1 Concepts of Intranasal Surgery of the Paranasal Sinuses
Intranasal endoscopic surgery of the paranasal sinuses has essentially been developed for the treatment of chronic sinusitis. Only a few decades ago, the therapy of chronic sinusitis had consisted of the radical removal of the diseased mucosa, which was considered as of a biologically inferior quality (Albrecht 1926). External–meaning transfacial and transoral–approaches were the rule. Intranasal endoscopic surgery has not only become minimally invasive by changing the access but has also switched to the aim of preservation of the mucosa. Several prerequisites must be met if this alternative to the classical operations is to succeed:
• Modification of long-standing concepts of mucosal pathophysiology
• A more thorough knowledge of topographic anatomy
• Adaptation to endoscopic operative techniques using special angled telescopes and instruments through a narrow access port
• Abandonment of cherished principles of en-bloc clearance via wide access
• A long-term treatment plan that includes supplementary procedures and time-consuming endoscopic aftercare, which the patient must accept as an important part of the treatment
What was at first criticized as hazardous has subsequently been accepted as routine throughout the world. Endoscopic sinus surgery (ESS) today includes the use of the microscope and other technical improvements such as the laser or computer-assisted navigation, and is widely applied to other indications than sinusitis, e. g., for the treatment of trauma, malformations, and neoplasias. Regardless of this variety of indications, the local reactions of the mucosal texture to any of these noxious factors have much in common, and thus an intimate knowledge of its endoscopic and pathohistological appearance is key to its successful handling during surgery and during the postoperative phase, when wound healing has to be supported.
Attention to the details of this complex strategy is needed if one is to reap the full benefit of intranasal surgery, to avoid complications and disappointing results, and to recognize the unsolved problems obstructing the development of ideal treatment.
Surgical Pathology of the Sinus Mucosa
The respiratory mucosa of the nose and paranasal sinuses is part of a large and coherent system of internal surfaces reaching from the nostrils to the bronchi and communicating with the middle ear spaces (Fig. 1.1). It must, therefore, be regarded as a unit and be thoroughly investigated whenever parts of it produce signs of pathological alterations. But it does not present a homogenous histological structure throughout its extent. Its texture depends on site, age, and physical/biological responses to metabolic, endocrine, and other factors.
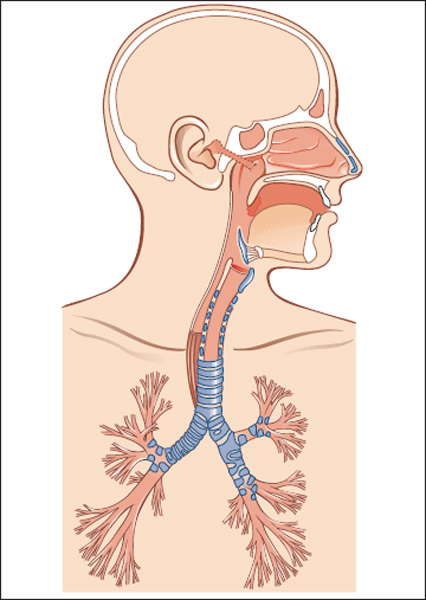
Fig. 1.1 The coherent system of respiratory mucosa extending from the nasal cavity into the paranasal sinuses, the tracheobronchial tree and, via the eustachian tube, into the middle ear. Its epithelial self-cleaning drainage system is susceptible to inflammatory disturbances. Infection in one compartment can involve remote areas.
In the nasal cavity, secretory elements (goblet cells and mucosal glands) are abundant where the mucosa carries a dense ciliary layer. In the more remote niches of the large sinuses, these typical characteristics are sparser and the histological picture more nearly resembles that of a mucoperiosteum with, at times, a thin serosal layer resembling the pattern of the middle ear and mastoid. Tos et al. (1978) have accurately measured the normal variation in density of the mucosal glands in the sinuses: under pathological conditions this pattern of distribution can change radically. The frequent macroscopic variants of the mucosa, even in the absence of inflammation, are already familiar to the rhinologist: dry, thickened regions at the nasal valve, atrophic areas over bony ridges, succulent velvety ends of the turbinates with arterial or venous coloration, and finally the swollen, pale, mulberrylike, bluish-red colored mucosa on the posterior end of the turbinates.
