Purpose
To study the scope of dry eye syndrome (DES) in veterans on a national level and to evaluate the relationship between psychiatric diagnoses and DES.
Design
Case-control study.
Methods
Setting : Patients were seen in a Veterans Affairs (VA) eye clinic between 2006 and 2011. Patient population : Patients were divided into cases and controls with regard to their dry eye status (cases = ICD-9 code for DES plus dry eye therapy; controls = patients without ICD-9 code plus no therapy). Main outcome measures : The prevalence of DES and the influence of psychiatric diagnoses on the risk of DES.
Results
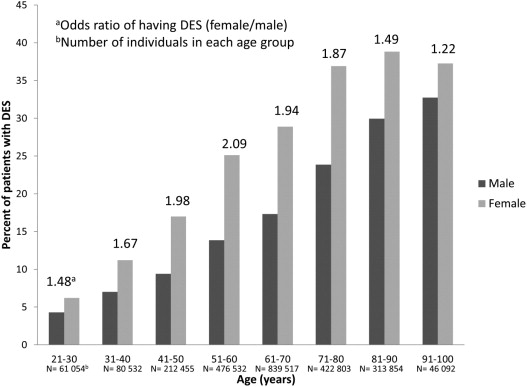
A total of 2 454 458 patients were identified as either a dry eye case (n = 462 641) or control (n = 1 991 817). Overall, 19% of male patients and 22% of female patients had a diagnosis of DES, with female sex imparting an increased risk of DES at each decade compared to male sex (odds ratio [OR] 1.22–2.09). Several conditions were found to increase DES risk, including post-traumatic stress disorder (OR 1.92, 95% CI 1.91–1.94) and depression (OR 1.92, 95% CI 1.91–1.94) (analyses adjusted for sex and age). The use of several systemic medications was likewise associated with an increased risk of DES, including antidepressant medications (OR 1.97, 95% CI 1.79–2.17) and antianxiety medication (OR 1.74, 95% CI 1.58–1.91). Multivariate analysis (adjusted for age and sex) revealed that for psychiatric diagnoses, both the use of medication and the diagnosis remained significant risk factors when considered concomitantly, although the magnitude of each association decreased.
Conclusions
DES is a disease associated with depression and post-traumatic stress disorder, and is prevalent among male and female veterans receiving eye care services. The association could be driven by underlying disease physiology or medications used to treat psychiatric conditions. Regardless of the causal link, this suggests that individuals with a known psychiatric diagnosis should be questioned about dry eye symptoms and, if applicable, referred to an eye care physician.
Dry eye syndrome (DES) is a prevalent condition both in the United States and worldwide, with manifestations that negatively impact physical and mental functioning. We felt that it was essential to study the scope of DES specifically in the Veterans Affairs population, as veterans as a group have demographic characteristics, exposures, and medical profiles that are different from previously studied populations. Specifically, while previous US populations have focused on mainly female and/or non-Hispanic white populations, veterans are a predominantly male population with a diverse racial and ethnic make-up. A recent evaluation of the scope of DES in Miami veterans found a high prevalence of disease in this population, with 12% of male and 22% of female patients carrying a diagnosis of DES. The presence of a psychiatric diagnosis, including depression and post-traumatic stress disorder (PTSD), and the use of psychiatric medication imparted a 2-fold risk of having a DES diagnosis. This study highlighted that DES is present in both male and female patients and suggested that veterans may be uniquely more susceptible to DES given the comorbidities found in this population. A limitation of the study, however, was that it only looked at a demographically select subset of veterans and therefore the generalizability of data onto a national veteran population was uncertain.
The Veterans Affairs (VA) has recently created a centralized data warehouse that contains merged information from several VA clinical and administrative systems. The premise behind its creation was that the incorporation of data from multiple differing data sets throughout the VA into 1 standard database structure would facilitate reporting and data analysis. The goal of this study, therefore, was to use this national data set to study the scope of DES in veterans on a national level and to evaluate the relationship between important comorbidities in veterans and DES, especially the relationship between psychiatric diagnoses and DES.
Methods
Study Population
All patients seen in a VA eye clinic between July 5, 2006 and July 4, 2011 were included in this retrospective analysis. As the data included patients from 365 VA eye clinics in all Veterans Integrated Service Networks (VISNs), it captured all veterans that were seen in a US VA eye clinic during the study period. Patients seen in VA clinics consist of ex-military personnel but do not include or represent all former military personnel. Patients seen in other Veterans Affairs outpatient clinics during this time period were not included as a preliminary analysis revealed that non–eye care professionals did not use the ICD-9 code for DES. Patients were divided into cases and controls with regard to their dry eye status. Cases included patients with an International Classification of Disease code (ICD-9) for DES (375.15) who received some form of dry eye therapy (n = 462 641); controls included patients who received eye clinic care but who did not have an ICD-9 code for DES and did not receive any form of dry eye therapy (n = 1 991 817). Dry eye therapies included: any type of artificial tear, gel, or ointment; topical cyclosporine 0.05% (Restasis); or punctal plugging procedure (Current Procedural Terminology [CPT] codes 68760 and 68761). Patients were excluded from the risk factor analysis if they had discordant dry eye information (eg, an ICD-9 diagnosis but no dry eye therapy or no ICD-9 diagnosis but with dry eye therapy).
