Purpose
To evaluate scleral pneumatonometry as an alternative method for measuring intraocular pressure (IOP).
Design
Prospective cross-sectional study.
Methods
Adult subjects with healthy eyes were recruited from the Comprehensive Eye Service at the University of Illinois Eye and Ear Infirmary from August 2008 through February 2009. Study measurements included corneal pneumatonometry (IOPk), scleral pneumatonometry (IOPs), axial length (AL), spherical equivalent (SE), and central corneal thickness (CCT). Main outcome measures were scleral IOP and corneal IOP.
Results
Analysis included a monocular data set from single eyes of 97 subjects (age: 18-82 years). IOPs was consistently higher than IOPk, and correlated positively with IOPk (r = 0.57, P < .0001), age (r = 0.51, P < .0001), and SE (r = 0.32, P = .0002). The difference between scleral and corneal IOP (IOPs − IOPk) correlated positively with IOPs (r = 0.89, P < .0001), age (r = 0.57, P < .0001), and SE (r = 0.34, P < 0.0001). Bland-Altman analysis for agreement between scleral and corneal pneumatonometry measurements showed a mean difference of 8.08 mm Hg, with the 95% limit of agreement between -3.47 and 19.64 mm Hg. Regression analysis yielded the following equation: IOPk = 11.9 + 0.32(IOPs) − 0.05(Age).
Conclusions
Scleral pneumatonometry correlates positively with corneal pneumatonometry and is more accurate at lower values and in younger patients. When adjusted for age, scleral pneumatonometry may be an adequate alternative in situations where corneal measurements are impractical.
Obtaining accurate intraocular pressure (IOP) measurements in patients with prosthetic corneas is an ophthalmologic challenge that is yet to be solved. This is especially important for, but not limited to, patients with pre-existing ocular hypertension or glaucoma. Various alternatives, including tactile estimation, have been suggested, but these require the use of special implants and/or measuring techniques that are not practical in the office setting. Additionally, various disease states, including acromegaly, corneal edema, and keratoconus, produce surface and/or thickness irregularities that undermine the accuracy of IOP measurements.
Presently, corneal pneumatonometry is an acceptable alternative when dealing with diseased or irregular corneas, where mire distortion precludes the accuracy of Goldmann applanation tonometry (GAT). In patients with prosthetic corneas, both GAT and corneal pneumatonometry are impractical, and many physicians resort to tactile estimation in this setting. Instruments such as the Tono-Pen and vibration tonometer have been tested on the sclera, but their accuracy is either poor or unknown. The design of the Goldmann applanation tonometer and dynamic contour tonometer (DCT) largely precludes their use on the sclera.
Interestingly, when the pneumatonometer was first introduced to the ophthalmologic community, it was described on the sclera, where it was shown to correlate well with corneal GAT and Schiotz measurements. Despite this report, we are unaware of any subsequent studies in the current literature that compared scleral and corneal pneumatonometry, provided guidelines for scleral pneumatonometry, or assessed factors that would influence this technique.
Given its original description on the sclera, scleral pneumatonometry represents a potential alternative means of measuring IOP in eyes with abnormal corneas. In an effort to better characterize this approach, we designed this study to compare scleral pneumatonometry with corneal pneumatonometry in adult subjects with healthy eyes.
Methods
This prospective cross-sectional study with patient informed consent to participate in research was reviewed and approved by the Institutional Review Board at the University of Illinois, Chicago. This study was performed in accordance with HIPAA regulations.
All study subjects were recruited from the Comprehensive Eye Service at the University of Illinois Eye and Ear Infirmary during the period ranging from August 2008 through February 2009. All eligible participants were informed of the study and its anticipated benefits along with any risks associated with participation in the study. Only those individuals who were willing to proceed were asked to sign their informed consent and enrolled as study subjects. All measurements were carried out by a single investigator (M.A.K.).
All subjects were 18 years of age or older. The exclusion criteria included any history of corneal disease, uveitis, ocular trauma, ocular surgery, and/or collagen-vascular disease. In order to maintain the accuracy of our corneal pneumatonometry measurements, we also excluded eyes with myopia greater than 6 diopters, hyperopia greater than 3 diopters, or astigmatism greater than 3 diopters. We excluded eyes with a history of vitrectomy, cryotherapy, scleral buckle surgery, treatment with miotic agents, or age-related macular degeneration, because there have been several reports of altered scleral rigidity in these eyes. For the same reason, history of scleritis or any evidence of scleral thinning on slit-lamp examination also warranted exclusion from this study.
The manifest refraction was measured using a phoropter. Each eye was anesthetized with 1 drop of 1% proparacaine. One central corneal pneumatonometry (IOPk) reading and 3 inferotemporal scleral pneumatonometry (IOPs) readings were obtained for each eligible eye by using a pneumatonometer (Mentor 30 Classic pneumatonometer; Mentor Inc, Norwell, Massachusetts, USA). These measurements had a standard deviation (SD) of <0.5. All measurements were taken 2 mm posterior to the surgical limbus. Because serial IOP measurements can theoretically lower IOP, we waited 1 minute between successive attempts.
