Purpose
To investigate the effect of conjunctival mini-flap operation to treat restrictive strabismus in patients with diplopia caused by conjunctival adhesion and hyperplasia after periocular surgery.
Design
Case series study.
Methods
Eleven patients with diplopia and restrictive strabismus attributable to conjunctival dysplasia after periocular surgery underwent a conjunctival mini-flap surgery without a muscle operation and were followed-up at 1, 3, and 6 months after surgery. The Hess screen test, binocular single vision field with Goldmann perimetry, and extraocular muscle movement were analyzed pre- and postoperatively. Patient satisfaction with the cosmetic results of conjunctival mini-flap operation was also investigated.
Results
The mean preoperative alignment deviation in primary position was 10.4 ± 5.6 prism diopters (PD). Diplopia in the primary position was resolved in 95% of the patients. The mean postoperative deviation was 1.36 ± 2.34 PD at the primary position. No significant complications or recurrences were noted after mean 9.5 ± 4.2 months follow-up.
Conclusion
Conjunctival mini-flap operation is an effective and safe surgical technique for treating patients with diplopia and restrictive strabismus following periocular surgery.
Restrictive strabismus and diplopia are uncommon but important complications of periocular surgery. Restrictive strabismus has been reported after pterygium excision, cosmetic wide conjunctivectomy, scleral buckle procedure, and orbital surgery. Scarring of the conjunctival-perimuscular connective tissue complex and symblepharon may also result in incomitant strabismus.
There is a higher chance of trauma or fibrosis in the connective tissue surrounding the globe and extraocular muscle adjacent to the pterygium after periocular surgery. In addition, cicatrical change, scar tissue formation, and conjunctival hyperplasia after periocular surgery may cause a restriction of ocular rotation contralateral to the lesion. Importantly, any periocular surgery that leaves bare sclera, such as recurrent pterygium excision or cosmetic wide conjunctivectomy, can cause restrictive strabismus.
Cosmetic wide conjunctivectomy is a surgical treatment for chronic conjunctival injection to make eyes look white by leaving the wide sclera bare. This procedure has been performed throughout South Korea, and a similar procedure is being performed in the United States. However, several severe complications, such as scleral thinning with or without calcified plaque formation, fibrovascular adhesion, chronic conjunctival epithelial defects, and diplopia, have been reported.
To prevent restrictive strabismus, several methods, including conjunctival autograft, amniotic membrane transplantation (AMT), and antimetabolites, have been used. Because adhesions often recur, restrictive strabismus is difficult to manage using standard surgical techniques such as simple scar removal, muscle surgery, or AMT. Previous studies have reported that surgical treatment is challenging because it requires a combination of surgery on the conjunctival-perimuscular connective tissue complex and the rectus muscle, with restrictive strabismus often recurring.
Conjunctival mini-flap operation was first introduced by Akura and associates for pterygium removal. The procedure involves dissection of conjunctival hyperplasia and adhesiolysis. Several studies have shown successful pterygium removal with lower recurrence rate, and conjunctival mini-flap is reported to be safe and effective in reducing the postoperative recurrence of primary pterygium compared to the conjunctival autograft technique. Based on these previous reports, we performed a conjunctival mini-flap without involving muscle operation for restrictive strabismus. To our knowledge, there have been no reports describing the use of conjunctival mini-flap to treat restrictive strabismus after periocular surgery. This article reports a retrospective case series describing the long-term effect of conjunctival mini-flap in restrictive strabismus caused by conjunctival hyperplasia and adhesion after anterior segment surgery.
Methods
This retrospective review included 11 consecutive patients who underwent conjunctival mini-flap without involving muscle operation for restrictive strabismus after previous periocular surgery between January 6th, 2011 and June 24th, 2012. Data were obtained from the electronic medical records of Severance Hospital, Yonsei University College of Medicine, Seoul, South Korea. This interventional case series study was approved by the Institutional Review Board (4-2012-0786) of Yonsei University College of Medicine and adhered to the tenets of the Declaration of Helsinki.
