Purpose
To develop a new method to quantify the choroidal vessel density by binarizing ultra-wide-field indocyanine green angiography (ICGA) images and determine whether values are altered in diseased eyes.
Design
Reliability and validity analysis.
Methods
Ultra-wide-field fluorescein angiography (FA) and ICGA images were obtained using an ultra-wide-field imaging device (Optos California ultra-wide-field imaging device; Dunfermline, Scotland, UK) in 11 eyes of 11 patients without chorioretinal diseases. The angiographic signals of the choroidal vessels were determined by subtracting those of the retinal vasculature and optic disc on the FA images from the ICGA images, binarized by Niblack’s method, and the choroidal vessel density calculated. Reproducibility of the method was assessed by calculating the coefficient of variance, coefficient of repeatability, and intraclass correlation coefficient. The relationships between age, spherical equivalent refractive error (SERE), and intraocular pressure and the vasculature density were assessed. To investigate possible impacts of chorioretinal diseases on the vasculature density, 10 eyes of 7 patients with central serous chorioretinopathy (CSC) were compared with the 11 control eyes.
Results
Choroidal vessels were contrasted by binarizing ICGA images. The method to quantify the choroidal vessel density showed high reproducibility. The SERE was correlated significantly (r = 0.573, P < .05) with the vasculature density. In the 11 control eyes, the vasculature density was 34.26% ± 0.77% in the entire area, 31.37% ± 0.97% in the superior portion, 36.98% ± 0.88% in the inferior portion, 37.01% ± 1.44% in the posterior portion, and 34.17% ± 0.77% in the peripheral portion. In eyes with CSC, the density was significantly ( P < .05) higher: 36.46% ± 0.49%, 34.02% ± 0.97%, 38.65% ± 0.27%, 41.04% ± 0.82%, and 36.36% ± 0.51%, respectively.
Conclusions
Binarization of ultra-wide-field ICGA images enabled quantification of the choroidal vessel density, which was altered in eyes with CSC. This method of measuring the choroidal vessel density may provide new insights into diagnosing and treating chorioretinal diseases.
Panoramic images obtained using scanning laser ophthalmoscopy provide new pathologic findings in the peripheral retina in a variety of chorioretinal diseases such as diabetic retinopathy, retinal vein occlusion, myopia, age-related macular degeneration (AMD), and retinitis pigmentosa.
A new device, the Optos ultra-wide-field retinal imaging device “California” (Dunfermline Scotland, UK), enables imaging up to 200 degrees in a single capture. This device can capture consecutive ultra-wide-field fluorescein angiography (FA) and indocyanine green angiography (ICGA) images, equipped with light sources of emission wavelength of 488 nm for FA and 802 nm for ICGA. Ultra-wide-field ICGA has been previously performed in several chorioretinal diseases using a modified Optos 200Tx. Panoramic FA and ICGA, autofluorescence, and fundus images are acquired rapidly by single capture using this device, in contrast to other panoramic images composed manually or with computer software, which had difficulties with imaging the peripheral retina, illumination irregularities, and time gaps among individual pictures. Thus, high-contrast whole images of choroidal vessels can be obtained by the Optos device.
A subtraction technique of sequential ICGA images can analyze pathologic changes in the choroidal veins. In the current study, we subtracted the fluorescent signals from the retinal vasculature and the optic disc on the FA images from the ICGA images, which further enhanced preferential visualization of the choroidal vessels with higher contrast throughout the fundus. To quantify the vascular density, we applied Niblack’s binarization method, which Sonoda and associates used to detect the choroidal structure on optical coherence tomography (OCT) images. To evaluate the feasibility of this new method to quantify the choroidal vasculature, we assessed the repeatability of the calculations and the correlations with possible factors affecting the choroidal circulation and compared eyes with and without central serous chorioretinopathy (CSC), because choroidal vessels are dilated in eyes with CSC.
