8 Cutaneous Malignancies
Cutaneous Squamous Cell Carcinoma
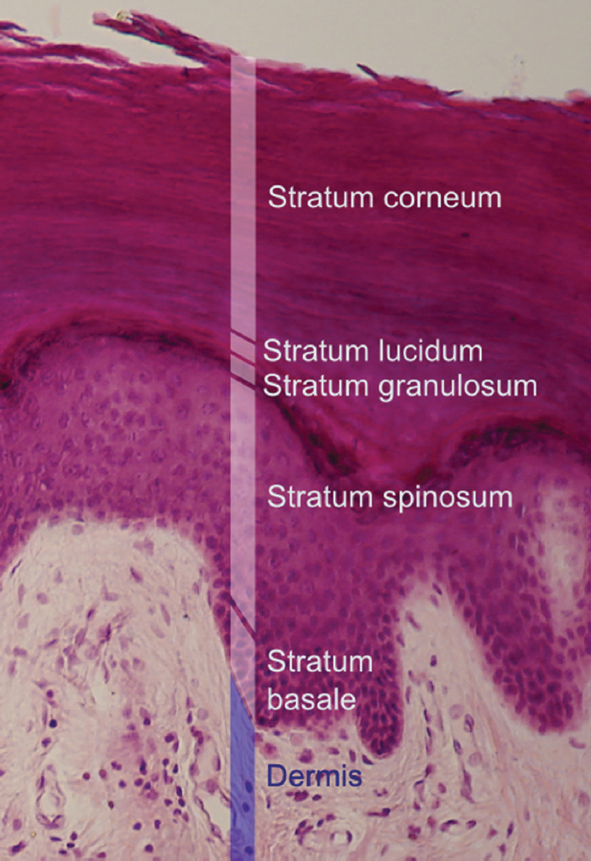
1 | What are the layers of the epidermis from superficial to deep? ( | • Stratum corneum (cornified layer) • Stratum granulosum (granular layer) • Stratum spinosum (spinous layer) • Stratum germinativum (basal layer) The dermis is immediately deep to this. |
Fig. 8.1 Histological section with H&E stain of the epidermis showing the five strata, from superficial to deep: corneum, lucidum, granulosum, spinosum and basale. (Used with permission from Gantwerker EA, Hom DB. Principles to minimize scars. Facial Plastic Surg. 2012 Oct;28(5):473-486.)
2 | Name the four cell types of the epidermis. | • Keratinocytes (80%) • Merkel cells (mechanoreceptors) • Langerhans cells (antigen processing and presenting cells • Melanocytes (pigmented dendritic cells) |
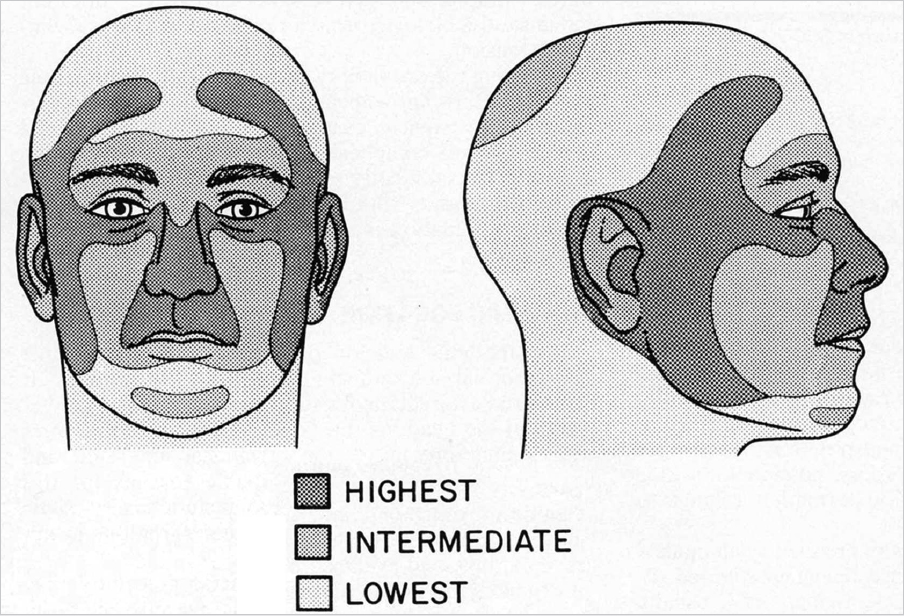
What is the “H-zone” of the head and neck? ( | This area extends vertically from the angle of the mandible through the ear and preauricular region to the temple and is connected horizontally through the periorbital skin, nasal skin, and upper lip. |
Fig. 8.2 “H-zone” of the face where squamous cell carcinoma and basal cell carcinoma potentially demonstrate a more aggressive course. (Used with permission from Donald PJ, ed. The Difficult Case in Head and Neck Cancer Surgery. New York, NY: Thieme; 2010.)
