Craniopharyngiomas are rare epithelial tumors arising along the path of the craniopharyngeal duct; therefore, they occur in the sellar or suprasellar regions. These tumors commonly lead to neurologic, endocrinological, or visual symptoms. Radical surgery is the treatment of choice in craniopharyngiomas. The transnasal/transsphenoidal endoscopic approach offers the possibility of removing the tumor without retracting brain and optic pathways, with good results. The rate of cerebrospinal fluid fistula has improved due to the use of vascularized mucosal flaps for cranial base reconstruction.
| EBM Question | Level of Evidence | Grade of Recommendation |
|---|---|---|
| Is morbidity decreased in patients with endoscopic resection of craniopharyngiomas (vision, pituitary function) compared to microscopic/trans-cranial surgery? | 4 | C |
Craniopharyngiomas are rare epithelial-squamous, extra-axial tumors arising along the path of the craniopharyngeal duct, with slow-growing characteristic. Two hypotheses explain the origin of craniopharyngioma—embryogenetic and metaplastic; they complement each other and explain the craniopharyngioma spectrum.
Epidemiology
The overall incidence of craniopharyngioma is approximately 0.5 to 2 per 100,000 per year. The Central Brain Tumor Registry of the United States revealed an average of 338 cases diagnosed annually, with 96 occurring in children aged 0 to 4 years in this country. No variance by gender or race was found. The age distribution is bimodal with a peak in childhood and a second peak among middle-aged and older adults. No definite genetic relationship has been found and few familial cases reported.
Pathophysiology
There are 2 hypotheses to justify the craniopharyngioma spectrum: embryogenetic (neoplastic transformation of embryonic squamous cell rests of the involuted craniopharyngeal duct) and metaplastic (metaplasia of adenohypophyseal cells in the pituitary stalk or gland).
Designated as World Health Organization grade I tumors, comprising 2% to 5% of all central nervous system tumors, craniopharyngiomas can be classified in 2 histologic subtypes: adamantinomatous and papillary. The adamantinomatous type may be encountered at any age but predominantly in the first 2 decades of life. The papillary variety has been primarily reported in adults. Some investigators report a lower recurrence rate with the papillary variety, whereas others have found no difference in surgical outcome or recurrence between the 2 subtypes.
Craniopharyngiomas are dysontogenic tumors with benign histology and malignant behavior with infiltrative tendency into critical parasellar structures, such as optic apparatus, pituitary stalk and gland, floor of the third ventricle, hypothalamus, and cerebral vasculature of the circle of Willis, and recur after what was thought to be total resection.
The tumor characteristics are solid (with or without calcification) and cystic. The cyst is filled with a turbid, proteinaceous material of brownish-yellow color that glitters and sparkles because of a high content of floating cholesterol crystals. Because of its appearance, it has been compared with machinery oil.
It occur most often in sellar/suprasellar region but can have anterior extension to the prechiasmatic cistern and subfrontal spaces; posterior extension into the prepontine and interpeduncular cisterns, cerebellopontine angle, third ventricle, posterior fossa, and foramen magnum; and laterally toward the subtemporal spaces. They can even reach the sylvian fissure.
Craniopharyngiomas are supplied with blood coming from the anterior circulation: perforators from anterior cerebral artery and the proximal portion of the posterior communicating artery.
Tumor adhesion is the result of local inflammation. Several inflammatory cytokines have been shown to be elevated in the craniopharyngioma cyst fluid compared with cerbrospinal fluid (CSF).
Clinical
Craniopharyngiomas are highly complex benign tumors and they have variable clinical presentation, the severity of which depends on the location, size, and growth potential of the tumor. Neurologic symptoms may include headaches, nausea, and vomiting. Childhood populations can present, more commonly than adults, hydrocephalus in 41% to 54% of cases. Because of the proximity to the optic chiasm, visual field defects usually present as bitemporal hemianopia, reported in as many as 49% of cases.
Pituitary symptoms are associated with growth failure and delayed puberty (in children) and hypogonadism in adults. Rates for pituitary hormone deficits include 35% to 95% for growth hormone, 38% to 82% for follicle-stimulating hormone/luteinizing hormone, 21% to 62% for corticotropin (eg, orthostatic hypotension, hypoglycemia, hyperkalemia, cardiac arrhythmias, lethargy, confusion, anorexia, nausea, and vomiting), 21% to 42% for thyroid-stimulating hormone (eg, weight gain, fatigue, cold intolerance, and constipation), and 6% to 38% for antidiuretic hormone.