Methods
Subjects
The Ethics Committee of the Nagoya City University Hospital approved this retrospective study. This clinical trial is registered in UMIN-CTR (UMIN-ID: UMIN000021450). The procedures used conformed to the tenets of the Declaration of Helsinki.
Eleven healthy fellow eyes of 11 patients (5 men, 6 women; average age, 64.4 ± 5.2 years; spherical equivalent refractive error [SERE] in phakic eyes, −1.7 ± 0.9 diopters [D]) were included. The control patients originally underwent FA and ICGA owing to unilateral macular edema secondary to branch retinal vein occlusion, because of unilateral traumatic choroidal rupture, or to rule out chorioretinal diseases. Angiographic images in fellow eyes of these patients were used as controls. Ten eyes of 7 consecutive patients (6 men, 1 woman; average age, 56.9 ± 6.6 years; SERE in phakic eyes, −2.4 ± 1.0 D) were included in the group with CSC. The average age and SERE did not differ significantly ( P = .36 and P = .86, respectively) between the 2 groups. All patients underwent ultra-wide-field FA and ICGA with the retinal imaging device between May 1, 2015 and October 31, 2015 at Nagoya City University Hospital. Patients with hypertension, diabetes mellitus, and hypercholesterolemia that could affect ocular circulation, as well as patients with high myopia (defined as SERE in phakic eyes <−8.0 D), were excluded.
Ultra-Wide-Field Fluorescein Angiography and Indocyanine Green Angiography
Ultra-wide-field FA and ICGA were performed simultaneously after an intravenous injection of 5 mL of 10% sodium fluorescein and 25 mg of ICGA. The retinal device recorded the images. The images in the early phase (2 minutes after dye injection) were used for analyses because the contrast of the choroidal vessels became obscured as the fluorescent background signals increased.
Subtraction and Binarization of Ultra-Wide-Field Indocyanine Green Angiography Images
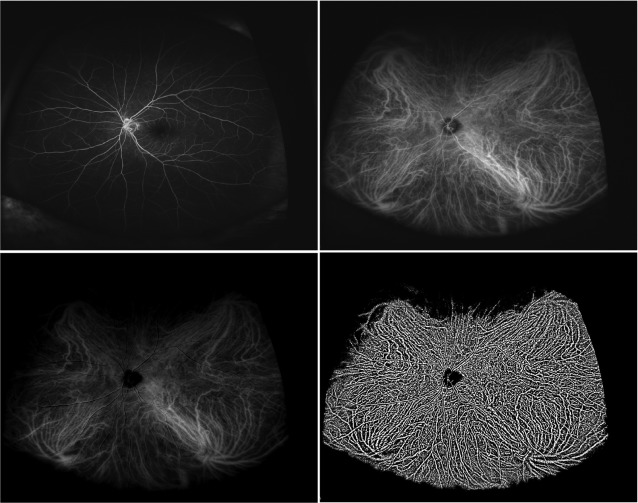
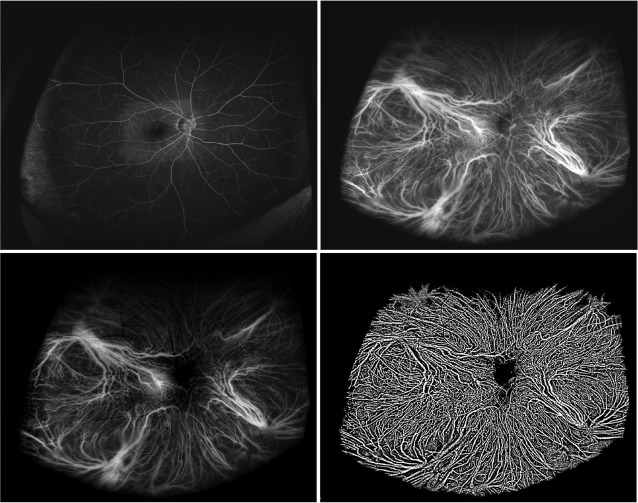
Digital FA and ICGA images were processed for subtraction and binarization using ImageJ software (National Institutes of Health, Bethesda, Maryland, USA; available at http://rsb.info.nih.gov/ij/index.html ) ( Figures 1 and 2 ) in eyes with and without a chorioretinal disease. To exclude fluorescent signals derived from the retinal vessels and the optic disc from the ICGA images, the FA images taken consecutively were subtracted from the ICGA images. After subtraction, the choroidal vessels had greater contrast throughout the fundus ( Figures 1 and 2 ). Binarization of the subtracted ICGA images then was performed by the modified Niblack method, as previously reported. Briefly, 2 points between the choroidal vessels were selected manually at each quadrant in a masked fashion, the averaged intensity of 8 points was set as the threshold for binarization, and the binarized images of the choroidal vessels were obtained ( Figures 1 and 2 ).