4 | Which skin cancer type is most common on the lower lip? | Squamous cell carcinoma |
5 | What risk factors are associated with lymphatic metastasis of cutaneous squamous cell carcinoma? | • Area > 20 mm (less in the H-zone) • Recurrent tumors • Site of prior radiation or scar • Rapidly growing tumor • Perineural invasion • Poorly differentiated tumors, high-grade tumors • Depth > 5 mm or subcutaneous fat • Lymphovascular invasion • Immunosuppression |
6 | Metastasis from cutaneous head and neck squamous cell carcinoma most commonly occurs in which lymphatics? | About 75% of cutaneous lymphatic metastases occur in the parotid bed; 40% occur in level II. |
7 | What are risk factors for cutaneous squamous cell carcinoma of the head and neck? | • Ultraviolet radiation is the number 1 risk factor • Light skin pigmentation • Ionizing radiation • Immunosuppression • Exposure to coal tar, asphalt, and arsenic consumption • Xeroderma pigmentosa, basal cell nevus syndrome • Tendency to burn or freckle (rather than tan) • Male sex |
8 | Describe the Fitzpatrick scale. | Classification schema for the color of skin. Associated with decreasing risk of cutaneous malignancy: • Type I: Pale white, blond, or red hair; blue eyes; always burns, never tans; freckles • Type II: White, fair, blond or red hair; blue, green, or hazel eyes; tans minimally, often burns • Type III: Fair skin; any hair and eye color; tans evenly, sometimes burns. • Type IV: Mediterranean skin, rarely burns, tans easily • Type V: Dark brown skin, rarely burns, tans easily • Type VI: Dark brown to black, never burns, tans very easily |
9 | What are the risk factors for development of solar keratosis, how many of these eventually undergo malignant transformation, and what percentage of squamous cell carcinomas can be traced to actinic keratosis? | Sun exposure is the most important risk factor, but immune suppression is also important (immune-suppressed individuals are 250 times more likely to develop solar keratoses). Fewer than 1/1,000 solar keratoses will go on to become squamous cell carcinoma; 60% of squamous cell carcinomas can be traced back to solar keratoses. |
10 | What is Marjolin ulcer? | Marjolin ulcer is a term used to describe an ulcerative squamous cell carcinoma at the site of prior trauma, inflammation, or scarring such as radiation or a burn. |
11 | What percentage of nonmelanoma cutaneous malignancies are made up of squamous cell carcinoma? | 20% |
12 | Which pathologic finding in squamous cell carcinoma is associated with the highest recurrence rate and regional metastasis? | Perineural invasion. This is associated with metastasis in 47% of patients. |
13 | How many solar keratoses eventually undergo malignant transformation? | Fewer than 1 in 1,000 solar keratoses will become squamous cell carcinoma. |
14 | What percentage of squamous cell carcinomas can be traced to actinic keratosis? | 60% |
15 | Describe the clinical and pathological characteristics of Bowen disease. | Bowen disease is an intraepidermal squamous cell carcinoma that manifests as an enlarging, well-demarcated erythematous plaque with surface crusting. Histologically, it resembles squamous cell carcinoma with atypical keratinocytes replacing epidermis. It appears more commonly in women (70 to 85%) and in the sixth or seventh decades of life. It can appear anywhere, but it is more common in the lower legs. The cause has been traced to sun exposure, arsenic, immune suppression, and viral infection. Treatment is most often provided with cryotherapy, curettage, excision, laser, photodynamic therapy and topical 5-fluorouracil (5-FU), with no treatment showing a clear superior effect. |
16 | What type of skin cancer is known for rapid progression of a swelling, dome-shaped lesion that eventually resolves by sloughing off and scarring? | Keratoacanthoma |
17 | Your patient, a 67-year-old farmer, has a rapidly expanding, symmetric, dome-shaped lesion on his neck. The lesion is surrounded by smooth, inflamed skin, but it has a central crater containing keratinous debris. What is the most likely diagnosis? | Keratoacanthoma |
18 | Describe the typical manifestation of a keratoacanthoma. | Keratoacanthomas are rapidly growing lesions that may then slowly spontaneously involute after a plateau phase. |
Describe the typical manifestation of cutaneous squamous cell carcinoma. | Cutaneous squamous cell carcinoma can present in a number of ways: A thick, scaly patch, an ulcerated patch with rolled borders, a nodular lesion, or scale with pigmentation | |
20 | What symptoms should be elicited in an history of present illness for a patient with newly diagnosed cutaneous squamous cell carcinoma? | Symptoms of advanced disease: numbness, pain, weakness or other perineural symptoms; weight loss, bone pain, shortness of breath to suggest distant disease; rapid growth, bleeding, fixation, neck mass to suggest locally advanced or aggressive disease |