Data Collection
All data were extracted from the Corporate Data Warehouse (CDW) by an expert programmer (A.L.F.) and automatically converted into an SPSS format. The Veterans Administration’s Corporate Data Warehouse is a national repository comprising data from several Veterans Health Administration (VHA) clinical and administrative systems. The CDW operates within the VA Office of Information & Technology Field Operations Business Intelligence Service Line. CDW data are stored in a relational database. Multiple VA data sources are merged so that cohorts are definable by attributes such as ICD-9 codes and CPT codes from both inpatient and outpatient encounters or from abnormal values of vital signs like blood pressure, weight, and height, within a target time period. These data sets are kept current by frequent updates with new data from the source databases so timely data are available for research.
The data used for this analysis were extracted from the CDW Encounters tables. The source of CDW Encounters is the National Patient Care Database, or NPCD. NPCD provides a single flat file to CDW on each business day that contains the most recent inserts and updates. CDW Encounters is normally current to within a couple of days. This extraction included demographic information (date of birth, sex, race, ethnicity), medical diagnosis information (extracted based on ICD-9 codes), use of systemic therapy (extracted based on pharmacy codes), and procedures (extracted based on CPT codes).
Main Outcome Measures
The main outcome measure was prevalence of DES and its associated risk factors.
Statistical Analysis
All statistical analyses were performed using SPSS 18.0 (SPSS Inc, Chicago, Illinois, USA) statistical package. Continuous variables were compared between the groups using the Student t test and categorical variables were compared using the χ 2 test. Multivariate logistic regression analysis (using the presence of DES as the dependent variable) was used to evaluate the effect of various risk factors on DES. All multivariate analyses were adjusted for sex and age.
Results
Dry Eye Syndrome Prevalence
During the studied period, 3 133 262 patients were seen in a VA eye clinic. After excluding discordant cases (n = 120 061 with an ICD-9 code for DES but no DES therapy; n = 558 743 with DES therapy but no ICD-9 code for DES), a total of 2 454 458 patients were identified as being either a dry eye case (n = 462 641) or control (n = 1 991 817). The period prevalence for these patients was 19% (n = 462 641/2 454 458).
Risk Factor Analysis of Demographic Characteristics
Overall, 19% of male patients and 22% of female patients had a diagnosis of DES, with female sex imparting an increased risk of DES at every age group (odds ratio [OR] 1.22–2.09) ( Figure ). The mean age of our population was 64.2 years (SD 14.26). The Figure depicts the percentage of patients with DES by decade of age and sex; the overall risk of DES increased by 1.42 for each increasing decade (95% confidence interval [CI] 1.42–1.42). The Veterans Affairs administrative database did not have complete information on self-identified race and ethnicity (this information was available for 86% of patients). With this limitation, identification as being nonwhite increased the risk of DES, with the OR for blacks, Asians or Pacific Islanders, and American Indians being 1.41, 1.29, and 1.28, respectively, compared to whites ( Table 1 ). While Hispanics comprised only a small percentage of the total veteran population (0.7%), Hispanics had a 1.69-fold higher risk of DES than their non-Hispanic counterparts (risk adjusted for age and sex).
| Patient Characteristic | Number a | Percent b | OR c |
|---|---|---|---|
| Race | |||
| White | 321 017 | 20% | — |
| Black | 85 553 | 21% | 1.41 (1.39–1.42) |
| Asian or Pacific Islander | 8386 | 21% | 1.29 (1.26–1.32) |
| American Indian or Alaskan | 2739 | 20% | 1.28 (1.22–1.33) |
| Ethnicity | |||
| Hispanic | 4254 | 30% | 1.66 (1.60–1.72) |
| Not Hispanic | 413 441 | 20% | — |
a Number of patients with dry eye syndrome (present if ICD-9 code 375.15 and received some form of dry eye therapy).
b Percent in group with dry eye syndrome.
c Odds ratio (OR) adjusted for sex and age. An OR greater than 1 represents an increased likelihood of dry eye syndrome.