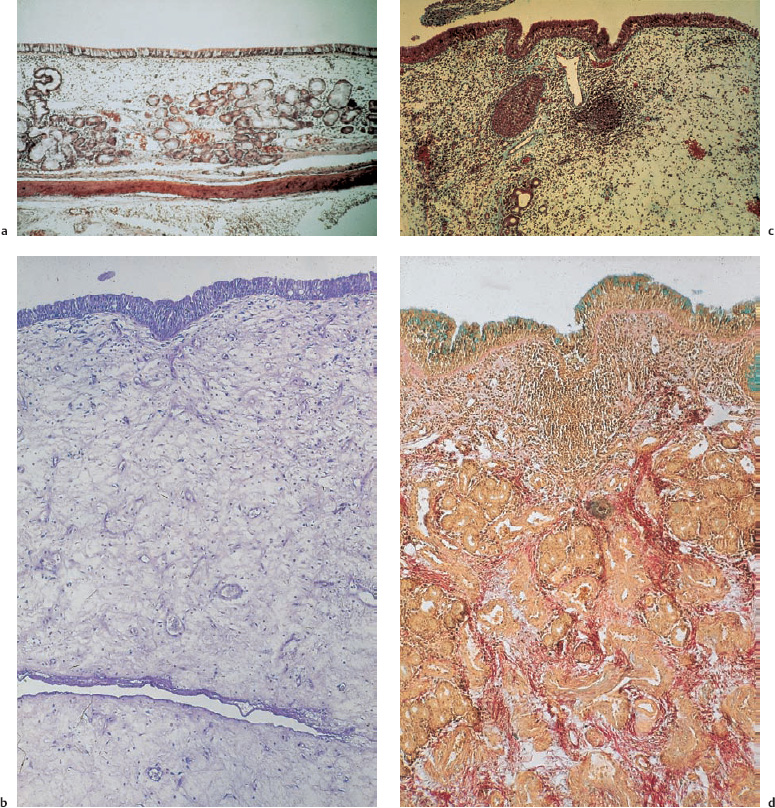
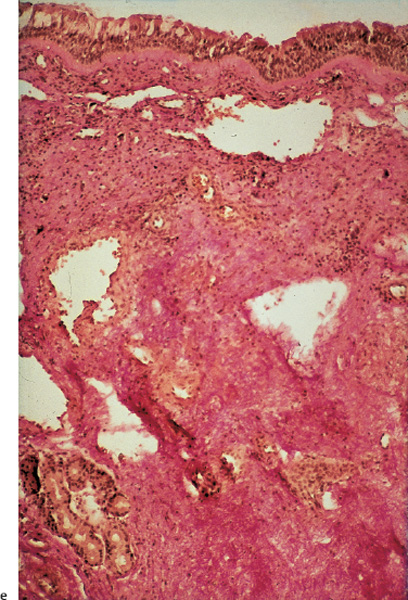
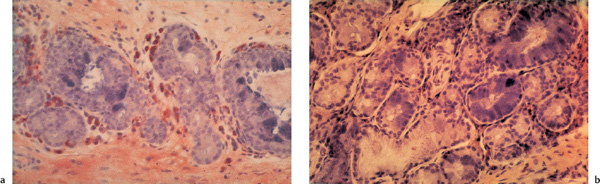
Fig. 1.2 a–e Histopathology of sinus mucosa in chronic rhinosinusitis.
a Normal respiratory mucosa of the ethmoid with ciliary epithelium and few secretory glands (H&E,×20).
b Edematous reaction of respiratory epithelium as first stage of inflammation. Wide intercellular spaces filled with lymph and hyalinic substance. Scarce cell infiltration (H&E,×63).
c Ethmoid mucosa in chronic sinusitis showing loose stroma with disseminated clumps of cells–microabscesses–but no glands (Goldner,×70).
d Chronic mucositis predominantly featuring glandular hyperplasia (Goldner and Alcian blue,×63).
e Chronic sinusitis with traits of scar formation, rich in collagen fibers and poor in leukocytes (van Gieson,×63).