Three major clinical syndromes have been described and relate to the anatomic location of the craniopharyngioma: a prechiasmal localization typically results in associated findings of optic atrophy (eg, progressive decline of visual acuity and constriction of visual fields); a retrochiasmal location commonly is associated with hydrocephalus, with signs of increased intracranial pressure (eg, papilledema and horizontal double vision); and intrasellar craniopharyngioma usually manifests with headache and endocrinopathy.
Investigation
The diagnostic evaluation for craniopharyngioma includes precontrast and postcontrast CT scans and MRI and, occasionally, cerebral angiography in addition to complete endocrinologic evaluation (baseline serum electrolytes, serum and urine osmolality, thyroid studies, and morning and evening cortisol levels, growth hormone levels, and luteinizing hormone and follicle-stimulating hormone levels, in adolescent and adult patients) and neuro-ophthalmologic evaluation with formal visual field documentation as well as neuropsychological assessment.
Imaging studies strongly suggest the diagnosis: on plain skull radiograph, tumor calcifications can be observed and may also show an abnormal sella (widening of its outlet, uniform expansion, and shortening or erosion of the dorsum sellae).
CT is the ideal modality for the evaluation of the bony anatomy and detection of calcifications of the tumor. MRI is particularly useful for the topographic and structural analysis of the tumor and is the most important imaging modality used to plan the surgical approach, showing the relationship between the tumor and the vascular structures and the optic apparatus.
Management
Surgical excision, with or without adjuvant conventional external beam irradiation, is the primary option to treatment of craniopharyngiomas. Complete resection remains the goal of primary surgery; however, even with the advent of modern surgical techniques, this may not be warranted if it is associated with significant morbidity.
Matson and Crigler, in 1969, postulated that “recurrence of symptoms has been so relentless and rapid in such a high percentage of cases if the tumor is not radically removed, that our conviction becomes steadily stronger that optimum treatment consists in making every effort to affect total excision at the first operation.” Total excision must be attempted at the first operation.
The classical operative technique for craniopharyngioma resection is based on various craniotomy approaches (pterional, bifrontal, and interhemispheric); the transsphenoidal route has always been reserved for resection of purely intrasellar masses. In the 1990s, some investigators began recommending the use of extended transsphenoidal approaches for sellar and suprasellar tumors. Due to the difficulty of visualizing structures of interest and the risk of CSF leak, however, this method did not gain wider acceptance. With the evolution of endoscopic surgery and the possibility of improved visualization, several investigators have since reintroduced the extended transsphenoidal approach as an option for resection of intrasellar and suprasellar craniopharyngiomas, with outcomes similar to those provided by traditional approaches. The lower incidence of CSF leak made possible by the use of vascularized flaps played a decisive role in expanding indications for this approach. In light of the complexity of craniopharyngiomas as a disease entity, any method that may increase the possibility of total resection and minimize operative mortality warrants consideration.
Since the work of Wang and colleagues, craniopharyngiomas were defined as midline lesions arising along the pituitary stalk and were classified by level of origin as infradiaphragmatic or supradiaphragmatic. Postsurgical outcomes in patients with supradiaphragmatic craniopharyngiomas are markedly worse than those achieved in patients with infradiaphragmatic tumors.
Prognosis
The definition of gross total removal (GTR) is the neurosurgeon’s intraoperative impression confirmed by the objective measure of a 3-months’ postoperative MRI. Approximately 10% of totally resected craniopharyngiomas recur and the extent of resection is the most significant predictor for recurrence.
Fahlbusch and colleagues showed 86.9% of recurrence-free survival at 5 years and 81.3% at 10 years. In contrast, the rate of recurrence-free survival was 48.8% for subtotal removal (STR) (ie, minor residual tumor) and only 15.6% for partial removal at 10 years of follow-up.
The Sao Paulo experience
After obtaining institutional review board approval, the authors included 18 patients treated with a purely endoscopic approach to craniopharyngiomas, confirmed with histopathological diagnosis.
All patients underwent MRI and CT to classify the tumor. The vertical extension and position relative to the optic chiasm were analyzed. Neurologic, endocrinological and ophthalmologic evaluations, including formal visual field testing, were performed in patients before and after surgery.
The degree of resection was determined by a combination of the intraoperative assessment and 3-month postoperative MRI studies. Resections were considered GTR only if the surgical impression and MRI assessment revealed no residual tumor. Resections were categorized as near total removal (NTR) if more than 95% of the tumor was removed. An STR was considered when more than 70% of the tumor was resected. Finally, a partial resection was indicated when more than 50% of the tumor remained.