Densitometry of the Choroidal Vessels
To quantify the area of the choroidal vessels, the binarized ICGA images were trimmed and evaluated within a Bézier curve drawn to connect the points 160 pixels (approximately 1.5 mm) posterior to the ampullas of each vortex vein ( Figure 3 ), because the vortex veins had variations among eyes in the number, location, size, and diameter. Exactly, the actual distance between each point and the ampullas may be shorter or longer than 1.5 mm, because the magnification of the peripheral image on Optos varies depending on a refractive error. The total area and the area with choroidal vessels were measured in pixels using the ImageJ software. The choroidal vessel density was calculated using the following formula: (area with choroidal vessels)/(total area) × 100 (%). To assess the repeatability of this method to quantify the choroidal vessel density, 2 masked investigators (S.H. and A.K.) performed all digital processing steps. The average of the results calculated from each measurement was compared and the coefficient of variance, coefficient of repeatability, and intraclass correlation coefficient (ICC) were calculated from all values of 2 measurements. For intrarater agreement, the measurement was performed twice by a single examiner (S.H.).
To investigate the impact of possible factors affecting the choroidal circulation on the choroidal vessel density, we assessed the correlations between the choroidal vessel density and the patients’ age, intraocular pressure (IOP), and SERE in eyes without chorioretinal diseases.
To evaluate the relationship between the density and location of the choroidal vessels, the area within 3 mm from the fovea was defined as the posterior area and the outside of that was considered the periphery ( Figure 3 ). The area was divided into the superior and inferior areas by a line passing through the fovea and the center of the optic disc, which was determined from original FA images ( Figure 3 ). In addition, to determine whether chorioretinal diseases alter the choroidal vessel density, the densities in eyes with and without CSC were compared.
Choroidal Vessel Diameters in Eyes With and Without Central Serous Chorioretinopathy
To elucidate whether the change of choroidal vessel density was ascribed to vasodilation or increased vascular plexus, the diameters of choroidal vessels were calculated using Photoshop CS5.1 (Adobe Systems Inc, San Jose, California, USA) and ImageJ software ( Supplementary Figure , available at AJO.com ). Briefly, the ICGA image processed by subtraction and binarization was trimmed by Photoshop CS5.1 to yield a fovea-centered circle with 1040 pixels (approximately 12 mm) in diameter and 20 pixels in width. After the minimum and maximum threshold of the area were set to exclude meandering or branching vessels, the number and the area of choroidal vessels were automatically measured by the “Analyze Particles Tool” in the ImageJ software. Mean choroidal vessel diameter was calculated by dividing mean area by 20 (pixels) and converting the unit to micrometers (μm) according to each magnification.
Statistical Analysis
All results are expressed as the means ± standard errors of the mean. All the statistical analyses were performed using SPSS software (IBM, Somers, New York, USA). The values were analyzed using the Mann-Whitney U test. The relationship between 2 variables was assessed by Kendall’s rank correlation. The Kruskal-Wallis and Bonferroni tests were used for multiple comparisons. The Bland-Altman method was used for coefficient of repeatability. P < .05 was considered statistically significant.