The local appearances of the mucosa show even more marked variations in sinusitis. The endoscopist is familiar with the various swellings, edematous areas, papillary hyperplasia, and polyps that differ between the two sides and even within one nasal cavity. Using standardized mucosal biopsies, Hosemann and Wigand (1985) have demonstrated the wide variation in histopathology of sinus mucosa in diffuse polypoid hyperplastic sinusitis (Fig. 1.2a–e) . A diagnosis of sinusitis by the histopathologist does not apply to the entire mucosa but only to that part which is sampled. This conclusion is self-evident, but conflicts with the concept of radical surgery that demands complete mucosal clearance. It is also in conflict with any kind of classification of types of sinusitis based on single biopsies (Lund and McKay 1993, Cho et al. 2006).
Nasal and paranasal polyps are a particular manifestation of chronic sinusitis histologically featuring various grades of intercellular edema (Fig. 1.3). Their macroscopic appearance varies between small humps of 2–3 mm diameter and large pedicled mucosal sacs pendulating from the middle turbinate or out of the semilunar hiatus (see Chapter 3). Tos (2000) has given a review of the multiple concepts of their pathogenesis. We are convinced that biomechanical obstruction of the submucous lymph drainage plays a prominent role in the causation of polypous swelling of the mucosa, which may easily occur in the narrow spaces of the ostiomeatal complex in the anterior ethmoids.
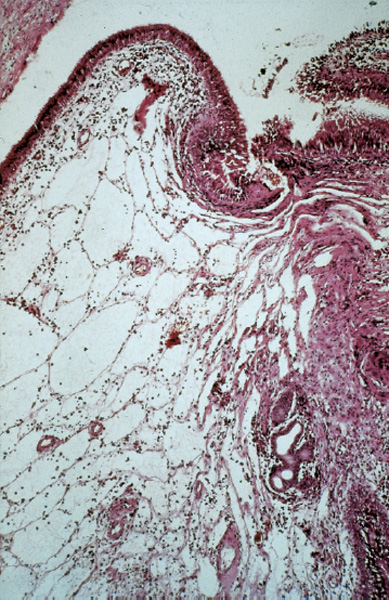
Fig. 1.3 Nasal polyp in a state of development, characterized by extremely wide intercellular spaces filled with edematous fluid (H&E,×63).
In our experience, temporal factors are as important as local factors because histomorphological findings change enormously over time. After a successful tympanoplasty even the most severe mucosal lesions have often regressed when the ear is later reopened after aeration and internal drainage have been restored. A previously very hyperplastic layer will be found to have been replaced by noninflamed, soft mucosa. The same results have now been found many times after surgery for severe sinusitis with mucosal preservation: even previously thick, spongy, injected, and indurated mucosa presents a completely healthy appearance after conservative sinus operations that restore drainage and aeration. Thus, neither the surgeon’s eye nor the results of a frozen tissue section can predict whether inflamed mucosa is capable of resolution.
| At the time of a first operation, the surgeon can by no means predict whether the chronically diseased mucosa will recover or not. |
Mucositis
Little is known of the morphological and functional changes in acute and chronic inflammation of the respiratory mucosa or of the healing processes, either with or without surgery. Numerous histomorphological and structural investigations have been done of the mucosal response pattern, the lymphatic system, and the pathological ciliary activity of the mucosa of humans and animals (e. g., Tos 1978; Hosemann 1985, 1991; Stammberger 1991; Thaler 2002; Benninger 2003), but an overall view of nonspecific mucosal inflammation is not available. The temporal course of the phenomena associated with spread of inflammation from the nasal cavity into the sinuses is not known.
We suspect that an intermediate stage of hyperemia, lymphatic swelling, stasis in the blood and lymphatic pathways, and increased secretion of mucus succeeds an initial stage of hyperemia with reduced mucociliary transport. This is followed either by resolution or by progression to a chronic stage with pathological increase in the elements of the lamina propria such as cells, fibers and ground substance, and resultant permanent disruption of the mucociliary transport and lymphatic drainage. The resulting obstruction of the narrow ducts between the paranasal sinuses and the nasal cavity leads to a vicious cycle of retention of secretions, obstruction of lymphatic drainage, edema, and finally organized connective tissue and mucosal hyperplasia. The causes of local and temporal variations of pathology probably depend on anatomy, the local mucosal response, the infl uence of other body systems, pathogens, and external noxious agents. The etiology of chronic rhinosinusitis (CRS), so far, remains unclear in the majority of cases. The assumption seems justified that an initial acute phase, caused by viral or bacterial infection, precedes chronicity, which is predominantly enhanced by the anatomical factors mentioned. The manifold evidence of a postsurgical reformation of a thick, infiltrated mucosa into a thin, normallooking mucoperiosteum is the strongest argument for the biomechanical hypothesis that an actual pathogenetic anatomical constellation, influencing ventilation, drainage, and subepithelial lymph flow, is the cardinal factor in sustaining the chronicity of lasting mucositis.