Surgery
In the majority of cases, a modified transseptal/transnasal binostril technique was used (described by Stamm).
After topical vasoconstriction with adrenalin applied on cottonoids, local infiltration of the nasal septum mucosa is performed with lidocaine with adrenaline 1:100,000. A nasal septal hemitransfixion incision is performed unilaterally, usually on the right side. The posterior part of the bony septum is removed, leaving the inferior portion as a midline landmark and the sphenoid face exposed. A nasoseptal flap is created on the contralateral side to the hemitransfixion incision. The superior horizontal incision is made 1 cm below the superior aspect of the nasal septum and continued posteriorly across the sphenoid face at the level of the inferior aspect of the sphenoid ostium. The inferior horizontal incision is performed 0.5 cm above the level of the floor of the nose or laterally in the inferior meatus of a larger flap is required. The position of the anterior incision depends on the length required and may be as far forward as the mucocutaneous junction.
After flap harvest, it is placed into the nasopharynx or maxillary sinus until the extirpate phase of the surgery is complete ( Fig. 1 ).
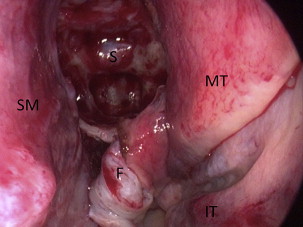
The approach is expanded as required by removal of middle and superior turbinates and opening of the maxillary and ethmoid sinus; in cases requiring bilateral exposure anterior to the sphenoid face, partial septectomy is performed.
Commencing at the sphenoid ostium, the maximum amount of the front wall is then removed.
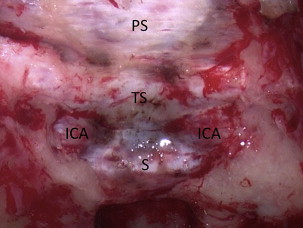
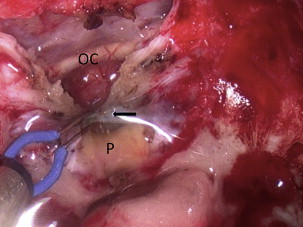
The mucosa of the posterior sphenoid wall is then displaced laterally. Drilling of the thick tuberculum sellae bone and the sella is then performed. An area the entire intercarotid width is thinned down to eggshell thickness with a high-speed drill and then removed. A Kerrison rongeur may be used for additional bone removal. Bone removal much wider and higher than the area exposed in standard pituitary surgery. Bone removal continues along the sphenoid planum ( Fig. 2 ). The superior intercavernous sinus is then coagulated with help of a bipolar cautery ( Fig. 3 ). The dura is opened above and below the superior intercavernous sinus, exposing the sellar and suprasellar region.
The intradural resection is performed at first with a debulking of the tumor. Modified transseptal/transnasal binostril approach allows 4 hands; extracapsular sharp dissection and countertraction using gentle suction form the foundation of the endoscopic surgery as they did when microsurgery was performed.
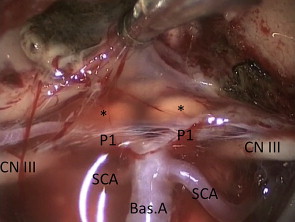
A final inspection is done with a 0° and/or 45° endoscope to identify all the structures, such as pituitary stalk, optic nerves and chiasm, and other cranial nerves and vessels ( Fig. 4 ).
Reconstruction
A reliable skull base reconstruction is mandatory at the end of the procedure because of the large dural opening, extensive dissection of arachnoid cisterns and/or third ventricle, and associated CSF leak.
In the beginning of the sao paulo experience, some multilayer free grafts, including fascia lata, fat, and DuraGen (Integra LifeSciences Corp), were used.
At the end of these cases, the authors prefer the triple-F reconstruction (fat, fascia, and flap), with free fat grafts used to fill dead space and form a buttress for a fascia lata inlay graft and, finally, covered with the pedicled nasosseptal flap.
Spongostan powder (Ethicon, NJ, USA) and Gelfoam TM (Pfizer, NY, USA) are layered directly over the flap, followed by gauze packing. The packing is supported by a RapidRhino 900 (Arthrocare, Austin, TX, USA) or similar pack.
Postoperative care
Antibiotics are used perioperatively and continued postoperatively while nasal packing remains in situ. Packing is left in place for 5 to 7 days. The onset of diabetes insipidus (DI) is monitored with serum and urine sodium/osmolality measurements. Patients are confined to bed for 48 hours, have 30° head elevation, and avoid straining, Valsalva maneuvers, and nose blowing. Lumbar drains are not routinely used unless there is an additional comorbidity, such as raised intracranial hypertension or prior radiotherapy.
