Corneal and Conjunctival Degenerations
Fina Cañas Barouch
Kathryn Colby
Corneal dystrophies are usually bilateral, inherited, symmetric conditions with onset early in life. In contrast, corneal degenerations can be unilateral or bilateral, are often asymmetric, with findings typically located peripherally and not associated with any inheritance pattern or genetic predisposition. The onset of the degenerations is often in middle life or later, and is characterized by slow progression. We describe in this chapter the corneal and conjunctival degenerations. Ectatic degenerations are discussed in Chapter 49.
PINGUECULA/PTERYGIUM
A pinguecula is an elevated, grayish yellow, horizontally oriented, triangular area of thickened bulbar conjunctiva adjacent to the limbus within the interpalpebral fissure. A pinguecula can encroach toward the cornea, but if it crosses onto the cornea it then becomes, by definition, a pterygium. Pingueculae are most frequently found nasally and are usually bilateral (1). They are pathologically characterized by elastotic degeneration, with hyalinization of the conjunctival stroma.
The incidence of pingueculae increases with age. Most individuals over the age of 80 have some degree of pinguecula formation (2). Their etiology is unknown but may be related to ultraviolet (UV) light exposure (3). It is thought that the nasal location may be due to actinic damage that preferentially occurs in this area from reflection of sunlight from the nose onto the nasal limbus (4). Other possible etiologic factors for pingueculae include trauma, wind, or drying. Pingueculae rarely cause symptoms, but if they become inflamed they can be treated with lubricants or topical antiinflammatory medications.
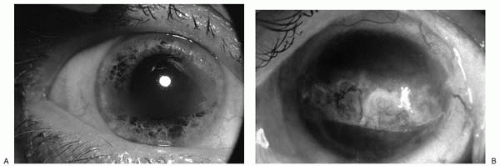
A pterygium is a growth of horizontally oriented winglike, fibrovascular tissue onto the cornea. Like pingueculae, pterygia are found within the interpalpebral fissure and are more commonly located nasally than temporally (Fig. 48-1). Although pterygia and pingueculae are similar clinically and histopathologically, it is unclear if pingueculae give rise to pterygia. Pterygia are associated with UV exposure and are more common in warmer climates, particularly in equatorial countries (5, 6, 7). Histopathologically, pterygia are characterized by fibrovascular proliferation and elastotic degeneration of collagen with the destruction of Bowman’s layer of the cornea (8).
Pterygia are often bilateral and progressive. When they involve the visual axis, reduced vision, induced astigmatism, irritation, and tearing can occur. The cosmetic appearance of the pterygium may also be the presenting complaint. True pterygia are considered conjunctival degenerations. In contrast, pseudopterygia, characterized by connections of the conjunctiva to the cornea that are not adherent at the limbus, often develop in response to trauma or inflammation. True pterygia are always located horizontally within the palpebral fissure, whereas pseudopterygia may be located in any axis. A probe cannot be passed beneath a true pterygium because of its adherence to the limbus.
Medical treatments for pterygia include lubrication and vasoconstrictors. Patients may be counseled to avoid sun, wind, and dust. When a pterygium approaches the visual axis or induces significant astigmatism, surgical excision should be considered. Simple excision leaving bare sclera is associated with a 30% to 70% recurrence rate, whereas excision with primary closure of the conjunctiva is associated with a 5% to 10% recurrence rate (9,10). Further reductions in recurrence rate have been noted following excision with a conjunctival autograft or an amniotic membrane graft (9, 10, 11). Adjuvant mitomycin C may also be used to discourage recurrence, although serious side effects can occur if this agent is used postoperatively on bare sclera as opposed to a single intraoperative application (12).
CALCIFIC BAND KERATOPATHY
Calcific band keratopathy is characterized by calcium deposition within the anterior cornea, most typically in the interpalpebral fissure. The calcium, primarily in the form of hydroxyapatite, deposits in the epithelial basement
membrane, Bowman’s layer, and the anterior stroma. The overlying epithelium is sometimes involved and may be disrupted, leading to symptoms of recurrent erosion. Band keratopathy typically begins in the peripheral cornea at the 3 and 9 o’clock positions (Fig. 48-2A). The central cornea is affected last. In advanced cases, the calcium deposits traverse the entire cornea (Fig. 48-2B). The peripheral edge is usually sharply demarcated and separated from the limbus by a clear zone. The clear zone may be due to the buffering capacity of the limbal vessels that prevents the precipitation of calcium. Alternatively, it may be due to the termination of Bowman’s layer in the peripheral cornea (13). The central edge of the deposit tends to be less sharply demarcated with a feathered appearance. Early calcium deposition is hazy and gray. As the disease progresses, the deposits become chalky white and opaque. Holes scattered throughout the band keratopathy represent the corneal nerves penetrating Bowman’s layer, giving the deposit a “Swiss cheese” appearance.
