Purpose
To evaluate the effect of posterior vitreous detachment (PVD) on contrast sensitivity function (CSF) in previously normal eyes, with the hypothesis that PVD reduces CSF.
Design
Prospective observational case series.
Methods
At a single clinical practice 28 eyes were evaluated: 8 eyes of 8 adults (mean age 54.4 ± 10.1 years; range 39–68 years) with normal CSF documented by Freiburg Acuity Contrast Testing (Weber index: %W) who subsequently experienced PVD, as confirmed by ultrasonography and optical coherence tomography; 8 fellow eyes without PVD; and 12 control eyes: 9 eyes with PVD in patients who chose observation and 3 fellow eyes without PVD.
Results
At study entry there was no significant difference in CSF of fellow eye controls (mean 1.44 ± 0.27 %W; range 1.06–2.00 %W) and eyes that subsequently developed PVD (1.81 ± 0.61 %W; P = .146; range 1.01–2.69 %W). Following PVD there was a 52.5% reduction in CSF (2.76 ± 0.30 %W; P = .001; range 2.25–3.14 %W). CSF in the patients who chose limited vitrectomy (2.51 ± 0.46 %W; range 2.03–3.06 %W) was 41.8% worse than in the eyes with PVD of patients who chose observation (1.46 ± 0.21 %W; P = .001; range 1.08–1.87 %W). After vitrectomy, CSF improved by an average of 43.2%, normalizing in each case at 1 month (CSF 1.51 ± 0.28 %W; P = .001; range 1.14–2.00 %W), 3 months (1.38 ± 0.10 %W; P = .0002; range 1.28–1.51 %W), and 12 months (1.34 ± 0.34 %W; P = .0001; range 1.01–1.89 %W, n = 5) postoperatively, attaining the same CSF as the control fellow eyes (1.34 ± 0.20 %W; range 1.06–1.56 %W).
Conclusion
PVD is associated with significant reduction in CSF of previously normal eyes. This quantifiable negative impact on visual function can distinguish patients who are not significantly bothered by vitreous floaters from those with clinically significant symptoms.
Posterior vitreous detachment (PVD) is separation of the posterior vitreous cortex from the inner limiting membrane of the retina that results from age-related liquefaction of the vitreous gel concurrent with weakening of vitreoretinal adhesion. It was previously postulated that PVD occurs acutely, beginning posteriorly and progressing peripherally with entry of liquefied vitreous into the retrocortical (preretinal) space, leading to separation of the posterior vitreous cortex from the retina. It has recently been proposed, however, that age-related PVD begins insidiously as a localized separation of the posterior vitreous cortex from the perifoveal retina, progressing slowly over months or years until its completion at the time of vitreopapillary separation. The effects of age-related PVD are usually benign, as most patients are asymptomatic and PVD often goes clinically undetected until separation from the optic disc produces symptoms related to entopic phenomena from the posterior vitreous cortex and/or a Weiss ring. Although many patients adapt, some patients are very bothered by PVD-induced floaters, even in the absence of hemorrhage and inflammation.
Although previous studies have shown that contrast sensitivity function (CSF) is abnormal in patients with vitreous floaters, those studies compared floater patients with non-floater controls. No previous studies have prospectively documented changes in a group of individuals who served as their own controls. The following presents a prospective study of patients with previously documented normal CSF and new-onset PVD that resulted in clinically significant bothersome floaters. As a secondary outcome measure, CSF was assessed postoperatively in a subgroup of these eyes that underwent limited vitrectomy; however, surgery for vitreous opacities is not the subject of this research endeavor.
Methods
Study Design
This prospective, controlled study was performed in a single clinical practice setting. Institutional review board approval was obtained (St Joseph Health Human Research Protection Program) and approved for the prospective study of quality-of-life changes and visual function changes before and after vitrectomy for vitreous opacities. The study adhered to the principles of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. Informed consent was obtained from all subjects prior to their participation. The main outcome measure was contrast sensitivity (CSF).
Subjects
Inclusion criteria were the absence of PVD, the presence of normal CSF at study entry, and the subsequent development of PVD in only 1 eye, allowing the fellow eyes to serve as controls. During the period 2013–2015, there were 8 consecutive patients (mean age 54.4 ± 10.1 years; range 39–68 years) who met these criteria, with no history of eye disease except for myopia in 7 cases (range −1.75 to −6.75 diopters; status post laser-assisted in situ keratomileusis in 2 cases) and bilateral pseudophakia (monofocal intraocular lens) in 1 case.
