Purpose
To assess through-focus polychromatic image sharpness of 5 FDA-approved presbyopia-correcting intraocular lenses (IOLs) through a range of object vergences and pupil diameters using an image sharpness algorithm.
Design
Laboratory investigation.
Methods
A 1951 USAF resolution target was imaged through Crystalens AO (AO), Crystalens HD (HD), aspheric ReSTOR +4 (R4), aspheric ReSTOR +3 (R3), and Tecnis Multifocal Acrylic (TMF) IOL in a model eye and captured digitally for each combination of pupil diameter and object vergence. The sharpness of each digital image was objectively scored using a 2-dimensional gradient function.
Results
AO had the best distance image sharpness for all pupil diameters and was superior to the HD. With a 5-mm pupil, the R4 distance image sharpness was similar to the HD and at 6 mm the TMF was superior to the HD, R3, and R4. The R3 moved the near focal point farther from the patient compared to the R4, but did not improve image sharpness at intermediate distances and showed worse distance and near image sharpness. Consistent with apodization, the ReSTOR IOLs displayed better distance and poorer near image sharpness as pupil diameter increased. TMF showed consistent distance and near image sharpness across pupil diameters and the best near image sharpness for all pupil diameters.
Conclusions
Differing IOL design strategies to increase depth of field are associated with quantifiable differences in image sharpness at varying vergences and pupil sizes. Objective comparison of the imaging properties of specific presbyopia-correcting IOLs in relation to patient’s pupil sizes can be useful in selecting the most appropriate IOL for each patient.
Presbyopia and cataract represent the 2 most common human ocular afflictions. In the past, cataract extraction with monofocal intraocular lens (IOL) implantation addressed the loss of acuity and contrast attributable to forward light scatter associated with cataract, but did not remedy the effects of the age-associated loss of accommodation on limiting the range of functional vision and increasing spectacle dependence. With monofocal IOLs, a functional restoration of near vision was limited to those patients choosing pseudophakic monovision or those patients (roughly 3%-8% in most studies ) fortunate enough to have adequate pseudoaccommodation to readily perform near tasks (such as reading a newspaper without glasses) with both eyes targeted to emmetropia.
More recently, different approaches to IOL design have evolved in an effort to address the impact of presbyopia, and new strategies and technologies will continue to appear. Multifocal IOLs are designed with refractive and/or diffractive optical properties, which focus light at multiple foci and allow the patient to see both near and distant objects. Since the light energy is distributed between more than 1 image and some energy is lost to useless foci, each primary image produced by a multifocal IOL is thereby fainter and defocused at any given pupil diameter compared to monofocal, toric, or accommodating IOLs that do not split light in this manner. In contrast to fully diffractive multifocal IOLs, where the step height of each concentric ring is uniform, apodized diffractive-refractive IOLs take advantage of progressively smaller step heights to shift the energy distribution toward the distance focus with larger pupil diameters.
Accommodating IOLs are designed to change the refractive state of the eye, by either translating the optic axially or inducing higher-order aberrations (Neal DR, et al. IOVS 2010; 51: ARVO E-Abstract 812) to improve through-focus via the movement of the ciliary muscle and changes in vitreous pressure. Unlike multifocal IOLs, accommodating IOLs have a single point of focus. The increase in effective dioptric power with current single-optic accommodating IOLs may be limited and the clinically observed enhanced near vision may be the result of dynamic changes in spherical aberration and other higher-order aberrations resulting from accommodative effort (Neal DR, et al. IOVS, 2010;51: ARVO E-Abstract 812). The current study does not address the effects of accommodation on through-focus pseudophakic image quality.
Currently in the United States, these presbyopia-correcting IOL designs include spherical progressive zonal refractive, aspheric full-aperture diffractive, spherical, and, more recently, aspheric apodized-diffractive-refractive, spherical and aspheric accommodating, and an accommodating IOL with central bispheric optic modification. In the near future, we will likely have toric versions of all of the above, along with dual-optic accommodating IOLs and shape-changing accommodating IOLs, to name just a few. In this study, we compared 5 intraocular lenses that have been approved by the US Food and Drug Administration (FDA) for the treatment of aphakia and presbyopia. The optical features of the Crystalens AO (model AT-50AO; Bausch & Lomb Surgical, Aliso Viejo, California, USA), Crystalens HD (model HD-500; Bausch & Lomb Surgical), AcrySof IQ ReSTOR +4 (model SN6AD3; Alcon Laboratories, Fort Worth, Texas, USA), AcrySof IQ ReSTOR +3 (model SN6AD1; Alcon Laboratories), and Tecnis Multifocal Acrylic (model ZMA00; Abbott Medical Optics, Irvine, California, USA) are described in Table 1 .