membrane, Bowman’s layer, and the anterior stroma. The overlying epithelium is sometimes involved and may be disrupted, leading to symptoms of recurrent erosion. Band keratopathy typically begins in the peripheral cornea at the 3 and 9 o’clock positions (Fig. 48-2A). The central cornea is affected last. In advanced cases, the calcium deposits traverse the entire cornea (Fig. 48-2B). The peripheral edge is usually sharply demarcated and separated from the limbus by a clear zone. The clear zone may be due to the buffering capacity of the limbal vessels that prevents the precipitation of calcium. Alternatively, it may be due to the termination of Bowman’s layer in the peripheral cornea (13). The central edge of the deposit tends to be less sharply demarcated with a feathered appearance. Early calcium deposition is hazy and gray. As the disease progresses, the deposits become chalky white and opaque. Holes scattered throughout the band keratopathy represent the corneal nerves penetrating Bowman’s layer, giving the deposit a “Swiss cheese” appearance.
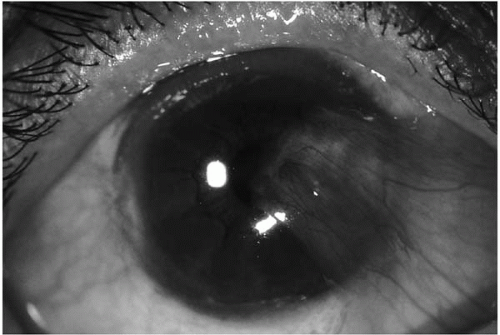 FIGURE 48-1. Right eye with pterygia. The larger nasal and smaller temporal pterygia are within the interpalpebral fissure. |
Deposition of basophilic granules in Bowman’s layer is the earliest change detected on histology (14). Eventually the granules coalesce and Bowman’s layer becomes calcified. The calcium deposition is primarily extracellular. In cases of hypercalcemia, however, the calcium deposition is also found within the basal epithelial cells. Calcified Bowman’s layer can break into small plaques and disrupt the overlying epithelium. Hyaline material deposits between the fragments of calcified Bowman’s layer and the overlying epithelium giving the appearance of reduplication of Bowman’s layer (13,14).
The pathogenesis of band keratopathy has not been well defined. Calcium and phosphate are present in tears at concentrations that are barely soluble. Precipitation of calcium can occur easily with an alteration in tear osmolality, elevation of the pH from corneal tissue metabolism, increase in the concentration of either calcium or phosphate, or tear evaporation from exposure within the interpalpebral fissure. The pH of the interpalpebral fissure is higher than that of the rest of the ocular surface because of carbon dioxide release from the exposed zone. This also enhances calcium precipitation. In an experimental model in which animals with induced ocular inflammation were given overdoses of vitamin D, band keratopathy developed only in animals with open eyelids but did not develop if the eyelids were kept closed (15). In addition, band keratopathy can occur rapidly in patients with dry eyes, further suggesting a role for tear evaporation in the pathogenesis of this process (16).
Calcific band keratopathy is associated with hypercalcemic states, chronic ocular disease, and repeated ocular injury (Table 48-1). Band keratopathy is often seen in patients with chronic keratitis, long-standing glaucoma, or chronic uveitis (e.g., children with juvenile idiopathic arthritis). Interestingly, band keratopathy can be seen in cases of chronic uveitis that begin in childhood but rarely in chronic uveitis of adult onset. It is also seen in patients with systemic hypercalcemia or hyperphosphatemia such as in chronic renal failure, hyperparathyroidism, milk-alkali syndrome, sarcoidosis, vitamin D toxicity, and metastatic
neoplastic disease (17, 18, 19, 20, 21). Band keratopathy has also been associated with the use of pilocarpine with mercurial preservatives, intraocular silicone oil, older viscoelastics with high phosphate concentrations, and phosphate forms of corticosteroids (22, 23, 24, 25, 26). Hereditary forms occur in hypophosphatasia, Norrie’s disease, and autosomal-recessive congenital band keratopathy.
neoplastic disease (17, 18, 19, 20, 21). Band keratopathy has also been associated with the use of pilocarpine with mercurial preservatives, intraocular silicone oil, older viscoelastics with high phosphate concentrations, and phosphate forms of corticosteroids (22, 23, 24, 25, 26). Hereditary forms occur in hypophosphatasia, Norrie’s disease, and autosomal-recessive congenital band keratopathy.
