Purpose
To report the results of Descemet stripping automated endothelial keratoplasty (DSAEK) to treat endothelial failure in eyes with buphthalmos.
Design
Prospective interventional case series.
Methods
All buphthalmic eyes with endothelial failure undergoing DSAEK by the same surgeon (M.B.) between March 2007 and January 2012 were included. Outcome measures included best spectacle-corrected visual acuity (BSCVA), refraction, and endothelial cell loss (assessed 6, 12, 24, 36, and 48 months postoperatively). Standardized DSAEK was performed in all cases, with minor modifications in phakic and aphakic eyes. Other outcomes included comparisons to penetrating keratoplasty (PK) published results and comparisons to visual outcomes in DSAEK for other indications.
Results
There were 14 transplants performed in 12 eyes (11 patients). Mean age was 34.9 years (range 15-54 years). The average follow-up was 21.7 ± 13.8 months (range 6-48 months). At last follow-up examination, BSCVA had improved in 11 of 13 cases, with a logMAR average value ± standard deviation of 0.74 ± 0.66 from the preoperative value of 2.07 ± 0.80. Eleven eyes reached Snellen acuity of 20/200 or better, and 5 eyes reached 20/40 or better. Mean endothelial cell loss was 40.5% ± 8.9% (range 23.7%-53.1%). Complications included graft detachment (n = 2), glaucoma progression (n = 1), and late endothelial failure (n = 1). All complications were managed successfully either by repeat DSAEK (n = 2), rebubbling (n = 1), or cyclocryocoagulation (n = 1).
Conclusions
DSAEK may be performed safely and effectively in buphthalmic eyes, with comparable results to outcomes after PK. Visual outcomes are not substantially different after DSAEK for this indication compared to DSAEK for other indications.
Endothelial dysfunction is relatively common in buphthalmos: the high intraocular pressure (IOP) results in stretching of the sclera and cornea, damaging the Descemet membrane (DM) and the endothelial layer, resulting in breaks and subsequent formation of Haab striae. More importantly, multiple intraocular surgeries are often required throughout the life of these young patients to manage the glaucoma and other associated pathologies, further contributing to the progressive decline of endothelial cell density.
Traditionally, endothelial failure in patients with buphthalmos has been treated with penetrating keratoplasty (PK), but visual prognosis of this surgical approach is guarded because of comorbidities (ie, advanced glaucomatous optic neuropathy and amblyopia) and the higher-than-normal intraoperative complication and postoperative failure rates.
During the past decade, Descemet stripping automated endothelial keratoplasty (DSAEK) has been established as a successful treatment for endothelial failure in Fuchs endothelial dystrophy or pseudophakic bullous keratopathy. However, to date, only 1 case of DSAEK for the treatment of buphthalmos has been reported; this may reflect on the reluctance among surgeons to perform a relatively new procedure in eyes that have a rare and often complex condition.
We report herein the results of the first prospective case series of eyes with buphthalmos with endothelial failure that underwent DSAEK; we further report on a modified surgical technique for these challenging cases.
Methods
This prospective study, undertaken to evaluate the outcomes of DSAEK for endothelial failure in the setting of buphthalmos, was approved by the University of Magna Graecia Institutional Review Board on November 27, 2006 (Study number 107/06). The research protocol adhered to the tenets of the 1964 Declaration of Helsinki for clinical research. All patients undergoing surgery or their legally responsible guardians (if patients were not of age to provide their own legal consent) provided informed consent to participate in this research study, and provided informed consent regarding the risks related to the presence of buphthalmos.
All patients scheduled for DSAEK for endothelial failure in the setting of buphthalmos between March 1, 2007 and December 31, 2011 were included (n = 11 patients/12 eyes). All surgeries were performed by 1 surgeon (M.B.). A standard spreadsheet program was used to collect and analyze data pertaining to the visual results and survival of the transplants.