All patients underwent a complete ophthalmologic examination that included best-corrected visual acuity (BCVA), manifest refraction, intraocular pressure, slit-lamp examination, and fundus examination. Motor alignment was determined by the prism cover test with the patient fixating at a 20/30 target placed at 6 m. Diplopia symptoms were assessed by subjective complaints and binocular single visual fields with Goldmann perimetry (Haag Streit, Bern, Switzerland), the Hess screen test, and ductions and versions were also evaluated. All evaluations were performed before surgery and repeated 1, 3, and 6 months after surgery. In all cases, conjunctival mini-flap procedure was performed by a single surgeon (K.Y.S.).
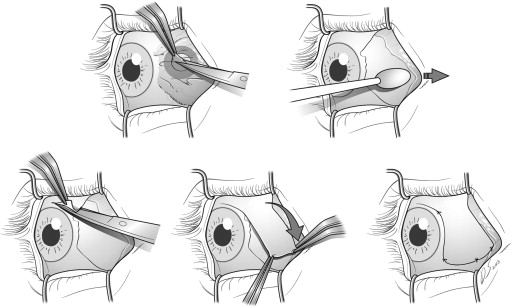
Conjunctival mini-flap procedure was composed of the following steps ( Figure 1 ). First, 0.5% proparacaine hydrochloride eye drops were applied for topical anesthesia and subconjunctival local anesthesia was injected around the lesion. We pressed the conjunctiva with a cotton swab where we injected a local anesthetic agent to dissect the epithelium from the underlying Tenon and fibrotic adhesion more easily. The underlying abnormal Tenon and fibrotic adhesion were also carefully dissected from the sclera. The overlying conjunctiva was excised together with the abundant scarred and hyperplastic tissue, because it was very difficult to distinguish and dissect abnormal subconjunctival tissue from the overlying conjunctiva. After careful adhesiolysis, removal of abundant scar and hyperplastic tissue, remnant subconjunctiva tissue was pushed to the peripheral side to avoid muscle damage and excessive bleeding. In addition, we fully covered the bare sclera with the conjunctiva flap after removal of sufficient subconjunctival tenon tissue, which permitted the flap to be rotated easily. Then, the range of motion of extraocular muscle and the symptoms of diplopia were checked. If diplopia symptoms were resolved and eye movement was normalized, the conjunctival flap adjacent to the lesion was harvested. For mobility of the conjunctival donor flap and prevention of recurrence, extensive sub-Tenon tissue removal of the donor site was performed. The superior or inferior flap was harvested according to the defect size and location. After the flap was harvested, the horizontal flap was rotated to vertical or the vertical flap to horizontal to cover the defect site. The flap was then moved to the sclera to cover the area where the lesion had been located and attached to the sclera with 8-0 vicryl. At this point, we adjusted the suture to evenly distribute tension and attached the flap to the sclera firmly so the flap acted as a barrier against abnormal tissue growth from the periphery. For patients who were expected to have excessive reactive tissue inflammation, 10-0 nylon was used. Antibiotic eye drops and topical steroids were used for postoperative management.
Subject data were tabulated using Microsoft Excel 2010 software (Microsoft, Redmond, Washington, USA). The SPSS software (ver. 20.0 for Windows; SPSS, Inc, Chicago, Illinois, USA) was used for data analysis. Paired t test was used to compare preoperative and postoperative deviation change.
Results
The patients’ characteristics are summarized in Table 1 . Two male and 9 female patients were included in this study. The mean age at the time of initial examination was 42.1 ± 9.5 years. Two patients had a history of unilateral pterygium excision surgery. All lesions were on the nasal side in patients who had undergone more than 1 previous pterygium surgery. Nine patients had undergone bilateral cosmetic wide conjunctivectomy combined with postsurgical mitomycin C application. All these patients had undergone more than 1 reoperation because of recurrence of hyperemia or diplopia. Mean preoperative alignment deviation in primary position was 10.4 ± 5.6 prism diopters (PD). Onset of postoperative diplopia occurred at a mean of 7.7 ± 6.8 months.