TABLE 48-1. CONDITIONS ASSOCIATED WITH BAND KERATOPATHY | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Patients with band keratopathy are typically asymptomatic and do not require treatment. In cases in which vision is reduced or there is discomfort and foreign-body sensation when the band breaks through the epithelium or the deposits irritate the eyelids, the central deposits can be removed. The mainstay of treatment is chelation of the calcium with ethylenediaminetetraacetic acid (EDTA) (27,28). The epithelium is removed with a sponge or a blade to allow penetration of the EDTA. EDTA (0.35%) can be applied to the subepithelial calcification via surgical sponges or directly using a reservoir such as a corneal trephine or a photorefractive keratectomy (PRK) well to hold the solution. The chemical reaction takes several minutes to occur (at least 5 minutes). Mechanical scraping following application of EDTA facilitates removal. Multiple EDTA applications are typically needed to remove all of the calcium. The excimer laser has also been used to remove calcification within the visual axis (29,30). Phosphate-containing drops are avoided to prevent recalcification. Amniotic membrane transplantation after the surgical removal of calcium deposits has been shown to help facilitate resurfacing of the epithelial defect with corneal epithelium, although a bandage contact lens is generally sufficient to accomplish the same goal (31).
LIMBAL GIRDLE OF VOGT
Limbal girdle of Vogt is a narrow, arcuate, chalky white opacity in the nasal and temporal limbal areas of the cornea within the interpalpebral fissure (32). It occurs more frequently in the nasal limbus than in the temporal limbus but is often symmetric. There are two types of limbal girdle: Type 1 is thought to represent early calcific band keratopathy and is characterized by a white band that contains multiple holes separated from the limbus by a clear area. Type 2 is the more common true limbal girdle. It is a chalky band without holes that is contiguous to the conjunctiva. No lucent zone is present. Fine white lines that run radially in type 2 limbal girdle are best seen using retroillumination and sclerotic scatter. Histopathologically, limbal girdle is composed of hyperelastotic degeneration at the level of Bowman’s layer similar to that seen in pingueculae. The prevalence of limbal girdle increases with age (32). It is present in normal eyes in 55% of those ages 40 to 60 and in 100% of those over 80 years of age (32). It does not cause any symptoms or decreased vision and thus does not require treatment.
CALCAREOUS DEGENERATION
Calcareous degeneration is characterized by calcium deposition within the deep and anterior layers of cornea. It is similar to calcific band keratopathy but also involves the posterior corneal stroma. Calcium deposition can be full thickness or can spare Bowman’s layer and the corneal epithelium. The calcification typically occurs more rapidly than in band keratopathy and may develop as quickly as within a 24-hour period (33). Calcareous degeneration is usually seen in seriously diseased or injured eyes with an epithelial defect and exposed stroma or with anterior segment vascular compromise. It can be a complication of severe dry eye, recurrent corneal ulcerations, chronic ocular inflammation, or multiple surgical procedures (33, 34, 35, 36). It is also seen in phthisis bulbi and can be associated with bone formation elsewhere in the globe. Primary calcareous degeneration can occur in patients with normal calcium and phosphate levels. It has been reported in a case of a failed corneal graft and following the use of topical steroidphosphate therapy in a patient with chronic keratoconjunctivitis after Stevens-Johnson syndrome (37,38). Chelation
with EDTA is ineffective in treating this condition because the calcium deposition is deeper than in band keratopathy. Penetrating keratoplasty is often required for visual rehabilitation (39).
with EDTA is ineffective in treating this condition because the calcium deposition is deeper than in band keratopathy. Penetrating keratoplasty is often required for visual rehabilitation (39).