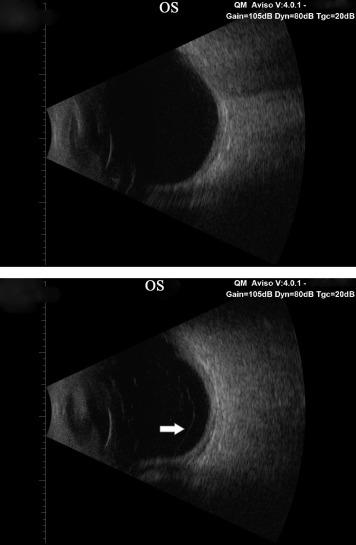
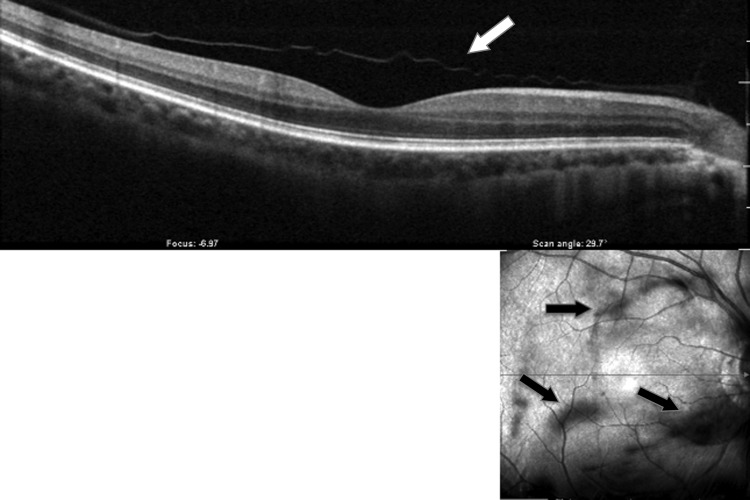
An average of 13.4 ± 7.9 (range 8–17) months later, each patient presented with the sudden onset of unilateral floaters and was found to have PVD documented by B-scan ultrasonography (AVISO; Quantel Medical, Clermont-Ferrand, France; Figure 1 ) and/or combined spectral-domain optical coherence tomography–confocal scanning laser ophthalmoscopy imaging (OCT-SLO; Optos, Marlborough, Massachusetts, USA; axial resolution of <6 μm and transverse resolution of 20 μm; Figure 2 ). Fellow eyes had no evidence of PVD, and served as controls.
Six of these subjects chose to undergo surgery (see below) and as a further comparison, the CSF measured in the 6 eyes with PVD of these 6 individuals was compared with 9 eyes with PVD in 6 patients who elected observation without surgery, since these individuals did not perceive their floaters as sufficiently bothersome. Among these 6 control subjects, 3 did not have PVD in the fellow eye, whereas 3 did have PVD in the fellow eye. For the 3 subjects with bilateral PVD, the average CSF of both eyes was calculated for statistical comparison with the eyes that underwent vitrectomy.
Vision Testing
The impact of PVD on vision was assessed objectively using best-corrected visual acuity (VA; Snellen, expressed in decimal notation) and CSF testing with the Freiburg Acuity Contrast Test (FrACT). FrACT operates on standard backlit light-emitting diode (LED) computer display monitors with luminance calibration performed prior to each evaluation. Testing was performed at 2.9 meters from the subject’s eye, level to the LED monitor, employing 24 testing trials at a spatial frequency of 5 cycles per degree, using a tumble Landolt C (sized to 20/200) in 8 different orientations. All subjects wore correction if ametropic and were dark adapted for at least 3 minutes before testing. The Weber index, defined as
is automatically calculated by the program. A higher Weber index (%W) reflects lower CSF. FrACT has previously been shown to be a reliable and accurate measure of CSF in various clinical settings, including PVD. Reproducibility of the FrACT test in our institute was previously found to be 92.1% and in the present study was determined to be 93.8% (coefficient of variance = 0.062).
Surgery
All patients were advised to attempt coping with the symptoms before considering treatment. After an average of 6.4 ± 2.1 months, 6 patients were unable to cope and underwent sutureless 25 G vitrectomy, as previously described.
Statistical Analyses
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) 22.0 (IBM, Chicago, Illinois, USA). Independent samples t tests were used to compare mean baseline parameters (VA, CSF) between control eyes and eyes with subsequent PVD. Difference in mean post-PVD CSF between the patients electing to have surgery and the nonsurgical subgroup was evaluated with an independent samples t test. Comparison of mean CSF between eyes at baseline vs post-PVD and baseline vs post-vitrectomy was performed with paired samples t tests. P values less than .05 were considered statistically significant.
Results
At study entry, all 28 eyes had normal CSF (mean 1.47 ± 0.53 %W, range 1.01–2.69 %W), as compared to previous studies. Upon initial evaluation, there were no statistically significant differences in CSF between control eyes (CSF 1.44 ± 0.27 %W; range 1.06–2.00 %W) and the eyes that subsequently developed symptomatic PVD (CSF 1.81 ± 0.61 %W, range 1.01–2.69 %W; P = .146; Table ). Further, baseline VA (Snellen decimal) was not statistically significantly different ( P = .708) between control eyes (VA 0.88 ± 0.13) and subsequently affected eyes (VA 0.86 ± 0.13).
For each subject, ultrasound determined that there was no PVD in either eye at study entry. However, an average of 13.4 ± 7.9 (range 8–17) months after study entry, 8 patients presented with the sudden onset of unilateral floaters. In each case, ultrasound documented that PVD had developed in the eye with floaters ( Figure 1 ). When the detached posterior vitreous cortex was near the retina, OCT imaging confirmed the presence of PVD ( Figure 2 ). Following PVD, CSF declined in the affected eyes by an average of 52.5%, from 1.81 ± 0.61 %W (range 1.01–2.69 %W) to 2.76 ± 0.30 %W (range 2.25–3.14 %W) ( P = .001; Table , Figure 3 ). Mean VA did not significantly change in eyes before (0.86 ± 0.13) and after (0.83 ± 0.11) PVD ( P = .685).