Systemic diseases, such as allergy, mucociliary insufficiency syndrome, mucoviscidosis, Kartagener syndrome, ASA-intolerance, etc., may act as important co-factors. Nasal polyposis in patients with ASA-intolerance has a different pattern of leukotriene release and apoptosis of eosinophils (Ziroli 2002), which does not explain its higher recurrence rates.
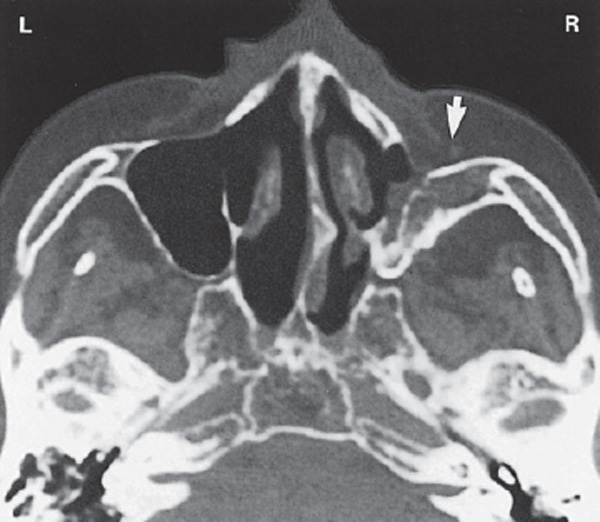
Continuous infection from foreign bodies or from adjacent contaminated areas must also be taken into account. Examples are chronic sinusitis of dental origin due to inflamed dental roots penetrating upward into the antrum or to perforating screws after implantation of dental prostheses or after splinting of facial fractures (Fig. 1.4a, b).
Finally, environmental noxae have been postulated as important. In recent years a particular eosinophilic reaction on fungi in the nasal mucosa (eosinophilic fungalrhinosinusitis, EFR) was emphatically postulated as the origin of nasal polyposis (Ponikau et al. 1999; Lebowitz etal. 2002; Taylor et al. 2002; Stammberger 2003; Lackner et al. 2004). However, Kaschke et al. (2002) could detect only a low incidence (17%) of EFR among their 124 ESSoperated patients with chronic sinusitis.
Tos has presented a fine review of the different hypotheses on the development of polyps (Tos et al. 2000). These cannot, at first glance, convince the endoscopic surgeon who perceives completely healed ethmoids and sphenoid sinuses after ESS with maximal preservation of the diseased mucosa, and who nevertheless detects a typical polyp in the most anterior ethmoid close to the frontoethmoidal transition. If the simple removal of narrow passages in the ethmoid for the restoration of ventilation and drainage is able to normalize a polypous mucosa and in the same patient a remaining isthmus in the anterior ethmoid provides the basis for a recurrent polyposis, it is hard to comprehend that a systemic mucosal pathology should be its main cause. It appears rather obvious that a major causative factor lies in the particular local structure of the bone influencing the homeostasis of the mucosa: pathogenetic anatomy predisposing the normal mucosal reactions to infectious inflammation, e. g. by restricting the lymph drainage, thus provoking edema and polypous swelling.
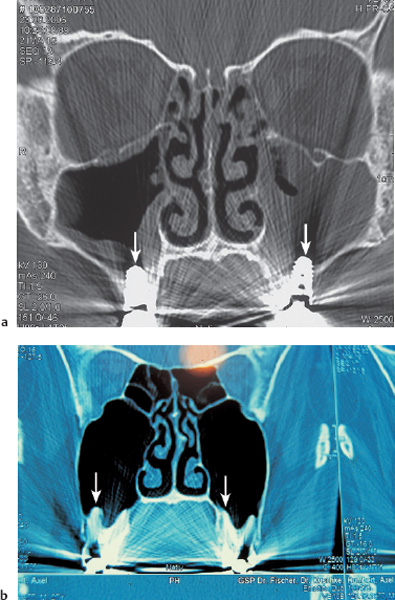
Fig. 1.4 a, b Irritation of the antral mucosa of dental origin.
a Implant screws (arrows) penetrating from the mouth into both maxillary cavities caused chronic sinusitis over the course of 6 months.
b Dental roots (arrows) protruding into the antrum.