A complete ophthalmic history, including previous ocular surgeries, lenticular status, medical and surgical management of glaucoma, and date of onset of corneal decompensation was obtained for each patient. All patients underwent a complete ophthalmologic examination including slit-lamp examination, best spectacle-corrected visual acuity (BSCVA), manifest refraction, applanation tonometry, fundoscopy, and B-scan ultrasound (if required) preoperatively and again at 6, 12, 24, 36, and 48 months after DSAEK. Low visual acuity and/or poor visualization prevented visual field testing or optic nerve head assessment before patients underwent DSAEK. Of the 12 eyes, 5 were phakic, 4 were aphakic, and 3 were pseudophakic with a posterior chamber IOL already in place.
Baseline donor endothelial cell density was measured by the provider eye bank by means of fixed frame technique at 100× magnification by specular microscopy (mean of 5 different counts). Postoperative endothelial cell density was measured with automated noncontact specular microscopy (EM-3000; Tomey GmbH, Erlangen, Germany), beginning at the 6-month follow-up.
Surgical Technique
Surgery was performed under peribulbar anesthesia in 10 of the 12 eyes (50% mixture of lidocaine 2% and bupivacaine 0.5%). The remaining 2 eyes (both eyes of the same 15-year-old boy) had surgery performed under general anesthesia, with additional peribulbar anesthesia administered at the start of the case.
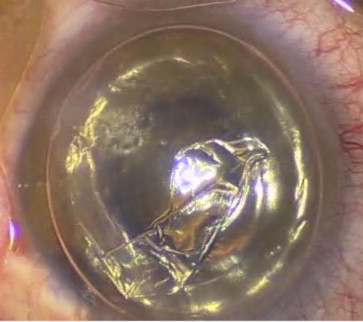
All eyes underwent a standardized DSAEK with the surgeon sitting at the 12 o’clock position, following the technique published previously. DM was removed under air starting at the site of the Haab striae, which peeled off, showing no attachment to the overlying stroma ( Figure 1 ). An inferior peripheral iridotomy was performed in all cases, even though a complete air fill was not expected to last in eyes with previous filtering surgery. In all cases, the increased size of the recipient cornea, the difficult intraoperative visualization, and the presence of the natural lens prompted changes as described in detail below.
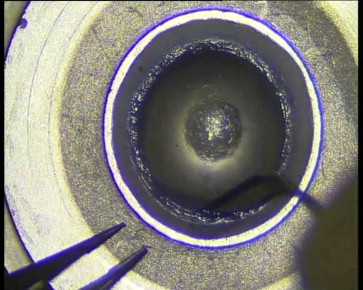
Because the recipient corneas were enlarged as a result of buphthalmos, the donor graft size was increased to 9.5-10.5 mm to allow approximately 1 mm between the edge of the donor tissue and the corneoscleral limbus, as is typical in other DSAEK procedures. In each case, donor tissue was mounted on the artificial anterior chamber of the ALTK system (Moria, Antony, France) and then dissected with a single microkeratome pass. After discarding the anterior lamella, a round, sharp microfeather blade (Feather, Osaka, Japan) was used to manually dissect the peripheral cornea from the base of the keratectomy up to the edge of the artificial anterior chamber for the entire 360 degrees ( Figure 2 ), thereby including the corneoscleral limbus. The dissected rim was excised with corneal scissors while the tissue was still mounted on the artificial anterior chamber. The circumference of the dissected surface was then marked with trypan blue, and the donor tissue was punched to the desired size. We ensured proper centration to avoid peripheral nondissected tissue of uneven thickness.
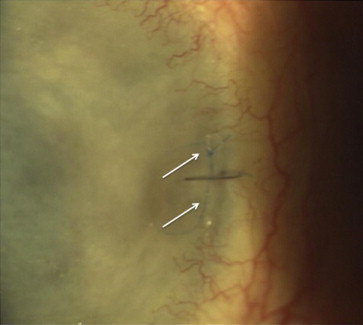
In the aphakic cases, the absence of a barrier between the anterior chamber and the vitreous cavity, coupled with the poor visualization that was caused by severe and chronic corneal edema, mandated the use of a transcorneal suture (10-0 prolene) to fixate the donor tissue to the recipient temporal cornea in the periphery ( Figure 3 ). This technique was first described by Patel and associates, whereby a temporal attachment is obtained between donor and host to be used intraoperatively, and as a reference point for air reinjection when requiring rebubbling. Each aphakic eye underwent 4 full-thickness corneal venting incisions in the host stroma. Price and Price first described this method as a means to help drain the interface fluid that could not be removed by air tamponade.