SALZMANN’S NODULAR DEGENERATION
Salzmann’s nodular degeneration, first described in 1925, is characterized by elevated gray to blue-gray, fibrous nodules in the superficial corneal stroma just beneath the epithelium (Fig. 48-3) (40). The nodules elevate the epithelium. There are usually one to nine discrete paracentral lesions, often in a circular array at areas of corneal scarring or at the junction of old corneal scars and clear cornea. Each nodule is separated from other nodules by clear cornea, and iron lines may outline each nodule (41). The nodules are not vascularized but the underlying stroma may be (42). Salzmann’s nodular degeneration is associated with past corneal inflammation, but the onset of the lesions is gradual and often occurs many years after the keratitis. It may follow phlyctenular keratitis, vernal keratitis, trachoma, interstitial keratitis, exposure keratopathy, keratitis sicca, Thygeson’s superficial punctate keratitis, and other forms of chronic keratitis (42, 43, 44). It can also be associated with recurrent corneal erosions (45). It occurs more often in women than in men, and the nodules can be bilateral or unilateral.
Histopathologically, Bowman’s layer is replaced by eosinophilic material. There is thinning and flattening of the epithelium with degeneration of the basal cells and disorganization of the underlying stromal collagen. The nodule itself is not vascularized and consists of dense collagenous tissue. In addition, residua of old keratitis may be seen in the surrounding stroma.
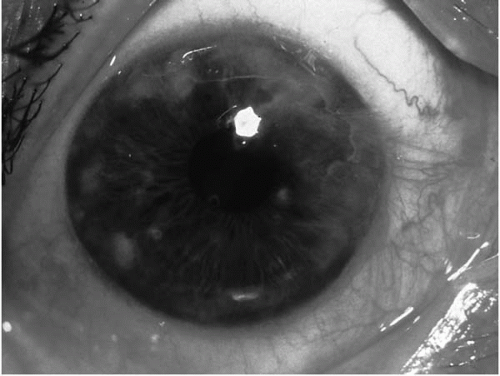 FIGURE 48-3. Multiple elevated nodules in the cornea of a patient with Salzmann’s nodular degeneration. |
Many patients with Salzmann’s nodular degeneration are asymptomatic. Patients may complain of reduced vision if the nodules are located in the central cornea. Elevated nodules can cause discomfort and epithelial erosions. Treatment by simple excision of the nodule, lamellar keratectomy, or excimer laser phototherapeutic keratectomy is indicated if vision is decreased or if recurrent erosions occur (46, 47, 48). Recurrences are common but take many years to develop.
IRON DEPOSITIONS
Iron deposits in the deep corneal epithelium can assume a variety of configurations including lines, rings, or diffuse depositions. The most common iron deposition is the Hudson-Stähli line (49,50). Hudson-Stähli lines are located in the deep corneal epithelium at the line of eyelid closure at the junction of the middle and lower thirds of the cornea. The line curves downward at its center, is approximately 0.5 mm wide, 1 to 2 mm long, and is usually yellow, green, brown, or white in color. It is best visualized as a black line when cobalt blue light is used. Hudson-Stähli lines occur most commonly in patients over the age of 50, but decrease in frequency after the age of 70 (50,51). There is no sex predilection. Histologic evaluation shows intracellular iron deposition in the form of ferritin-like material, possibly hemosiderin, in the basal epithelial cells of the cornea (50). The cause of Hudson-Stähli lines is unknown, but the tear film may be the source of iron (49). Other possible sources of iron include the aqueous humor, limbal vessels, and cellular or blood breakdown.
Other iron lines include Fleischer rings around a cone in keratoconus (50), Ferry lines near filtering blebs (52), and Stocker-Busacca lines in front of pterygia (53). Iron lines can occur in association with superficial corneal scars, after corneal transplants (54), and surrounding refractive corneal procedures (e.g., after radial keratotomy and laser in situ keratomileusis) (55,56). They may also be seen with Salzmann’s nodules (57), in congenital spherocytosis (58), and in association with iron foreign bodies. Alterations in corneal shape with secondary pooling of tears are thought to contribute to the formation of iron lines (54,55). In addition, migration of corneal epithelial cells may contribute to the location and shape of iron lines (59). Iron lines are asymptomatic and do not require treatment.
Coats’s white ring is an iron deposition that occurs at the level of Bowman’s layer (60). The overlying epithelium remains intact. It is usually located in the inferior cornea and is 1 mm or less in diameter. It appears as a small ring made up of discrete white dots that can coalesce. The rings are secondary to corneal trauma and may in fact represent remnants of old metallic foreign bodies (61). Coats’s rings are incidental findings and do not require treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree