Purpose
To investigate the efficacy of decellularized porcine-derived membrane (tarSys; IOP Inc), a bioengineered eyelid spacer graft, for lower lid retraction correction in patients with Graves ophthalmopathy.
Design
Retrospective observational case series study.
Methods
This was a retrospective review of patients with Graves ophthalmopathy undergoing lower eyelid retraction surgery using decellularized porcine-derived membrane bioengineered eyelid spacer grafts from 2008 through 2011. Outcome measures included lower eyelid height (measured from the corneal light reflex to the lower eyelid margin, or marginal reflex distance-2 [MRD 2 ]), reduction of lagophthalmos, cosmetic appearance, complications, and need for further surgery. Presurgery and postreconstruction photographs were reviewed for functional and cosmetic outcome.
Results
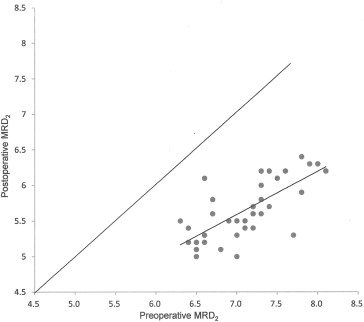
A total of 32 Graves patients and 37 eyelids underwent lower eyelid retraction surgery using decellularized porcine-derived membrane. There were 10 male and 22 female patients with mean age of 41.8 ± 8.6 years. Mean improvement in MRD 2 was 1.4 ± 0.4 mm. Mean reduction of lagophthalmos was 1.3 ± 0.4 mm. There are statistically significant differences between preoperative and postoperative MRD 2 and lagophthalmos (paired t test, both P < .0001). No evidence of infection and corneal erosion was noted and none of the patients needed further surgeries. Prolonged lower lid swelling and slight puffy appearance were noted for 6 patients. The swelling and puffy appearance resolved completely 3 months after surgery. Conjunctival granuloma formation was found in 1 patient. The cosmetic result was satisfactory in all cases.
Conclusions
Decellularized porcine-derived membrane, a bioengineered graft, is effective for the management of lower lid retraction in patients with Graves ophthalmopathy. It can offer an alternate graft for eyelid reconstruction.
Lower lid retraction, even though not as common as upper lid retraction, is present at diagnosis in about 20% of Graves ophthalmopathy (GO) patients. The causes of lower lid retraction may be attributable to chronic and longstanding inflammation resulting in fibrosis of the orbital fascia and suspensory system in GO. In addition, inferior rectus recession more than 4 mm also may lead to prominent lower lid retraction for Graves myopathy. A major consequence of lower lid retraction is lagophthalmos and corneal exposure.
The surgical correction of the lower lid retraction frequently requires a spacer graft to keep the retractors recessed and support the tarsus. Autogenous cartilage and hard palate mucous graft are commonly used as spacer materials. The thickness and contour of ear cartilage do not match the tarsus as well as hard palate. The hard palate graft is a composite autograft with a texture and thickness similar to tarsus. However, harvesting the hard palate graft requires an additional surgical manipulation. Donor-site morbidity and patient discomfort sometimes discourage the use of hard palate grafts. Homologous sclera such as banked sclera or tutoplast sclera (IOP Inc, Costa Mesa, California, USA) is useful for lower lid lengthening, but tends to be associated with absorption and recurrence. Homologous grafts also carry a risk of infectious disease transmission. Many other materials are used for lower lid retraction correction, such as human cadaveric acellular dermis (AlloDerm) or high-density polyethylene (Medpor). These materials offer the advantage of not requiring an additional procedure for autografts; however, they vary in effectiveness, permanence, and tissue tolerance.
Decellularized porcine-derived membrane (tarSys; IOP Inc) is a relatively new bioengineered eyelid spacer graft derived from a porcine source. It is derived from porcine small intestinal submucosa by Strike Force processing. Products derived from porcine small intestinal submucosa can be used in abdominal wall hernia repair in animal study and nasal septal perforation repair in human study. Decellularized porcine-derived membrane is an 8-layer or 12-layer, decellularized membrane consisting of collagen types I, III, and VI and made specifically for eyelid retraction repair. Recently, Borrelli and associates reported a case using decellularized porcine-derived membrane for the correction of lower lid retraction with good results. In this study, we present our experiences of using decellularized porcine-derived membrane implant to repair lower lid retraction for patients with Graves ophthalmopathy.
Methods
This study is a retrospective observational case series study. We retrospectively reviewed the charts of all patients with dysthyroid lower eyelid retraction undergoing repair using a decellularized porcine-derived membrane graft from February 2008 through December 2011. The Ethics Committee of the National Taiwan University Hospital approved the protocol of this study, which conformed to the tenets of the 1964 Declaration of Helsinki, and written informed consent was obtained from all patients. All GO patients were in euthyroid status and marginal reflex distance-2 (MRD 2 ) readings were stable for more than 6 months before surgeries. All lower lid retraction surgeries were performed by 1 oculoplastic surgeon (S.-L.L.).
Outcome measures included lower eyelid height (measured from the center of the pupil to the inferior eyelid margin, or MRD 2 ), reduction of lagophthalmos, evaluation of the cosmetic appearances (categorized by patients as dissatisfied, fair, or satisfied), complications, and need for further surgery. Patients were asked to return for follow-up at 1 week and 1, 3, and 6 months after operation. Complications such as infection, corneal erosion, allergic reaction, granuloma formation, and hematoma were evaluated at each visit. Statistical analysis was carried out using the Statistical Package for Social Sciences, version 11.0 (SPSS Inc, Chicago, Illinois, USA). Paired-sample t test was used to compare outcome measures such as MRD 2 and the degree of lagophthalmos before and after operation. Digital photographs from each patient were taken preoperatively and 6 months after surgeries. All photographs were obtained with identical lighting at primary gaze. For the comparison of MRD 2 between photographs, we used the measurement method reported by Li and associates. After digitally rotating the photographs so that a horizontal line bisected both pupils, the photographs were analyzed using computer-assisted digitized drawing software (Mirror, Canfield Clinical System; Canfield Scientific, Inc, Fairfield, New Jersey, USA). The corneal diameter and distance from the center of the pupil to the lower eyelid margin (MRD 2 ) were measured and standardized to a corneal diameter of 11 mm.
Surgical Technique
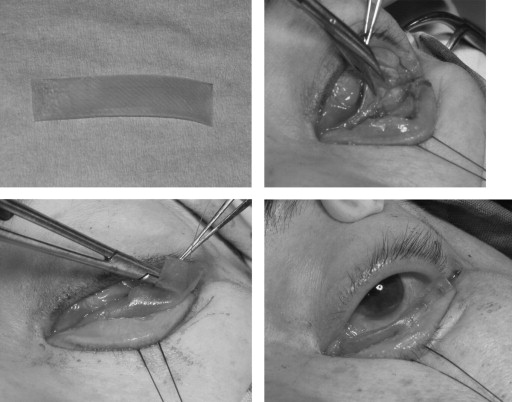
Lidocaine 2% with epinephrine was infiltrated through the inferior fornix, lateral canthal area. The initial part of the surgery was identical to the swinging eyelid transforniceal approach, as we have previously described. Surgery begins with a lateral canthotomy and cantholysis and a forniceal incision is created through the conjunctiva and lower eyelid retractors at the inferior tarsal margin. Further dissection is carried inferiorly in the septal plane to recess the lower retractor and release cicatricial tissues if the patients underwent previous surgeries such as orbital decompression. The decellularized porcine-derived membrane graft is placed into a 10-mL normal saline dish with 1 mL (10 mg) gentamicin solution. The graft is allowed to rehydrate for at least 20 minutes. The width of the graft is a 4:1 correlation with the amount of lower lid retraction correction desired. If the amount of the lower lid retraction is more than 2 mm, we used the full size (10 mm) of the decellularized porcine-derived membrane graft. The appropriate-size graft can be easily trimmed by a surgical scissor and then sutured to the inferior tarsal margin and the conjunctiva, with the greatest vertical dimension placed laterally ( Figure 1 ). The interrupted buried 6-0 polyglactin sutures are passed through the graft with the horizontal edge parallel to the eyelid margin ( Figure 1 ). The lateral canthotomy is then approximated with 5-0 polyglactin sutures. Finally, the skin wound is closed with interrupted 6-0 nylon sutures. Two temporary sutures are placed from the lower eyelid margin to the eyebrow to ensure upward traction of the eyelid during the initial healing phase (1 week). A pressure bandage is applied and left for 3 days.
Results
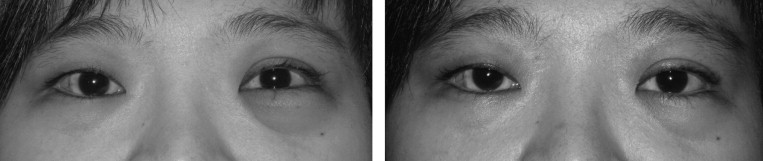
A total of 32 Graves patients and 37 eyelids underwent lower eyelid retraction surgery using decellularized porcine-derived membrane graft. There were 10 male and 22 female patients with a mean age of 41.8 ± 8.6 years. Among the 37 eyelids, 19 eyes underwent prior orbital decompression surgeries, 5 eyes underwent prior orbital decompression and subsequent muscle surgeries, and 1 eye had a previous muscle surgery. Only 12 eyes received no previous eye surgery. The mean preoperative MRD 2 was 7.1 ± 0.5 mm, whereas the mean MRD 2 measured 6 months after surgery was 5.6 ± 0.4 mm. The average MRD 2 change after operation was 1.4 ± 0.4 mm. There is statistically significant difference between preoperative and postoperative MRD 2 (paired t test, P < .0001) ( Figure 2 ). The mean degree of lagophthalmos before operation was 1.7 ± 0.6 mm, whereas the mean degree of lagophthalmos 6 months after surgery was 0.3 ± 0.4 mm. The average reduction of lagophthalmos after operation was 1.3 ± 0.4 mm. There is statistically significant difference between preoperative and postoperative lagophthalmos (paired t test, P < .0001) No patient had keratopathy under slit-lamp biomicroscopy at the first follow-up visit. No evidence of infection and corneal erosion was noted and none of the patients needed further surgeries. Conjunctival granuloma formation was found 2 weeks after surgery in 1 patient. Excision of the granuloma and reapproximation of the dehiscence wound resolved the complication with good result. Prolonged lower lid swelling and slight puffy appearance were noted in 6 patients. The swelling and puffy appearance resolved completely 3 months after surgery ( Figure 3 ). All patients perceived the improvement of lower lid retraction and were satisfied with their cosmetic results ( Figures 4 and 5 ).