Risk Factor Analysis of Medical Conditions
Systemic diagnoses were identified in the administrative database using ICD-9 codes. After adjusting for sex and age, several medical conditions were found to increase DES risk in our population ( Table 2 ). The magnitude of increased risk was highest in patients with sleep apnea (OR 2.46), rosacea (OR 2.29), nonautoimmune arthritis (OR 2.28), depression (OR 1.92), and PTSD (OR 1.92). The overall period prevalence of depression in our population was 22% and in those with the diagnosis 24% had DES, compared to 18% without depression. The overall prevalence of PTSD in our population was 18% and in those with the diagnosis 24% had DES, compared to 18% without PTSD. Combining both groups, the positive predictive value of a psychiatric disorder (PTSD and/or depression) on DES ranged from 6% in the 21-to-30 age group to 44% in the 81-to-90 age group, reflecting the increasing prevalence of DES with increasing age. In a forward stepwise regression model considering age, sex, and all medical diagnoses, the presence of depression (OR 1.34, 95% CI 1.33–1.35) and PTSD (OR 1.43, 95% CI 1.42–1.45) remained significant predictors of DES risk.
| Medical Condition | Number a | Percent b | OR c |
|---|---|---|---|
| Vascular | |||
| Diabetes mellitus: | |||
| yes | 215 844 | 20% | 1.06 (1.06–1.07) |
| no | 246 797 | 18% | — |
| Hypertension: | |||
| yes | 380 918 | 22% | 1.82 (1.80–1.83) |
| no | 81 723 | 11% | — |
| Lipid metabolism disorder: | |||
| yes | 358 630 | 22% | 1.56 (1.55–1.57) |
| no | 104 011 | 13% | — |
| Ischemic heart disease: | |||
| yes | 192 333 | 26% | 1.55 (1.54–1.56) |
| no | 270 308 | 16% | — |
| Cerebral vascular disease: | |||
| yes | 100 966 | 29% | 1.61 (1.60–1.63) |
| no | 361 675 | 17% | — |
| Psychiatric | |||
| Psychiatric illness: | |||
| yes | 210 960 | 24% | 1.88 (1.87–1.90) |
| no | 251 681 | 16% | — |
| PTSD: | |||
| yes | 105 239 | 24% | 1.92 (1.91–1.94) |
| No | 357 402 | 18% | 1.00 |
| Depression: | |||
| yes | 126 831 | 24% | 1.92 (1.91–1.94) |
| no | 335 810 | 18% | — |
| Alcohol dependence: | |||
| yes | 52 316 | 19% | 1.33 (1.31–1.34) |
| no | 410 325 | 19% | — |
| Drug dependence: | |||
| yes | 157 542 | 19% | 1.33 (1.32–1.34) |
| no | 305 099 | 19% | — |
| Autoimmune & arthritis | |||
| Autoimmune disease d : | |||
| yes | 110 700 | 31% | 2.18 (2.17–2.20) |
| no | 351 941 | 17% | — |
| Nonautoimmune arthritis: | |||
| yes | 281 148 | 27% | 2.28 (2.26–2.29) |
| no | 181 493 | 13% | — |
| Gout: | |||
| yes | 52 532 | 27% | 1.48 (1.46–1.50) |
| no | 410 109 | 18% | — |
| Thyroid disease: | |||
| yes | 23 812 | 31% | 1.81 (1.78–1.83) |
| no | 438 829 | 19% | 1.00 |
| Prostate | |||
| Benign prostatic hyperplasia: | |||
| yes | 178 091 | 28% | 1.74 (1.73–1.75) |
| no | 284 550 | 16% | — |
| Prostate cancer: | |||
| yes | 47 479 | 27% | 1.21 (1.19–1.22) |
| no | 415 162 | 18% | — |
| Miscellaneous | |||
| Sleep apnea: | |||
| yes | 27 798 | 33% | 2.46 (2.43–2.50) |
| no | 434 843 | 18% | — |
| Rosacea: | |||
| yes | 21 097 | 37% | 2.29 (2.25–2.34) |
| no | 441 544 | 18% | — |
| HIV: | |||
| yes | 3009 | 19% | 1.41 (1.35–1.47) |
| no | 459 632 | 19% | 1.00 |
| Chemotherapy: | |||
| yes | 9452 | 30% | 1.54 (1.50–1.58) |
| no | 453 189 | 19% | — |
| Ocular | |||
| Glaucoma: | |||
| yes | 164 171 | 28% | 1.84 (1.83–1.85) |
| no | 298 470 | 16% | — |
a Number of patients with dry eye syndrome (present if ICD-9 code 375.15 and received some form of dry eye therapy).
b Percent in group with dry eye syndrome.
c Odds ratio (OR) adjusted for sex and age. An OR greater than 1 represents an increased likelihood of dry eye syndrome.
d Autoimmune diseases include: Behcet syndrome, sarcoidosis, systemic lupus erythomatosis, rheumatoid arthritis, Wegener granulomatosis, vasculitis, vitiligo, psoriasis, ankylosing spondylitis, inflammatory bowel disease, Reiter syndrome, autoimmune hepatitis, and collagen vascular diseases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


