard anterior segment single-scan protocol. To obtain the best-quality image, the examiner adjusted the saturation and noise and optimized the polarization for each scan during the examination. As several scans are acquired by the AS-OCT device, the examiner chose the best image, with the least image artefacts attributable to eye motion or the eyelids. One cross-sectional scan imaging the nasal and temporal angle of the right eyes was evaluated for each subject. The entire acquisition process on both eyes of each patient, on average, took less than 5 minutes per patient.
Images were then processed using customized software, the Zhongshan Angle Assessment Program (ZAAP; Zhongshan Ophthalmic Centre, Guangzhou, China). The AS-OCT images were assessed by a single fellowship-trained glaucoma specialist (L.M.S.) masked to clinical data. The only observer input was to determine the location of the 2 scleral spurs. The ZAAP algorithm then automatically calculated the lens vault ( Figure ). To calculate lens vault, the software draws a line between the 2 scleral spurs and then a perpendicular line is extended from this line to the anterior border of the lens at the point of greatest convexity. Lens vault was defined as the perpendicular distance between the anterior pole of the crystalline lens and the horizontal line joining the 2 scleral spurs, on horizontal AS-OCT scans. The intraobserver reproducibility of the anterior chamber measurements were assessed using a random subset of 101 eyes by a single examiner (L.M.S.), masked to the initial test results. To do this, measurements were performed in 2 sessions separated by an interval of 1 week. Anterior chamber width (ACW), defined as the distance between the scleral spurs in the horizontal (nasal-temporal) axis of AS-OCT scans, was obtained using the same software as previously described.
Statistical Analysis
Data from right eyes were used for analysis. Statistical analyses were performed with SPSS (version 18; SPSS Inc, Chicago, Illinois, USA). Analysis of covariance (ANCOVA) models were used to estimate mean lens vault, adjusted for age and sex. The association between lens vault and the presence of narrow angles on gonioscopy was initially assessed using logistic regression models to determine the odds ratio (OR) and its 95% confidence interval (CI), adjusting for age and sex. Multivariate adjusted OR was obtained after adjustment for age, sex, AXL, and ACD. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of these ocular parameters for identifying narrow angles were also calculated. Receiver operator characteristic (ROC) curve was generated and the area under the ROC curve (AUC) was used to assess the performance of these ocular parameters in detecting narrow angles. A P value less than .05 was considered statistically significant.
Results
A total of 2047 participants were recruited into the study. Among them, 582 subjects were excluded for the following reasons: 11 subjects could not undergo gonioscopy; 62 subjects did not complete AS-OCT examination or had poor quality AS-OCT images; 42 subjects showed software delineation errors; and the scleral spur was not clearly visible on AS-OCT images in 467 subjects. There were no significant differences between included and excluded subjects regarding race, spherical equivalent refraction, IOP, or AXL, but included subjects were younger ( P < .001), had shallower ACD ( P = .02) and narrower mean angle grade ( P = .004), and were more often female ( P = .03). Therefore, data from 1465 participants (71.6%) were available and included in the analysis. Of these, 793 (54.1%) were female and 1319 (90.0%) were Chinese. The mean age (± standard deviation [SD]) was 62.7 ± 7.7 years.
The intraobserver reproducibility of lens vault measurement was excellent, with intraclass correlation coefficient of 0.973 (95% CI, 0.961−0.982). In the random subset of 101 eyes that were reassessed, overall mean lens vault was 767.03 μm with a within-subject standard deviation of 31.33 μm and a within-subject coefficient of variation of 4.1%. Repeatability coefficient was 61.40 μm.
Of the 1465 subjects, 315 (21.5%) were diagnosed as having narrow angles on gonioscopy. Analysis of ocular data was performed for all 1465 right eyes of these subjects. Eyes with narrow angles showed significantly shorter AXL (23.09 ± 0.88 mm vs 24.13 ± 1.36 mm, P < .0001) and shallower ACD (2.202 ± 0.202 mm vs 2.730 ± 0.294 mm, P < .0001) compared with eyes with open angles.