The rhinologist diagnosing one or more of these entities will, of course, reconsider a related fl anking therapy, if one exists, but will, finally, indicate endonasal surgery as the royal road to sanitation or relief because this method has also proved successful in syndromes such as allergy and mucoviscidosis.
Polyps, retention cysts (Fig. 1.5), and fistulas do not have a high potential for recovery, so that removal of mucosa should be restricted to these lesions, whereas smooth swellings, cushions of edema, and areas of papillary mucosa can be preserved and given the chance to recover. It is uncertain whether polyps and retention cysts in children heal spontaneously.
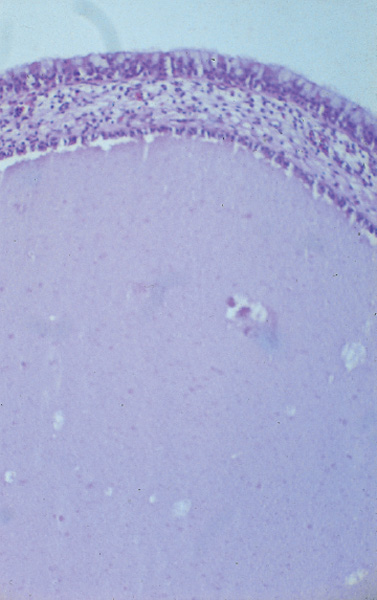
Fig. 1.5 Histological picture of a mucosal retention cyst. Note the respiratory epithelium on its inner surface with an outer epithelial surface rich in goblet cells (H&E,×70).
| In sinusitis, the removal of mucosal lesions that appear to be incapable of resolution is limited to polyps and (pseudo)cysts. Flat edematous swellings and broad-based mucosal cushions can be preserved. The treatment of granulations follows the principles of the treatment of ulcers (see below). |
Doctors and patients often ask whether the chance of healing is reduced by allergy, particularly of the respiratory, immediate type. Basically, it is not: data on this are scarce in the literature, and the conclusion is based on only a proportion of patients because it is impossible to subject large numbers of subjects to complete allergy tests including all possible provocation tests before and after operation.
About 10% of the population, including those with chronic polypoid sinusitis, exhibit an allergic response, and eosinophilia is often found in polyps. These two facts have led to overestimation of the importance of Type I allergy in the genesis and prognosis of nasal polyps. However, tissue eosinophilia is also found in primary nonallergic rhinitis, a disease that is often combined with endogenous asthma and sensitivity to analgesics. Furthermore, the typical immune-reactive elements, such as eosinophils, plasma cells, and immunoglobulin deposits, are so varied (Fig. 1.6a, b) that individual local mucosal responses must be recognized. In vitro experiments after a challenge with allergens showed no difference in the basic histamine release of polyps from allergic and nonallergic subjects (Baenkler et al. 1983, 1987). There is no correlation between the histological and immunohistochemical findings and the clinical and immunological response of patients with severe polypoid sinusitis (Waller et al. 1976). This is borne out by the smooth healing independent of proven allergy. While allergy contributes to the development of CRS (Krause 2003) it does not really exclude surgical therapy.
Whereas antiallergic conservative treatment of patients with nasal polyps can obviously lead to some reduction in size of the polyps (Krause 2003) on account of reduction of the edema, it is not adequate long-term therapy. In the author’s own follow-up investigations after intranasal ethmoid operations, the results of the operation did not depend on respiratory allergy or on treatment by desensitization. Surgery influences the allergic mucosal response favorably by controlling the inflammation, and often leads to complete or at least considerable relief of symptoms. Supplementary measures, for example septal correction, also play a role in this process.