Results
Subtraction and Binarization of Ultra-wide-Field Fluorescein Angiography/Indocyanine Green Angiography Images
Subtraction of the FA image reduced the fluorescent signals from the retinal vessels, optic disc, and background, resulting in high-contrast images of the choroidal vessels that enabled subsequent binarization to acquire a dislocation map of the choroidal vessels. Central hypofluorescence on the FA images owing to blockage of excitation light by macular pigments resulted in central hyperfluorescence on the subtracted ICGA images. Nevertheless, the binarization procedure was unaffected. Densitometry was repeated to yield each average and standard deviation, which were comparable with each other. In 11 control eyes, the coefficient of variance for densitometry was 1.94% (range, 1.10%–4.47%), the coefficient of repeatability was 2.46% (range, 1.34%–6.48%), and the ICC was 0.958 (range, 0.868–0.985), suggesting excellent repeatability of the subtraction and binarization technique to acquire a distribution map of the choroidal vessels ( Table ). The intrarater agreement was also high, with an ICC of 0.961 for the entire area, 0.986 for the superior area, 0.984 for the inferior area, 0.929 for the posterior area, and 0.957 for the peripheral area. The results in eyes with CSC were equivalent to those in control eyes (mean ICC: 0.930 for the interrater agreement and 0.942 for the intrarater agreement).
| Measurement | Area | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Entire | Superior | Inferior | Posterior | Periphery | ||||||
| 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | |
| Choroidal vessel density (%) | 34.49 ± 0.86 | 34.03 ± 0.70 | 31.65 ± 1.03 | 31.10 ± 0.91 | 37.20 ± 0.98 | 36.77 ± 0.79 | 36.84 ± 1.58 | 37.18 ± 1.48 | 33.95 ± 0.69 | 34.38 ± 0.86 |
| Mean choroidal vessel density (%) | 34.26 ± 0.77 | 31.37 ± 0.97 | 36.98 ± 0.88 | 37.01 ± 1.44 | 34.17 ± 0.77 | |||||
| CV (%) | 1.12 | 1.69 | 1.34 | 4.47 | 1.10 | |||||
| CR (%) | 1.34 | 1.49 | 1.59 | 6.48 | 1.40 | |||||
| ICC | 0.980 | 0.985 | 0.979 | 0.868 | 0.978 | |||||
Impact of Age, Intraocular Pressure, and Spherical Equivalent Refractive Error on Choroidal Vessel Density
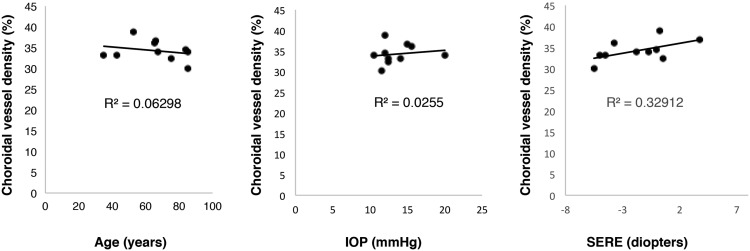
When the correlations of the choroidal vessel density with age, IOP, and SERE were assessed ( Figure 4 ), the SERE was correlated significantly (r = 0.573, P < .05, Kendall rank correlation) with the density.
Spatial Variability of the Choroidal Vessel Density in Eyes With and Without Central Serous Chorioretinopathy
In eyes without CSC, the mean choroidal vessel density was 34.26% ± 0.77% in the entire area, 37.01% ± 1.44% in the posterior area, 34.17% ± 0.77% in the periphery, 31.37% ± 0.97% in the superior area, and 36.98% ± 0.88% in the inferior area ( Figure 5 ). The densities in the macular area and inferior area were significantly ( P < .05, Bonferroni test) higher than in the superior area. All data reached significance ( P < .01, Kruskal-Wallis test).