21 | What features of cutaneous squamous cell carcinoma merit radiologic workup? | • Locally advanced disease: Fixation, numbness, weakness, pain or trismus, extensive lesions (> 2 cm), or perineural or lymphovascular invasion • Regionally advanced disease: Palpable lymphadenopathy, intransit metastasis • Distant metastasis risk: Axillary adenopathy, bone pain, shortness of breath, unexplained weight loss, unexplained neurologic symptoms • High-risk patients: Recurrent lesions, immunosuppression, history of radiation |
22 | What is the most appropriate biopsy technique for deep ulcerated lesions of the skin of the head and neck? | • Punch of incisional biopsy at the thickest portion of the lesion • Full-thickness biopsy should be attempted and should involve the reticular dermis or subcutaneous fat when possible. |
23 | What features of head and neck nonmelanoma skin cancer are associated with American Joint Committee on Cancer (AJCC) T2 tumors? | Greater than 2 cm greatest dimension or Two or more high-risk features: • > 2-mm invasion • Clark level ≥ IV • Perineural invasion • Primary site ear • Primary site non-hairbearing lip • Poorly or undifferentiated tumor Note: Excludes cutaneous squamous cell carcinoma of the eyelid |
24 | What features of head and neck nonmelanoma skin cancer are associated with T3 and T4 tumors (AJCC seventh edition)? | • T3: Invasion of the maxilla, mandible, orbit, or temporal bone • T4: Perineural invasion of the skull base |
25 | What are the high-risk features of head and neck cutaneous squamous cell carcinoma? | Deep lesions (< 2 mm, Clark level IV) • Perineural invasion • H-zone lesions • Recurrent lesions Lesions arising in radiated fields or scar • Size > 1.5 cm • Poorly differentiated lesions • Immunosuppression |
26 | What locations of head and neck cutaneous squamous cell carcinoma are more likely to exhibit recurrence and why? | High-risk sites for recurrence include the so-called H-zone along the preauricular and postauricular areas as well as across the midface, including the nose. This has been attributed to these sites being the location of embryologic fusion, affording tumors planes that provide avenues for spread. |
27 | True or False: Pathologic involvement of neck nodes with metastatic cutaneous squamous cell carcinoma is associated with worse survival in patients who also have parotid metastasis. | True. Andruchow et al 2006 |
28 | What are appropriate margins for low-risk cutaneous squamous cell carcinoma? | 4- to 6-mm clinical margins. |
Although not yet approved by the Food and Drug Administration (FDA), imiquimod has shown some promise of utility for the treatment of cutaneous squamous cell carcinoma. What is the mechanism of action for imiquimod? | Imiquimod is a local immune response modifier that induces activity of interferon-α and other cytokines. | |
30 | Describe the technique for electrodessication and curettage (EDC) used in cutaneous squamous cell carcinoma and basal cell carcinoma. | In EDC, a curette is used to scrape tumor off down to the dermis, following which an electrodessication is performed to denature any cells along the surface. This is repeated until a satisfactory depth of excision is reached. |
31 | When is Mohs surgery indicated for cutaneous squamous cell carcinoma of the head and neck? | • Anatomically or aesthetically sensitive areas where wide margins are not achievable (periorbital, nasal, periauricular and auricular, and perioral) • Positive margins after wide local excision and potential extension into an area fulfilling the first criteria |
32 | When is radiation indicated for cutaneous squamous cell carcinoma? | • Nonoperative candidates (surgical risk or unresectable) • Positive margins or incomplete excision • Solitary node ≥ 3 cm or with extracapsular extension • Multiple positive nodes • Multiple recurrent disease despite appropriate treatment • Perineural invasion of major (named) nerve or extensive perineural invasion • T4 disease |
33 | What is the appropriate treatment of keratoacanthoma? | • Wide local excision is preferred • Intralesional methotrexate, steroids, and 5-FU can be used for nonoperative cases. |
Basal Cell Carcinoma
34 | What proportion of basal cell carcinomas occur on the head and neck? | Four in five cutaneous basal cell carcinomas |
35 | Is upper lip cancer more common in men or women? | It is more common in women: 21% of lip cancers on the upper lip versus only 3% of lip cancer in men. |
36 | What percentage of cutaneous malignancies occur on the lower lip? | 90% |
37 | What is the significance of basal cell carcinoma found in the folds of the face? | These tumors develop at the site of embryonic fusion plates, resulting in more likely recurrence and higher risk of spread. They therefore require close follow-up. |
38 | Is basal cell carcinoma more likely on the upper or lower lip? | Upper lip (13% vs. 1% of lower lip cancers) |
39 | What is the likelihood of regional nodal metastasis in basal cell carcinoma? | Nodal spread is rare, occurring in fewer than 0.0028 to 0.5% of patients. |
40 |