| Intraocular lens | |||||
|---|---|---|---|---|---|
| Crystalens AO | Crystalens HD | ReSTOR +3 | ReSTOR +4 | Tecnis MF | |
| Optic material | Silicone | Silicone | Acrylic | Acrylic | Acrylic |
| Optic diameter | 5.0 mm | 5.0 mm | 6.0 mm | 6.0 mm | 6.0 mm |
| Anterior optic design | Aberration-free aspheric | Bispheric | Apodized diffractive bifocal, add = 3 D | Apodized diffractive bifocal, add = 4 D | Modified prolate aspheric |
| Posterior optic design | Aberration-free aspheric | Spherical | Aspheric | Aspheric | Diffractive bifocal, add = 4 D |
| Spherical aberration | 0 | N/A due to zone discontinuity at 1.5 mm radius | −0.1 μm | −0.1 μm | −0.27 μm |
With each presbyopia-correcting IOL design strategy, there are inherent tradeoffs with regard to depth of focus, contrast sensitivity, loss of light energy to useless foci, night glare and photic phenomenon, and near, intermediate, and distance image quality at any given pupil diameter. The better we can assess and model the optical performance of each IOL at different vergences and pupil diameters, the more information we have by which to custom-match different presbyopia-correcting IOLs for individual patients, who may have marked differences in pupil size, shape, and dynamics, all of which may further change with advancing age.
While not the only image quality metric, image sharpness is an important element of image quality. As per International Organization for Standardization (ISO) standard 11979, the United States Air Force (USAF) 1951 target is routinely employed to subjectively determine the spatial resolution efficiency of the IOL. In this study, we used an image sharpness algorithm similar to that commonly used in photography to provide an objective computation of the image sharpness of the 1951 USAF target imaged through a model eye incorporating each of 5 presbyopia-correcting IOLs. To our knowledge, this is the first study to use the standard 1951 USAF target linked to an objective measure of image sharpness by which to compare 5 presbyopia-correcting IOLs in a model eye system.
Methods
Test Articles
Tognetto and associates investigated the optical quality of 3 lenses each of 23 different IOL models and found almost no intramodel variance in the optical quality. Hence, in the current study, 1 representative lens of the following 5 presbyopia-correcting IOL models was measured: Crystalens AO (model AT-50AO), referred to herein as AO; Crystalens HD (model HD-500), referred to herein as HD; ReSTOR +3 (model SN6AD1), referred to herein as R3; ReSTOR +4 (model SN6AD3), referred to herein as R4; and Tecnis Multifocal acrylic (model ZMA00), referred to herein as TMF.
The key optical properties of the 5 different presbyopia-correcting IOL models are listed in Table 1 . The Tecnis Multifocal had a labeled dioptric power of +21.0 diopters (D) and all other IOLs had a labeled dioptric power of +20.0 D.
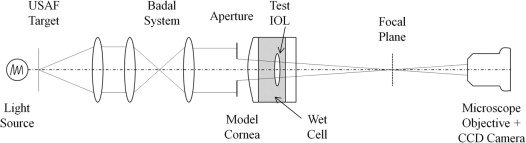
Measurement Apparatus
The apparatus used to measure the through-focus imaging quality of different IOL models is shown schematically in Figure 1 . The apparatus consisted of the following key components: target assembly, Badal relay assembly, and model eye/camera assembly. The target assembly consisted of a light source, a diffuser, a 1951 USAF resolution target, and an achromatic collimating lens. The light source was a high-intensity broadband halogen lamp. The Badal relay assembly consisted of 2 achromatic lenses, and the distance between the 2 lenses was adjusted to achieve different object vergences. The model eye/camera assembly consisted of a circular aperture simulating the entrance pupil, a model cornea, the test IOL, a glass window, a microscope objective, and a charge-coupled device (CCD) camera. The 3-mm space between the model cornea and the glass window contained balanced salt solution (BSS) at ambient temperature. The model cornea is a custom-made polymethylmethacrylate singlet with a focal length of 23 mm (43.5 diopters [D]) and aspheric anterior and posterior surfaces fabricated to achieve spherical aberration of +0.27 μm over the central 6-mm zone. These values were chosen because they approximate average values of measured human corneas. Four fixed aperture diameters (3, 4, 5, and 6 mm) were used. In this optical system, the range of angular spatial frequencies represented by the 1951 USAF resolution target is 14 cycles per degree (cpd) to 200 cpd.
Measurement Procedure
The test IOL and fixed aperture were assembled together to ensure precise centration. Then the IOL/aperture assembly was accurately positioned and centered within the model eye. The space between the model cornea and glass window was filled with BSS (Alcon Laboratories, Fort Worth, Texas, USA), and the model eye/IOL assembly was allowed to equilibrate for at least 1 hour. With the Badal assembly set for an object vergence of zero, the distance between the glass window and the camera assembly was adjusted to achieve best focus. The projected image of the USAF resolution target was captured for each object vergence between −1.0 D and +4.0 D in 0.125-D steps. The level of the light source was set such that each image had the same total intensity. Although the Crystalens models are accommodating lenses, the Crystalens lenses were measured in a static, nonaccommodated position for all object vergences. Once all images were captured for each combination of IOL model, aperture diameter, and object vergence, the sharpness score of each image was objectively determined and plotted vs object vergence, as described in the next section.
Two-Dimensional Image Sharpness Score
The sharpness score of each image was objectively determined using a 2-dimensional sharpness gradient (MatLab; MathWorks, Natick, Massaschusetts, USA). [Fx,Fy] = gradient(F) where F is the 2D image file, Fx and Fy are the x-direction and y-direction intensity gradient of each pixel, respectively. Then sum square of Fx and Fy is calculated for each pixel. The total sum of sum square values of all pixels is the sharpness score:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