The overall population mean lens vault was 469.97 ± 288.37 μm. Eyes with narrow angles had markedly higher lens vault values when compared to eyes with open angles (775.6 μm vs 386.8 μm, P < .0001) ( Table 1 ). Women had a significantly greater lens vault then men (497.28 μm vs 438.56 μm, P < .001), and this association remained after adjusting for age. Lens vault increased with greater age ( P for trend <.001) for all persons, as well as when analyzed separately for men and women. However, in female subjects with narrow angles, there was no significant change in lens vault found with increasing age ( Table 1 ).
| All Persons | Persons With Narrow Angles | Persons Without Narrow Angles | ||||
|---|---|---|---|---|---|---|
| Age (years) | N | Mean LV (SD), μm | N | Mean LV (SD), μm | N | Mean LV (SD), μm |
| All persons | ||||||
| All ages | 1464 | 469.97 (288.37) | 315 | 775.59 (190.35) | 1149 | 386.77 (251.75) |
| 50−59 | 612 | 434.78 (268.68) | 89 | 725.85 (162.31) | 523 | 329.93 (244.31) |
| 60−69 | 561 | 493.91 (284.94) | 138 | 781.07 (197.40) | 423 | 400.26 (243.58) |
| ≥70 | 291 | 599.04 (271.51) | 88 | 817.29 (196.02) | 203 | 504.44 (244.01) |
| P for trend | <.001 | .005 | <.001 | |||
| Male | ||||||
| All ages | 672 | 438.56 (295.27) | 112 | 785.47 (224.28) | 560 | 369.18 (256.39) |
| 50−59 | 245 | 329.57 (257.83) | 23 | 659.55 (173.26) | 222 | 295.39 (240.63) |
| 60−69 | 264 | 454.81 (292.00) | 49 | 780.05 (229.34) | 215 | 380.68 (251.49) |
| ≥70 | 163 | 576.08 (291.83) | 40 | 864.51 (213.78) | 123 | 482.28 (249.66) |
| P for trend | <.001 | <.001 | <.001 | |||
| Female | ||||||
| All ages | 792 | 497.28 (279.56) | 203 | 770.14 (169.11) | 589 | 403.24 (246.47) |
| 50−59 | 367 | 426.18 (275.63) | 66 | 748.95 (153.00) | 301 | 355.40 (244.27) |
| 60−69 | 297 | 528.67 (274.37) | 89 | 781.64 (178.81) | 208 | 420.43 (234.01) |
| ≥70 | 128 | 628.29 (241.17) | 48 | 777.94 (172.41) | 80 | 538.51 (232.48) |
| P for trend | <.001 | .463 | <.001 | |||
After controlling for age and sex, greater lens vault in all persons was associated with shorter AXL ( P < .001), shallower central ACD ( P < .001), higher IOP ( P = .014), more hyperopic spherical equivalent ( P < .001), and lower education ( P < .001) ( Table 2 ). However, education and refraction had no relationship with lens vault when analyzing only those with narrow angles. For IOP, stratified analysis found no relationship with lens vault when analysis was performed separately in those with and without narrow angles. Greater anterior chamber width was associated with higher lens vault only in those with narrow angles ( P = .008). There was no association found in those with no narrow angles or in the overall population.
| All Persons | Persons With Narrow Angle | Persons Without Narrow Angle | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | N | Mean LV (SD), μm | P Value | N | Mean LV (SD), μm | P Value | N | Mean LV (SD), μm | P Value |
| Race | .731 | .755 | .208 | ||||||
| Chinese | 1317 | 471.69 (290.23) | 303 | 774.98 (188.41) | 1014 | 381.06 (251.21) | |||
| Malay | 27 | 479.79 (308.42) | 5 | 809.84 (336.24) | 22 | 404.78 (253.79) | |||
| Indian | 102 | 444.21 (266.67) | 5 | 734.94 (131.01) | 97 | 429.22 (263.57) | |||
| Other | 18 | 504.41 (239.67) | 2 | 883.25 (313.60) | 16 | 457.05 (192.39) | |||
| Education | .001 | .678 | .001 | ||||||
| No formal education | 264 | 561.90 (278.05) | 82 | 792.46 (199.71) | 182 | 458.02 (244.03) | |||
| Primary | 401 | 500.91 (284.95) | 93 | 790.94 (214.98) | 308 | 413.34 (242.42) | |||
| Secondary/technical | 504 | 442.40 (273.11) | 86 | 765.39 (160.16) | 418 | 375.95 (242.49) | |||
| A level/polytechnic | 164 | 418.86 (289.33) | 31 | 751.51 (173.79) | 133 | 341.33 (253.89) | |||
| Tertiary | 131 | 364.02 (312.62) | 23 | 723.92 (175.03) | 108 | 287.38 (280.48) | |||
| BMI, kg/m 2 | .883 | .111 | .660 | ||||||
| First quartile (≤21.45) | 361 | 480.26 (291.47) | 97 | 754.91 (192.32) | 264 | 379.35 (254.44) | |||
| Second quartile (>21.45, ≤23.63) | 370 | 470.99 (275.98) | 83 | 749.97 (192.77) | 287 | 390.31 (241.86) | |||
| Third quartile (>23.63, ≤26.07) | 366 | 469.97 (297.66) | 70 | 812.92 (171.39) | 296 | 388.87 (261.24) | |||
| Fourth quartile (>26.07) | 366 | 459.35 (288.46) | 65 | 798.96 (198.55) | 301 | 386.02 (249.88) | |||
| Axial length, mm | <.001 | .002 | <.001 | ||||||
| First quartile (≤23.01) | 356 | 656.99 (228.53) | 150 | 804.1 (170.81) | 206 | 549.86 (204.61) | |||
| Second quartile (>23.01, ≤23.67) | 358 | 541.94 (254.70) | 88 | 783.73 (193.87) | 270 | 463.13 (220.4) | |||
| Third quartile (>23.67, ≤24.59) | 358 | 424.56 (255.98) | 51 | 709.7 (214.76) | 307 | 377.19 (230.45) | |||
| Fourth quartile (>24.59) | 362 | 265.17 (254.42) | 18 | 727.72 (154.89) | 344 | 240.97 (234.78) | |||
| Central ACD, mm | <.001 | <.001 | <.001 | ||||||
| First quartile (≤2.81) | 375 | 763.41 (196.49) | 225 | 828.92 (173.2) | 150 | 665.14 (188.7) | |||
| Second quartile (>2.81, ≤3.07) | 367 | 562.10 (179.70) | 80 | 652.72 (155.33) | 287 | 536.84 (178.1) | |||
| Third quartile (>3.07, ≤3.34) | 356 | 374.76 (176.21) | 10 | 558.48 (219.16) | 346 | 369.45 (172.31) | |||
| Fourth quartile (>3.34) | 365 | 170.88 (188.56) | 0 | 365 | 170.88 (188.56) | ||||
| Intraocular pressure, mm Hg | .014 | .794 | .637 | ||||||
| First quartile (≤13) | 366 | 437.03 (282.94) | 56 | 778.97 (197.17) | 310 | 375.26 (250.25) | |||
| Second quartile (>13, ≤14) | 383 | 453.97 (294.82) | 74 | 764.81 (201.18) | 309 | 379.52 (263.51) | |||
| Third quartile (>14, ≤16) | 483 | 488.74 (273.30) | 111 | 768.2 (199.98) | 372 | 405.36 (234.2) | |||
| Fourth quartile (>16) | 228 | 512.66 (310.57) | 73 | 795.26 (159.91) | 155 | 379.57 (273) | |||
| Anterior chamber width | .086 | .008 | .619 | ||||||
| First quartile (≤11.50) | 377 | 514.80 (279.40) | 130 | 753.61 (189.03) | 247 | 389.11 (233.62) | |||
| Second quartile (>11.50, ≤11.75) | 359 | 470.87 (277.38) | 83 | 765.2 (168.09) | 276 | 382.36 (240.26) | |||
| Third quartile (>11.75, ≤12) | 362 | 460.57 (299.39) | 71 | 782.93 (175.5) | 291 | 381.92 (269.25) | |||
| Fourth quartile (>12) | 366 | 433.62 (291.66) | 31 | 878.73 (250.96) | 335 | 392.43 (259.25) | |||
| Autorefraction spherical equivalent, diopters | <.001 | .597 | <.001 | ||||||
| First quartile (≤−0.44) | 343 | 313.79 (290.27) | 22 | 828.65 (238.05) | 321 | 278.5 (258.56) | |||
| Second quartile (>−0.44, ≤1.25) | 357 | 469.33 (262.38) | 66 | 757.28 (182.99) | 291 | 404.03 (232.07) | |||
| Third quartile (>1.25, ≤2.31) | 333 | 508.82 (265.60) | 84 | 764.07 (193.87) | 249 | 422.72 (228.8) | |||
| Fourth quartile (>2.31) | 339 | 593.45 (259.63) | 123 | 781.17 (177.63) | 216 | 486.56 (237.56) | |||
| Mean keratometry, mm | .176 | .488 | .077 | ||||||
| First quartile (≤7.4) | 563 | 492.90 (283.81) | 122 | 791.25 (187.54) | 441 | 410.36 (248.39) | |||
| Second quartile (>7.4, ≤7.5) | 190 | 439.49 (296.26) | 38 | 798.61 (171.98) | 152 | 349.7 (249.08) | |||
| Third quartile (>7.5, ≤7.7) | 416 | 463.97 (289.78) | 91 | 762.37 (206.59) | 325 | 380.41 (252.37) | |||
| Fourth quartile (>7.7) | 294 | 456.63 (287.99) | 64 | 750.85 (181.72) | 230 | 374.76 (257.11) | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