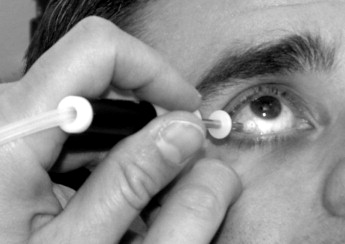
For obtaining scleral pneumatonometry measurements, the subjects were asked to tilt their heads back approximately 45 degrees while maintaining their eyes in primary position to minimize any influence of the extraocular muscles on IOP. Additionally, the body (torso) was kept in the upright, seated position to avoid any effects of body position on IOP. The pneumatonometer tip was then maintained as close as possible to the horizontal position, and its superior edge was applied 2 mm posterior to the limbus in the inferotemporal scleral quadrant ( Figure 1 ).
After the IOP measurements were completed, 3 central corneal thickness (CCT) measurements (Compuscan P Ultrasound Pachymeter; Storz Inc, St. Louis, Missouri, USA) and 5 A-scan axial length (AL) measurements with SD of <0.2 (Accutone/Advent A/B Scan; Accutone Inc, Maller, Pennsylvania, USA) were obtained.
Statistical Analysis
Pearson correlation coefficients were computed to describe the strength of the linear relationship between corneal and scleral IOP measurements. An r value of >0.5 indicated moderate significance. Simple linear regression analyses were performed using scleral IOP as an outcome with demographic, corneal, and anterior segment parameters. A P value of ≤.01 was considered statistically significant.
An assessment of Bland-Altman agreement was used to compare corneal and scleral pneumatonometry measurements. A range of agreement was defined as mean ±2 SD. All analyses were performed using SAS (SAS institute Inc, Cary, North Carolina, USA) and Microsoft Excel 2007 (Microsoft Corporation, Bellevue, Washington, USA) software.
Results
Measurements were obtained on a total of 131 eyes (70 right eyes and 61 left eyes) of 97 subjects with a mean age of 54.4 ± 17.7 years. The study population comprised 97 healthy subjects (44 men and 53 women), of which 65 were African American, 13 were Hispanic, 12 were white, and 7 were Asian.
For analysis, the findings were classified into 2 data sets: the binocular data set, which included all eyes (n = 131), and the monocular data set, which included single eyes (n = 97). To minimize selection bias when selecting which eye to include from patients with 2 eligible eyes, the monocular data set included data from only the right eyes of these patients. Because there were no statistically significant differences between the data sets with respect to any of the outcome measures investigated, our report here is limited to the discussion of the monocular data set.
Analyses were performed using only 1 eye from each patient (n = 97). The results are summarized in the Table . Mean IOPk was 17.9 ± 3.0 mm Hg (range: 13.0-27.0 mm Hg); mean IOPs was 26.3 ± 6.6 mm Hg (range: 13.2-45.5 mm Hg); mean difference between IOPs and IOPk (IOPs − IOPk) was 8.4 ± 5.7; mean CCT value was 536 ± 42 μm; mean spherical equivalent (SE) refraction was −0.50 ± 1.87 diopters; and mean AL was 23.71 ± 1.15 mm. IOPs was significantly correlated with IOPk (r = 0.51, P < .0001) and age (r = 0.50, P < .0001). There was a weaker, albeit significant, correlation between IOPs and SE (r = 0.31, P = .002). There was no statistically significant correlation with AL or CCT. The difference between IOPs and IOPk (IOPs − IOPk) had a strong statistically significant correlation with IOPs (r = 0.89, P < .0001) and age (r = 0.56, P < .0001) and a weak significant correlation with SE (r = 0.32, P = .001).
| Mean ± SD | Correlation r: IOPs ( P ) | Correlation r: IOPs-IOPk ( P ) | |
|---|---|---|---|
| IOPs (mm Hg) | 26.3 ± 6.6 | 1.00 | 0.89 (<.0001) |
| IOPk (mm Hg) | 17.9 ± 3.0 | 0.51 (<.0001) | 0.07 (.51) |
| Age (y) | 54.4 ± 17.7 | 0.50 (<.0001) | 0.56 (<.0001) |
| SE (diopter) | −0.50 ± 1.87 | 0.31 (.002) | 0.32 (.001) |
| AL (mm) | 23.71 ± 1.15 | 0.11 (.26) | 0.07 (.51) |
| CCT (μm) | 536 ± 42 | 0.17 (.09) | 0.19 (.06) |
In addition, comparisons of scleral and corneal measurements are shown in Figures 2 and 3 . Figure 2 is a plot showing IOPs vs IOPk measurements with the line of equality. A total of 94.84% (92 out of 97 eyes) of scleral IOP measurements were higher than corneal IOP, with values ranging from 0.2-24.5 mm Hg (in 3 eyes, IOPs was slightly lower; in 2 eyes, IOPs was equal to IOPk). A Bland-Altman plot is shown in Figure 3 , depicting the mean difference (estimated bias) between IOPs and IOPk, as well as the amount of variability (±2 SD) around this mean. The mean difference between the 2 methods is 8.08 mm Hg, with most of the measurements falling within 2 SD of the mean.