Discharge usually occurs 3 to 5 days postoperatively.
Follow-up
An MRI is performed at 3 months as a baseline study. This is important, because postsurgical MRI signaling is often difficult to interpret. Endocrine assessment is performed routinely in follow-up; however, ophthalmologic evaluation is undertaken only if clinically indicated. The long-term follow-up is multidisciplinary but an endocrinologist is the central team member who coordinates ongoing care.
Results
No patient of the 18 was excluded or lost in follow-up ( Table 1 ). There were 11 men and 7 women. Patients’ ages ranged from 6 to 72 years (mean age 29.4 years). Seven patients (39%) were under 16 years old, classified as child/young, and 11 (61%) were adults (see Table 1 ).
| Case | Sex | Age (Years) | Clinical Presentation | Previous Treatment | ||
|---|---|---|---|---|---|---|
| Anterior Pituitary Function | Posterior Pituitary Function | Visual Function | ||||
| 1 | M | 8 | Growth failure | Normal | Normal | None |
| 2 | M | 15 | Panhypopituitarism | DI | Normal | None |
| 3 | M | 34 | Normal | Normal | Visual loss | None |
| 4 | F | 26 | Normal | Normal | Visual loss | None |
| 5 | F | 7 | Normal | DI | Visual loss | None |
| 6 | M | 36 | Panhypopituitarism | Normal | Visual loss | None |
| 7 | M | 16 | Panhypopituitarism | DI | Visual loss | 1 VP shunt, 3 neuroendoscopies, and 2 craniotomies |
| 8 | F | 20 | Panhypopituitarism | DI | Visual loss | 3 Craniotomy and 3 radiosurgeries |
| 9 | M | 69 | Normal | Normal | Visual loss | None |
| 10 | M | 24 | Normal | Normal | Visual loss | None |
| 11 | F | 72 | Normal | Normal | Visual loss | None |
| 12 | M | 48 | Normal | Normal | Visual loss | None |
| 13 | M | 29 | Hypogonadism | Normal | Visual loss | None |
| 14 | F | 42 | Normal | Normal | Visual loss | None |
| 15 | M | 09 | Growth failure | Normal | Visual loss | None |
| 16 | F | 06 | Growth failure | Normal | Visual loss | None |
| 17 | F | 12 | Growth failure Hypothyroidism | Normal | Normal | None |
| 18 | M | 56 | Hypogonadism | Normal | Normal | None |
| Others: cognitive deficits/Somnolence | ||||||
Two patients (11%) had undergone previous surgery: one had 3 neuroendoscopic procedures, 2 craniotomies and 1 ventricular shunt and the other one had 6 previous procedures: 3 prior craniotomies and 3 radiosurgery.
Clinical presentation
The main symptom presented by patients, visual loss, was observed in 14 of 18 patients (78%). Four of these patients (22%) suffered from panhypopituitarism (anterior gland). Three of these 4 patients had DI associated and 1 patient had isolated posterior pituitary function impaired with DI. Two patients (11%) presented with hypogonadism.
Growth failure with somatotrophin deficiency (low insulinlike growth factor 1 levels) was presented alone as first endocrinology presentation in 3 patients. One patient had growth failure and hypothyroidism associated.
In the child/young group, the rate of growth failure with or without other pituitary dysfunction was 85.7% (6 of 7 patients).
One patient was diagnosed in investigation of cognitive deficits with somnolence.
Visual outcomes
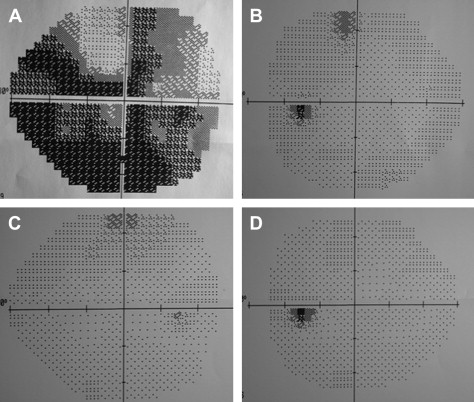
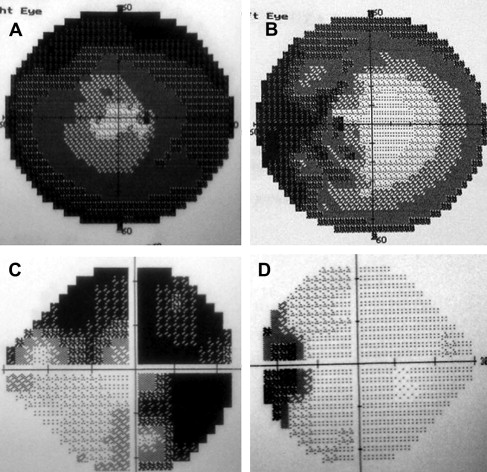
Before and after surgery, the patients underwent an ophthalmologic examination, including visual field examination.