| Patients (Eyes) | Age (y) | Sex | Previous Eye Surgery, Patients (Eyes) | Postoperative Onset of Diplopia, mo (range) | Preoperative Alignment Deviation in Primary Position (PD) | Mean Postoperative Deviation in Primary Position (PD) | ||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Pterygium | CWC | |||||
| 11 (14) | 42.1 (32-52) | 2 | 9 | 2 (2) | 9 (12) | 7.7 (1-24) | 10.18 ± 5.65 | 1.36 ± 2.34 |
Preoperatively, all patients had diplopia in lateral gaze, and 4 patients had diplopia at the primary position. Ten patients had esotropia and limited abduction, and the mean angle of deviation was 10.2 ± 5.8 PD in the primary position. One patient had limited adduction, 12 PD exotropia in the primary position, and 10 PD in the lateral gaze ( Table 2 ).
| Case | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Age, y | 32 | 33 | 42 | 46 | 51 | 35 | 54 | 28 | 32 | 48 | 52 |
| Sex | M | F | F | F | F | F | F | F | M | F | F |
| Previous surgeries | CWC (OU) | CWC (OU) | CWC (OU) | CWC (OU) | CWC (OU) | CWC (OU) | Pterygium (OS) | CWC (OU) | CWC (OU) | CWC (OU) | Pterygium (OS) |
| Associated treatment | Re-op (OU) × 4 | Strabismus op (OS) × 3 | Re-op (OS) × 1 | Re-op (OD) × 2 | Pterygium Re-op (OS) × 4 | Re-op (OS) × 4 | Re-op (OS) × 2 | Re-op (OU) | Pterygium Re-op (OS) | ||
| Conjunctival Avastin inj.(OS) | |||||||||||
| Onset of postoperative diplopia a | 7 mo | 6 mo | 9 mo | 9 mo | 1 mo | 24 mo | 1 mo | 6 mo | 12 mo | 3 mo | 5 mo |
| Preoperative diplopic field | RG, LG, UG | RG, LG, UG, DG | UG, LG | AG | RG | AG | PP, LG | LG | PP, LG | LG | LG |
| Preoperative alignment | |||||||||||
| PP | 12 RXT | 10 LET | 10 LET | 12 ET | 3 RET | 20 ET | 5 ET | 5 ET | 7 ET | 10 ET | 20 ET |
| RG | 10 RXT | Ortho | 5 RET | 10 ET | 14 RET | 20 ET | Ortho | 5 ET | 10 ET | 10 ET | 10 ET |
| LG | 10 RXT | 10 LET | 20 LET | 20 ET | 12 RET | 20 ET | 7 ET | 5 ET | 10 ET | 10 ET | 10 ET |
| UG | Ortho | 10 LET | Ortho | Ortho | Ortho | 5 RHoT | Ortho | Ortho | Ortho | Ortho | Ortho |
| DG | Ortho | 10 LET | Ortho | Ortho | Ortho | 5 LHoT | Ortho | Ortho | Ortho | Ortho | Ortho |
| Preoperative ductions (scale range, +4 to −4) | Limited adduction 1-R | Limited abduction 1-L | Limited abduction 1-L | Limited abduction 1-L | Limited abduction 1-R | Limited abduction 1-OU | No | Limited abduction 1-L | Limited abduction 1-L | No | Limited abduction 1-L |
| OP eye | OU | OS | OS | OS | OD | OU | OS | OS | OS | OU | OS |
| Follow-up | 10 mo | 20 mo | 10 mo | 8 mo | 7 mo | 7 mo | 7 mo | 14 mo | 10 mo | 6 mo | 6 mo |
| Postoperative alignment | |||||||||||
| PP | Ortho | 5 LET | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho | 5 ET | 5 ET | Ortho |
| RG | Ortho | Ortho | Ortho | Ortho | Ortho | 5 ET | Ortho | Ortho | 5 ET | 5 ET | Ortho |
| LG | Ortho | 5 LET | 5 XT | Ortho | Ortho | 5 ET | Ortho | Ortho | Ortho | 5 ET | Ortho |
| UG | Ortho | 5 LET | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho |
| DG | Ortho | 5 LET | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho | Ortho |
| Diplopia symptom after 6 months | No | No | Single vision at PP | No | No | No | Single vision at PP | No | No | No | No |
| Diplopic field after 6 months | All far pph | Far LG | UG, LG | No | No | Far UG | LG, DG | No | All far pph | No | No |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