Surgical Principles
Chronic hyperplastic sinusitis typically originates in the ostiomeatal complex of the anterior ethmoids neighboring the semilunar hiatus and the ethmoidal infundibulum. Endoscopy and high-resolution computerized tomography made it obvious that the mucosal changes develop from this primary location and only secondarily invade the peripheral ethmoids and the large cavities (Fig. 1.7). Killian was the first to utilize this knowledge by limiting an intervention against chronic sinusitis to the resection of the uncinate process, thus broadening the ethmoidal infundibulum (Fig. 1.8). Messerklinger has refined this function-orientated “minimal surgery” with the introduction of glass-fiber endoscopes, which became the basis of so-called functional endoscopic sinus surgery (FESS). Its systematic application beyond the ostiomeatal complex established the principle of restoring ventilation and drainage to all paranasal compartments by broadening affected narrow outlets–what we termed “isthmus surgery” (Fig. 1.9a, b) –within the wider definition of endoscopic sinus surgery (ESS) (Wigand 1981). Wherever the mucosal surfaces are brought back into communication with the nasal cavity, their recovery can be expected. ESS reconsiders this rule, and adapts its principles to the topographical pattern of the individual sinusitis case.
The main goal of intranasal endoscopic surgery for chronic sinusitis is the restitution of a normal biological homeostasis in the paranasal pneumatization, including complete recovery of its lining mucosa. For this purpose it postulates two aims: (1) preservation, or at least approximation, of the normal bony superstructure, and (2) preservation of the mucosal texture as much as possible. These aims are basically achieved by the physical restoration of permanent ventilation within the cavities, which is essentially the same as maintaining open ways for the drainage of mucosal fluids by mucociliary activity.
| Functional endoscopic sinus surgery (FESS) means: • Precise reopening of the ethmoidal infundibulum for reventilation of the ostiomeatal complex • Recovery of the paranasal sinus system after limited partial resection of the ethmoid |

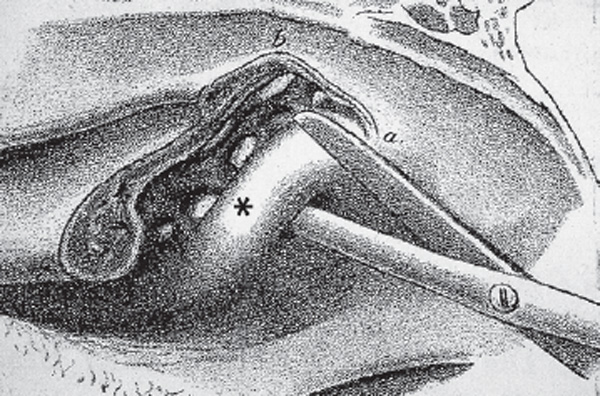
Fig. 1.8 Resection of the uncinate process (*) with the scissors to expose the ethmoid infundibulum (from Killian 1900).
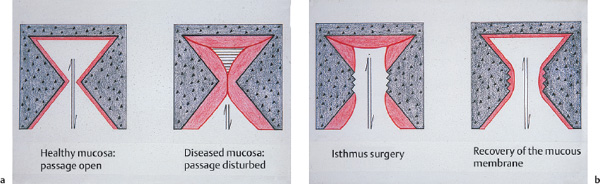
Fig. 1.9 a, b Diagram of the principle of isthmus surgery.
a Vicious circle due to mucosal edema of the antrostomy. The stasis facilitates inflammation and hyperplasia.
b Reventilation and drainage are encouraged by widening of the functionally closed window.
| Endoscopic sinus surgery (ESS) means: • Generalization of endoscopic isthmus surgery • Restoration of ventilation and drainage directed to all affected areas • Preservation of healthy and diseased mucosa by blunt dissection and sharp transection (cutting forceps, electric needle, laser, shaver) • Flanking septal and turbinal surgery |
The first aim is realized by avoiding unnecessary bone removal, limiting this to the broadening of narrow ducts and windows at the large cavities, and to the punching of blocking cell septa in the ethmoid. Only the narrow points are opened up in “isthmus surgery” (Wigand 1981) and a secure communication between the nasal cavity and the paranasal sinuses via the natural channels is reestablished (see Fig. 1.9a, b) . In the maxillary sinus this communication is achieved by creation of a new window in the middle nasal meatus, a recourse to Zuckerkandl 1882. In the frontal sinus the aim is to restore ventilation and drainage via the original frontonasal duct or a channel of adequate width, but without weakening the bone around the frontal infundibulum.