Of the 14 patients with preoperative visual deficits, 12 had their vision normalized ( Fig. 5 ) or improved ( Fig. 6 ), showing a substantial improvement of visual defect rate of 85.7%. One patient’s deficit remained stable and another patient had his right vision improved but showed no changes in the left eye ( Table 2 ).
| Case | Sex | Preoperative Visual Function | Postoperative Visual Result |
|---|---|---|---|
| 1 | M | Normal | Remained normal |
| 2 | M | Normal | Remained normal |
| 3 | M | Visual loss | Improved |
| 4 | F | Visual loss | Improved |
| 5 | F | Visual loss | Improved right eye |
| 6 | M | Visual loss | No improved |
| 7 | M | Visual loss | Improved |
| 8 | F | Visual loss | Improved |
| 9 | M | Visual loss | Improved |
| 10 | M | Visual loss | Improved |
| 11 | F | Visual loss | Improved |
| 12 | M | Visual loss | Improved |
| 13 | M | Visual loss | Improved |
| 14 | F | Visual loss | Improved |
| 15 | M | Visual loss | Improved |
| 16 | F | Visual loss | Improved |
| 17 | F | Normal | Remained normal |
| 18 | M | Normal | Decreased |
Of the 4 patients without preoperative visual deficits, the conditions of 3 patients were unchanged postoperatively, but 1 patient had visual worsening.
Endocrine outcomes
Only 1 of the 4 patients who had preoperative DI improved (case 2), whereas the other 3 remained with deficit ( Table 3 ). Nine of the 14 (64%) patients who had normal preoperative function of posterior pituitary experienced new persistent DI after surgery.
| Case | Anterior Pituitary Function | Posterior Pituitary Function | ||
|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | |
| 1 | Growth failure | Hypothyroidism growth failure | Normal | Normal |
| 2 | Panhypopituitarism | Panhypopituitarism | DI | Improved |
| 3 | Normal | Normal | Normal | Normal |
| 4 | Normal | Normal | Normal | Normal |
| 5 | Normal | Normal | DI | DI |
| 6 | Panhypopituitarism | Panhypopituitarism | Normal | New DI |
| 7 | Panhypopituitarism | Panhypopituitarism | DI | DI |
| 8 | Panhypopituitarism | Panhypopituitarism | DI | DI |
| 9 | Normal | Normal | Normal | New DI |
| 10 | Normal | Normal | Normal | New DI |
| 11 | Normal | Panhypopituitarism | Normal | New DI |
| 12 | Normal | Normal | Normal | Normal |
| 13 | Hypogonadism | Panhypopituitarism | Normal | Normal |
| 14 | Normal | Panhypopituitarism | Normal | New DI |
| 15 | Growth failure | Panhypopituitarism | Normal | New DI |
| 16 | Growth failure | Panhypopituitarism | Normal | New DI |
| 17 | Growth failure Hypothyroidism | Panhypopituitarism | Normal | New DI |
| 18 | Hypogonadism | Panhypopituitarism | Normal | New DI |
None of the 4 patients who had panhypopituitarism improved this condition postoperatively. Of the 14 patients without preoperative panhypopituitarism, 7 (50%) developed panhypopituitarism after the surgery. One patient who had preoperative growth failure experienced the maintenance of this deficit and a new hypothyroidism (case 1). The normalization of an anterior pituitary deficiency after surgery occurred in none of the patients.
Tumor location, surgical approach, and reconstruction
The authors classify tumors based on the location according to the sellar diaphragm as subdiaphragmatic or supradiaphragmatic. The subdiaphragmatic tumors are classified as sellar and/or suprasellar depending on its vertical extension. The supradiaphragmatic are classified as prechiasmatic or postchiasmatic, with or without intraventricular extension.
Five tumors had subdiaphragmatic origin; 4 of these had sellar and suprasselar presentation, and 1 was confined to the sella. In all these cases, the authors used a transsellar approach without the opening of the planum sphenoidale ( Table 4 ).