In the phakic cases, incision sites were shifted superiorly by about 1 clock hour to eliminate the risk of passing the surgical instruments across the pupil over the unprotected crystalline lens, thus minimizing the possibility of surgically induced cataract formation. This method has been described in more detail previously.
Postoperatively, all patients were instructed to remain in a supine position for 2 hours and were then examined with the slit lamp. When no aqueous was present in the anterior chamber or its level was below the inferior iridotomy, some air was removed through 1 of the side entries.
If a graft detached, air was reinjected without delay; in the eyes with a temporal fixation suture, a paracentesis was created beneath the location of the suture. When necessary, wounds were resutured to ensure adequate air tamponade.
Postoperatively, all patients were given topical tobramycin 0.3% / dexamethasone 0.2% suspension combination therapy (Tobradex, Fort Worth, Texas, USA) every 2 hours for 2 weeks, then every 3 hours for 2 additional weeks. Treatment was switched to dexamethasone 0.1% (Luxazone, Allergan SpA, Rome, Italy) in a tapering regimen: 4 times daily for 1 month, to 3 times daily for a subsequent month, to twice daily in the third month, and then once daily indefinitely unless the patient was phakic or a steroid responder, in which case the steroid drops were ceased after a further 1 month. All sutures were removed 4-6 weeks post surgery. Patients continued their regular glaucoma regimens, modified as needed.
Results
The study group consisted of 14 DSAEK procedures in 12 eyes of 11 patients. Mean age was 34.9 ± 9.7 years (range, 15-54 years). All patients had developed corneal edema in late childhood or early adulthood. Preoperatively, all patients had diffuse corneal edema, with increased maximum corneal diameter with or without Haab striae. Despite multiple ocular surgeries, none of the corneas exhibited neovascularization ( Figure 4 ).
Five eyes were phakic (1 with cataract), 4 were aphakic, and 3 were pseudophakic with a posterior chamber intraocular lens. All but 2 eyes in this series had a varying degree of glaucomatous optic neuropathy. No eyes had nystagmus, relative afferent pupillary defect, or strabismus. Three eyes had amblyopia. Seven eyes had previous trabeculectomy ( Table ).
| Case | Patient | Age | Eye | Comorbidities | Previous Surgeries a | Lens | BSCVA Preop | BSCVA Postop | F/U (mo) | ECL % |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | A | 15 | OD | G | Gs3, L1 | A | HM | 20/400 | 42 | 53.1 |
| 2 | A | 15 | OS | G | Gs2, L1 | A | HM | 20/200 | 36 | 42.8 |
| 3 | B | 39 | OD | G | Gs4, L1, Cs1 | A | CF | 20/200 | 24 | 48.2 |
| 4 | C | 45 | OS | G, ROP | Gs6, L1, R22 | A | CF | CF | – b | – b |
| 5 | C | 45 | OS | G, ROP | Gs6, L1, R22 | A | CF | 20/100 | 18 | n/a |
| 6 | D | 30 | OS | G | Gs2 | P | CF | 20/32 | 48 | 41.5 |
| 7 | E | 31 | OD | G, C | Gs2 | P c | 20/60 | 20/28 | 6 | 23.7 |
| 8 | F | 32 | OD | Am | Gs3, L1 | P | CF | CF | 24 | 28.2 |
| 9 | G | 33 | OS | G, Am | Gs2 | P | CF | 20/40 | 12 | 51.0 |
| 10 | H | 36 | OD | G, Am | Gs2, Cs1 | P | CF | 20/60 | 6 | 40 |
| 11 | I d | 33 | OS | G | Gs3, Cs2 | PCIOL | HM | 20/60 d | 12 | – d |
| 12 | I | 33 | OS | G | Gs3, Cs3 | PCIOL | HM | 20/100 | 6 | 40.7 |
| 13 | J | 36 | OS | G | Gs3, L1 | PCIOL | CF | 20/16 | 24 | 36.5 |
| 14 | K | 54 | OS | G | Gs3, L1 | PCIOL | 20/70 | 20/25 | 24 | 39.9 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