The same concept also applies to the ethmoid and sphenoid sinuses: of necessity many cells must be removed, but not every cell must be denuded or drilled out into every last corner. This attitude is entirely different from the principles of the classical radical sinus surgery in which the mucosa, regarded as irreversibly damaged or as “biologically inferior,” was completely removed, and the bony framework was also widely sacrificed (Fig. 1.10).
ESS conforms to the second postulate by respecting the lining mucosa of walls and cavities. The improved aeration and drainage and supplementary procedures (see below) can confidently be expected to achieve definite resolution of the chronically inflamed mucosa (Fig. 1.11). The entire circumference of ducts and antrostomies must not be completely deprived of mucosa, as this leads to stenosis by circular scarring. If such denudement of the bone is unavoidable, an attempt should be made to pull some cavity mucosa into the bare window (eversion technique, see below). With this goal in mind, the endoscopist will prefer sharp cutting forceps and punches for the limited bone resections in order to avoid unnecessary laceration of the adjacent mucosa; also this contrasts with the older concepts of radical sinus surgery and with contemporary methods of radical exenteration of large cavities with their subsequent obliteration with fat or other materials.
One will perceive a close correspondence of these essentials to the philosophy of modern middle ear surgery (Wigand 1970).
Mucosal continuity of the sinus cavities with each other and with the nose is important to restore mucociliary transport, to prevent granulations arising from denuded bone, and, more importantly, to supplement the abnormal or absent lymphatic drainage. Although this matter has received little attention, the author’s own endoscopic dissections show that the diversion or abnormal function of the lymphatic network can cause serious problems. Even minor manipulations at the ostium or in a duct can lead to long-standing mucosal edema within the sinus, interfering with healing as much as disordered mucociliary transport.
| Intranasal endoscopic operations on the paranasal sinuses for chronic sinusitis are mainly limited to opening the narrow bony points to restore ventilation and internal drainage. |
The recommendation to open narrow areas should not be misinterpreted as an invitation to create large cavities: respect for natural sinus physiology is the guideline running throughout this type of surgery. At the same time, the long-held view that wide nasal cavities automatically carry the danger of drying and atrophy of the mucosa, and even of ozena, must be challenged.
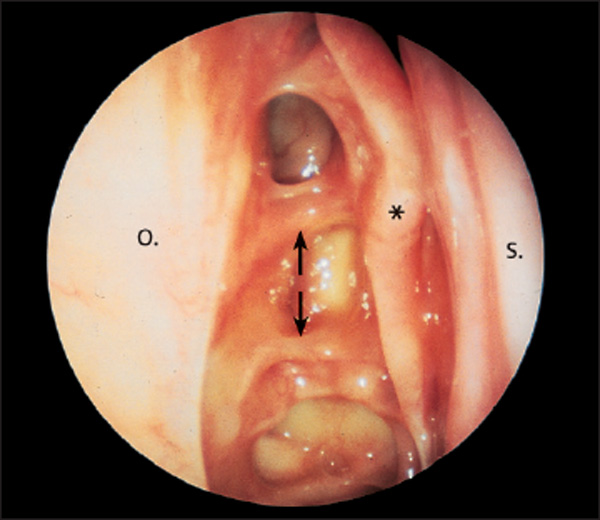
Fig. 1.11 Regeneration of previously polypoid-hyperplastic ethmoid mucosa after endoscopic ethmoidectomy with preservation of the sinus mucosa. The surgically opened areas are healed. The medial lamella (or wall) of the middle turbinate (*) is still present, and the olfactory cleft is normal. Right ethmoid (70° telescope). ↑ = anterior ethmoidal artery. ↓ = posterior ethmoidal artery.
Despite relatively generous septal correction, partial resection of the middle turbinate with complete ethmoidectomy (see below), and limited inferior turbinectomy, we have so far not seen a single case of true ozena after intranasal ethmoidectomy. Although poor aftercare can cause crusting in the ethmoid sinuses, careful removal of the crusts reveals that the underlying mucosa is not dry and atrophic but oversecreting with resultant granulations.
| Enlargement of the nasal cavity by ethmoidectomy, partial turbinectomy, and septum correction does not provoke atrophic rhinitis (ozena). |
With regard to indications other than chronic sinusitis, such as the management of trauma, malformation, and neoplasia, ESS follows the same surgical principles whenever possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


